Title: Indiana Summary of Rights and Obligations under COBRA: A Comprehensive Guide Keywords: Indiana Summary of Rights and Obligations under COBRA, COBRA benefits, qualified beneficiaries, continuation coverage, COBRA eligibility Introduction: The Indiana Summary of Rights and Obligations under COBRA is an essential resource that outlines key details regarding the Consolidated Omnibus Budget Reconciliation Act (COBRA) and its provisions. COBRA offers continuation coverage for eligible individuals who experience a qualifying event that would otherwise result in the loss of their employer-sponsored health insurance. This article will delve into the various aspects of Indiana's COBRA coverage, its requirements, and the rights and obligations of qualified beneficiaries. 1. Indiana COBRA Eligibility: In Indiana, employees who work for private-sector employers with 20 or more employees are generally eligible for COBRA coverage. Part-time employees might also be eligible under certain circumstances. It is crucial to note that eligible individuals must experience a qualifying event such as termination, reduction in hours, or divorce to be eligible for continuation coverage. 2. Qualifying Events: Indiana COBRA coverage is available for qualified beneficiaries in the event of termination or reduction in work hours, divorce, legal separation, death of the covered employee, or the employee becoming eligible for Medicare. Additionally, dependent children can qualify for COBRA coverage should they lose their dependent status. 3. Notification Requirements: The Indiana Summary of Rights and Obligations under COBRA highlights the importance of timely notification. Employers with group health plans are required to provide eligible employees and their dependents with a written notice explaining COBRA rights and obligations. This notification should be sent within specified timeframes to ensure individuals are aware of their coverage options. 4. Continuation Coverage Duration: Under COBRA, qualified beneficiaries may be entitled to continue their employer-sponsored health insurance for a specific period of time. In Indiana, this duration is typically 18 months for those experiencing termination or reduction in work hours. However, other qualifying events can extend coverage up to 36 months for certain individuals. Specifics regarding duration and coverage options can be found in the Indiana Summary of Rights and Obligations under COBRA. 5. Cost of Coverage: Continuation coverage under COBRA requires individuals to pay the full premium costs, including the share their employer previously covered. In Indiana, qualified beneficiaries can expect to pay the full premium amount, ensuring that the coverage remains uninterrupted. The Indiana Summary of Rights and Obligations under COBRA provides detailed information regarding the cost and payment methods. 