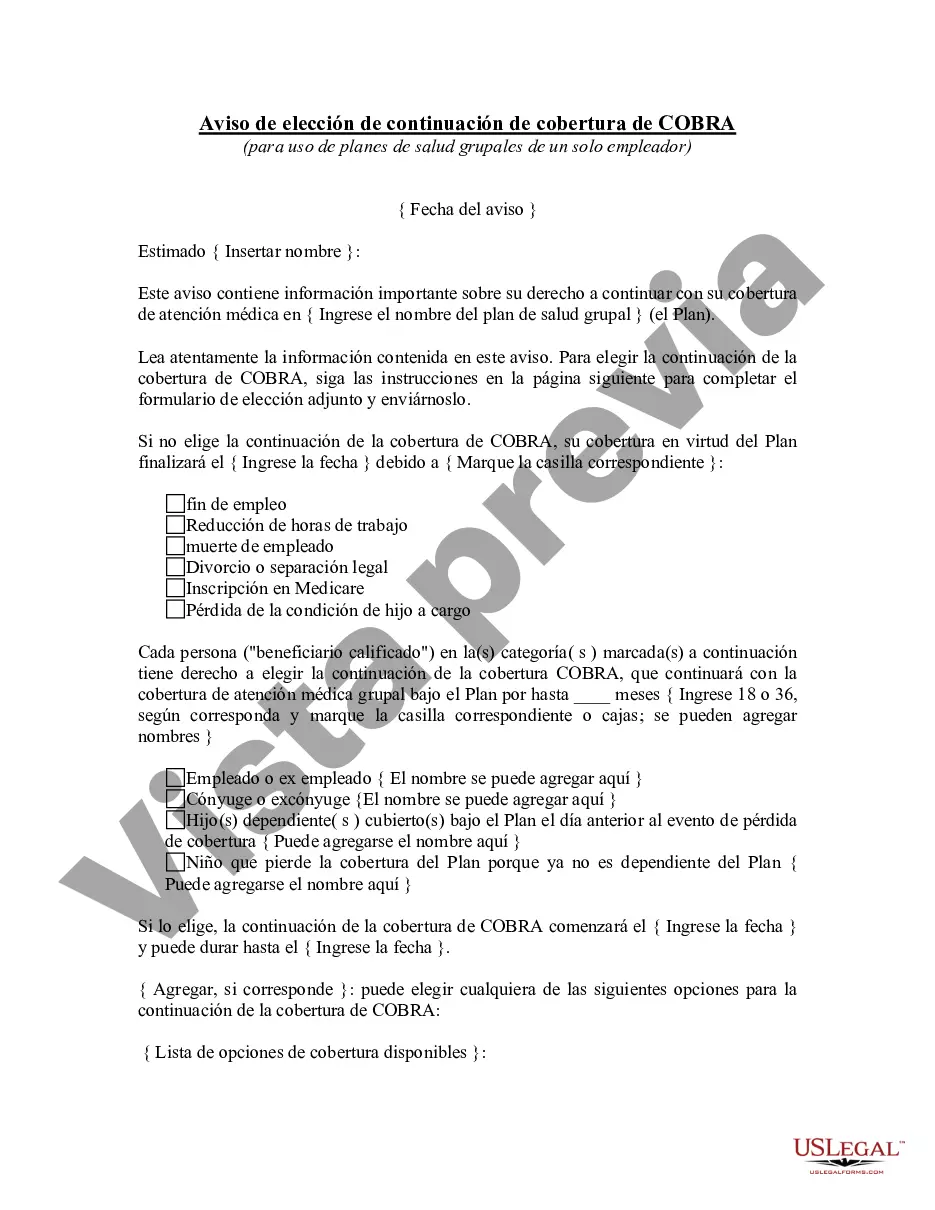
The California COBRA Continuation Coverage Election Notice is a crucial document that helps employees and their dependents understand their rights and options when it comes to continuing their healthcare coverage after experiencing a qualifying event that results in the loss of their insurance. COBRA, or the Consolidated Omnibus Budget Reconciliation Act, requires certain companies to offer continuation coverage to eligible individuals who would otherwise lose their group health insurance benefits. The California COBRA Continuation Coverage Election Notice contains all the necessary information an individual needs to make an informed decision regarding their healthcare coverage. It informs eligible individuals of their ability to continue their group health insurance coverage temporarily, although the premium will typically be higher as the individual will be responsible for paying both the employee and employer portions of the insurance premium. This notice outlines the various conditions that must be met to qualify for continuation coverage, including the types of qualifying events that may trigger the need for coverage such as termination of employment, reduction in work hours, or death of the covered employee. Additionally, it provides crucial information regarding the dates within which individuals must elect continuation coverage, the duration of coverage available, and the procedures for making the election. The California COBRA Continuation Coverage Election Notice also highlights the importance of promptly notifying the employer or benefits administrator of any changes in address or other relevant contact information in order to ensure continuous