6. How to Obtain Indiana COBRA Coverage: If eligible, individuals can elect to receive COBRA continuation coverage by following the instructions provided in the notice received from their employer. The Indiana Summary of Rights and Obligations under COBRA emphasizes the importance of completing the necessary paperwork within the specified timeframe to secure continued coverage. Conclusion: Understanding the Indiana Summary of Rights and Obligations under COBRA is crucial for both employers and employees. This comprehensive guide shines light on the various aspects of COBRA coverage, including eligibility, qualifying events, notification requirements, continuation coverage duration, cost, and the enrollment process. By referring to this resource, individuals can navigate the complexities of COBRA and ensure they receive the necessary health insurance coverage when needed.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Indiana Resumen de derechos y obligaciones bajo COBRA - Summary of Rights and Obligations under COBRA
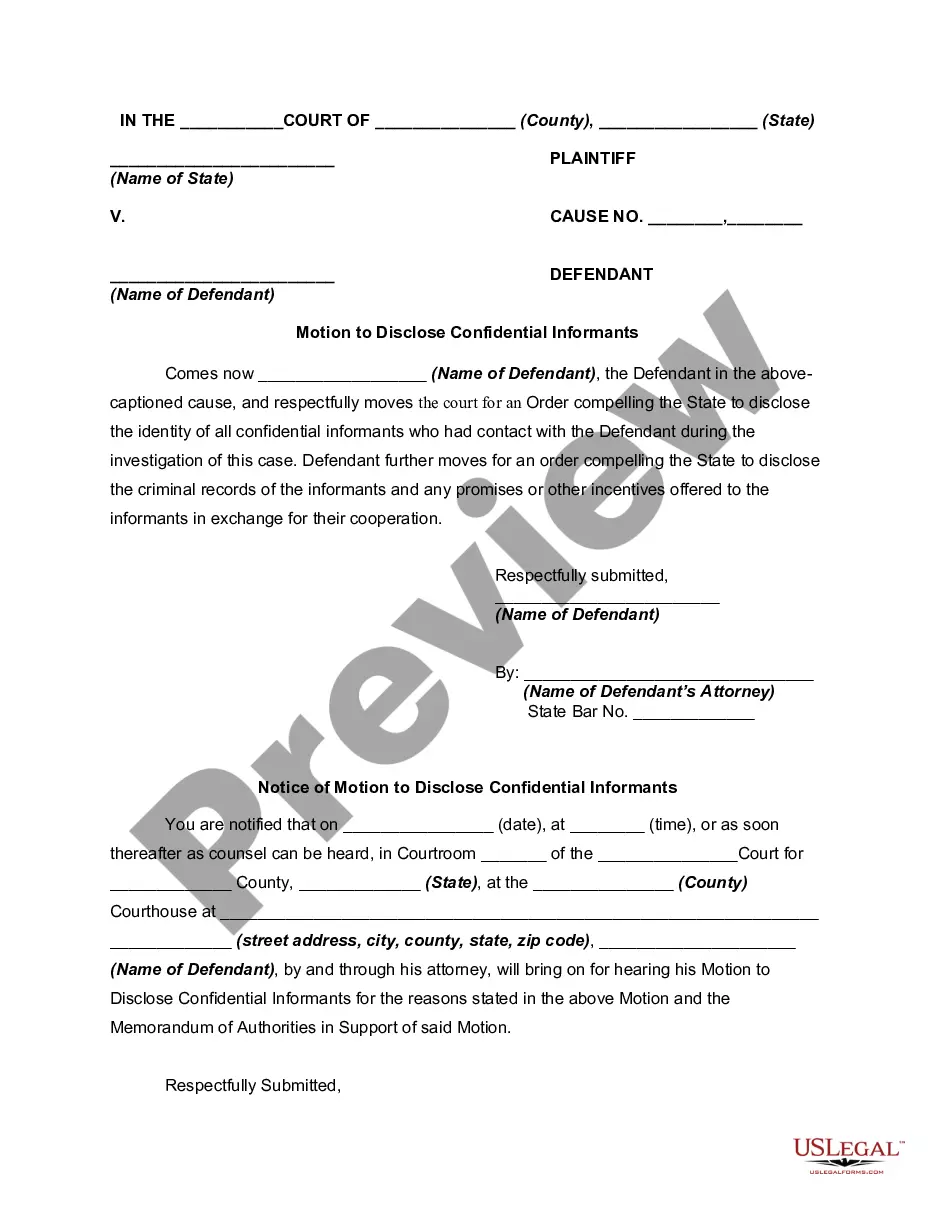
Description
How to fill out Indiana Resumen De Derechos Y Obligaciones Bajo COBRA?
Are you presently within a position the place you will need paperwork for both business or personal reasons nearly every time? There are a variety of legal file themes accessible on the Internet, but finding types you can rely isn`t straightforward. US Legal Forms provides a large number of form themes, such as the Indiana Summary of Rights and Obligations under COBRA, which can be written to satisfy federal and state specifications.
If you are presently informed about US Legal Forms site and get a free account, merely log in. Afterward, you may download the Indiana Summary of Rights and Obligations under COBRA template.
Should you not provide an profile and wish to start using US Legal Forms, abide by these steps:
- Find the form you will need and make sure it is for that correct city/county.
- Take advantage of the Review button to examine the shape.
- See the information to ensure that you have selected the proper form.
- In case the form isn`t what you`re searching for, take advantage of the Research field to find the form that meets your requirements and specifications.
- When you get the correct form, simply click Purchase now.
- Opt for the costs program you would like, submit the desired information to make your account, and purchase an order making use of your PayPal or charge card.
- Choose a convenient paper file format and download your duplicate.
Locate all the file themes you possess purchased in the My Forms menu. You can get a more duplicate of Indiana Summary of Rights and Obligations under COBRA anytime, if required. Just go through the essential form to download or print out the file template.
Use US Legal Forms, probably the most extensive collection of legal kinds, to save lots of efforts and steer clear of mistakes. The support provides professionally made legal file themes that you can use for an array of reasons. Generate a free account on US Legal Forms and begin producing your lifestyle a little easier.