communication and coverage. While the general concept of the COBRA Continuation Coverage Election Notice remains consistent across California, there may be different variations based on specific circumstances or employer requirements. For instance, some employers may provide a separate notice for employees whose spouses or dependents qualify for continuation coverage due to a divorce or legal separation. Others may offer different continuation options based on the type of qualifying event. It is important for individuals to carefully review the specifics of their notice to understand all available options and requirements. In conclusion, the California COBRA Continuation Coverage Election Notice serves as a crucial communication tool that ensures eligible individuals are informed about their right to continue their healthcare coverage under the COBRA regulations. It provides detailed information regarding qualifying events, coverage duration, premium responsibilities, and election procedures. By carefully reviewing and understanding this notice, individuals can make informed decisions about their healthcare coverage during critical life transitions.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.California Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
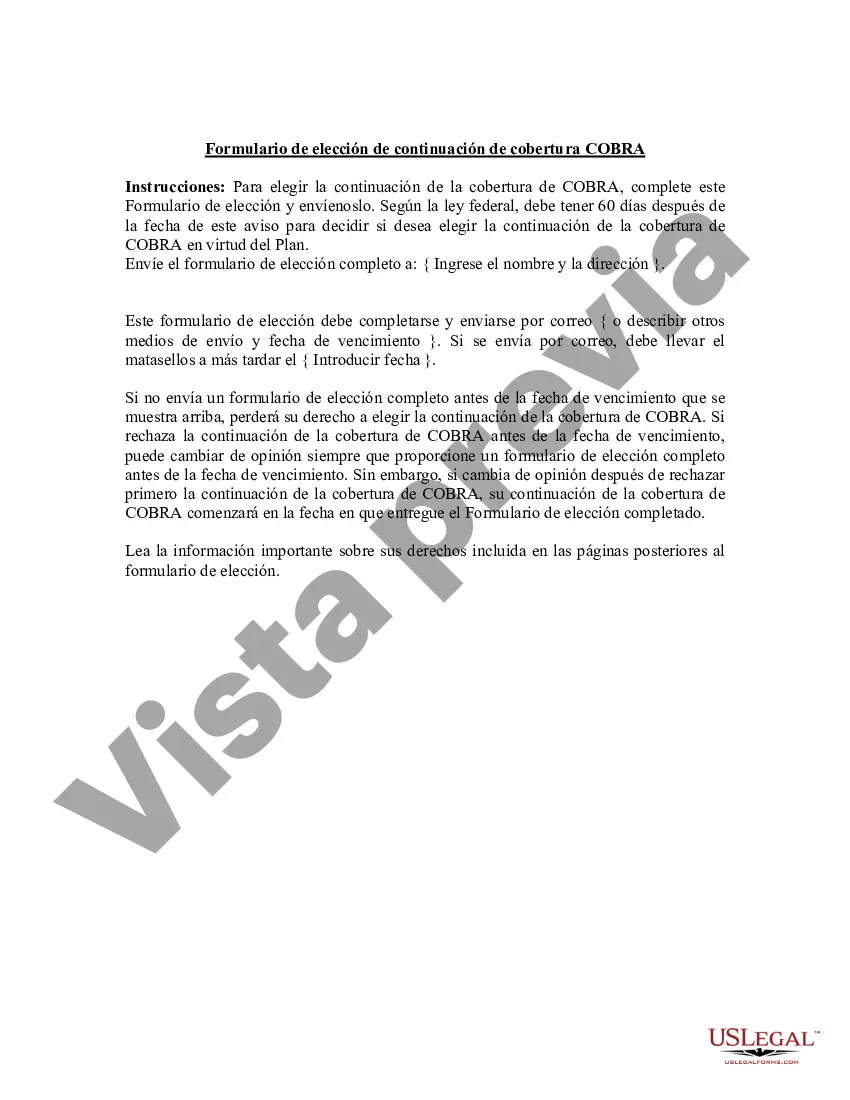
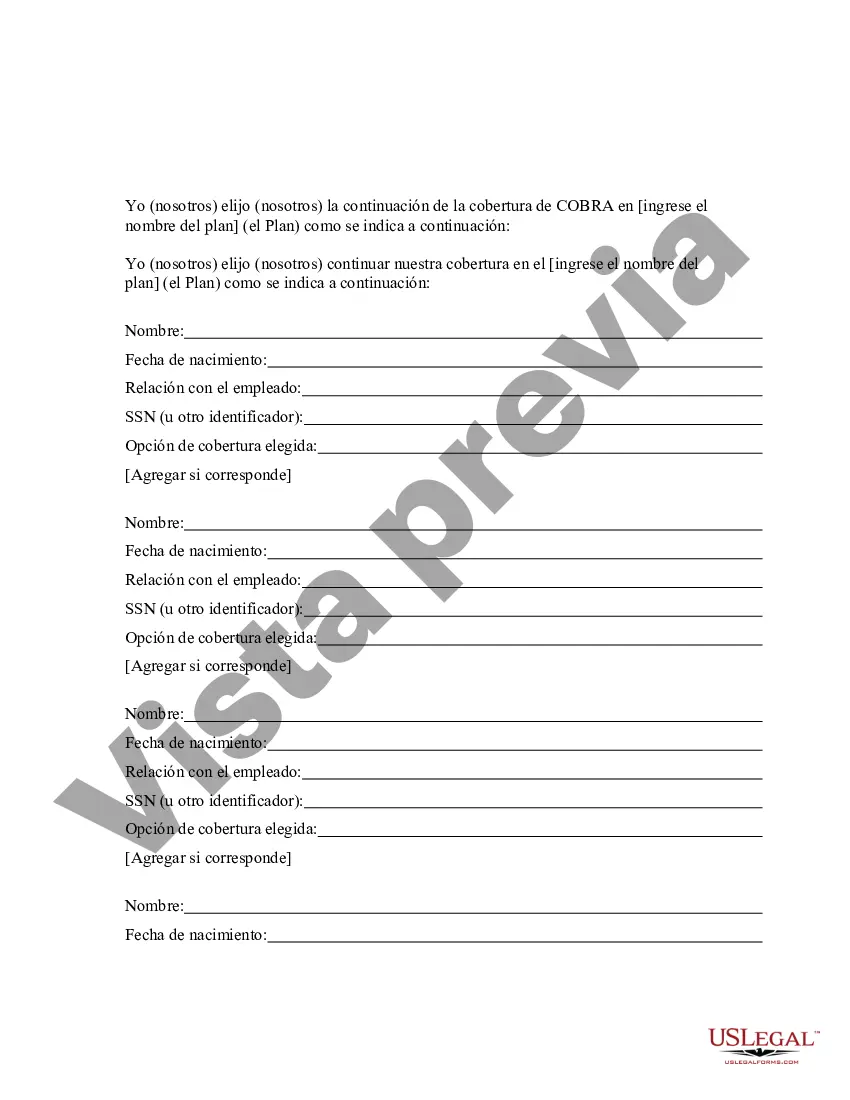
How to fill out California Aviso De Elección De Continuación De Cobertura De COBRA?
Choosing the best authorized papers template could be a have difficulties. Naturally, there are tons of layouts accessible on the Internet, but how can you discover the authorized type you require? Utilize the US Legal Forms internet site. The service offers a large number of layouts, such as the California COBRA Continuation Coverage Election Notice, which can be used for company and personal requires. All of the varieties are checked by specialists and satisfy federal and state needs.
In case you are currently listed, log in to the bank account and click on the Down load key to obtain the California COBRA Continuation Coverage Election Notice. Make use of bank account to check with the authorized varieties you have ordered formerly. Visit the My Forms tab of your own bank account and have another copy of your papers you require.
In case you are a whole new customer of US Legal Forms, listed below are simple directions that you can adhere to:
- Very first, be sure you have selected the correct type for your area/state. You are able to look over the form making use of the Review key and look at the form outline to make sure this is basically the right one for you.
- In the event the type will not satisfy your preferences, take advantage of the Seach industry to find the appropriate type.
- When you are positive that the form is suitable, select the Buy now key to obtain the type.
- Select the rates program you want and enter in the essential information and facts. Design your bank account and buy the transaction with your PayPal bank account or credit card.
- Pick the data file formatting and download the authorized papers template to the device.
- Total, change and print out and signal the received California COBRA Continuation Coverage Election Notice.
US Legal Forms will be the greatest library of authorized varieties that you will find a variety of papers layouts. Utilize the service to download appropriately-made paperwork that adhere to status needs.