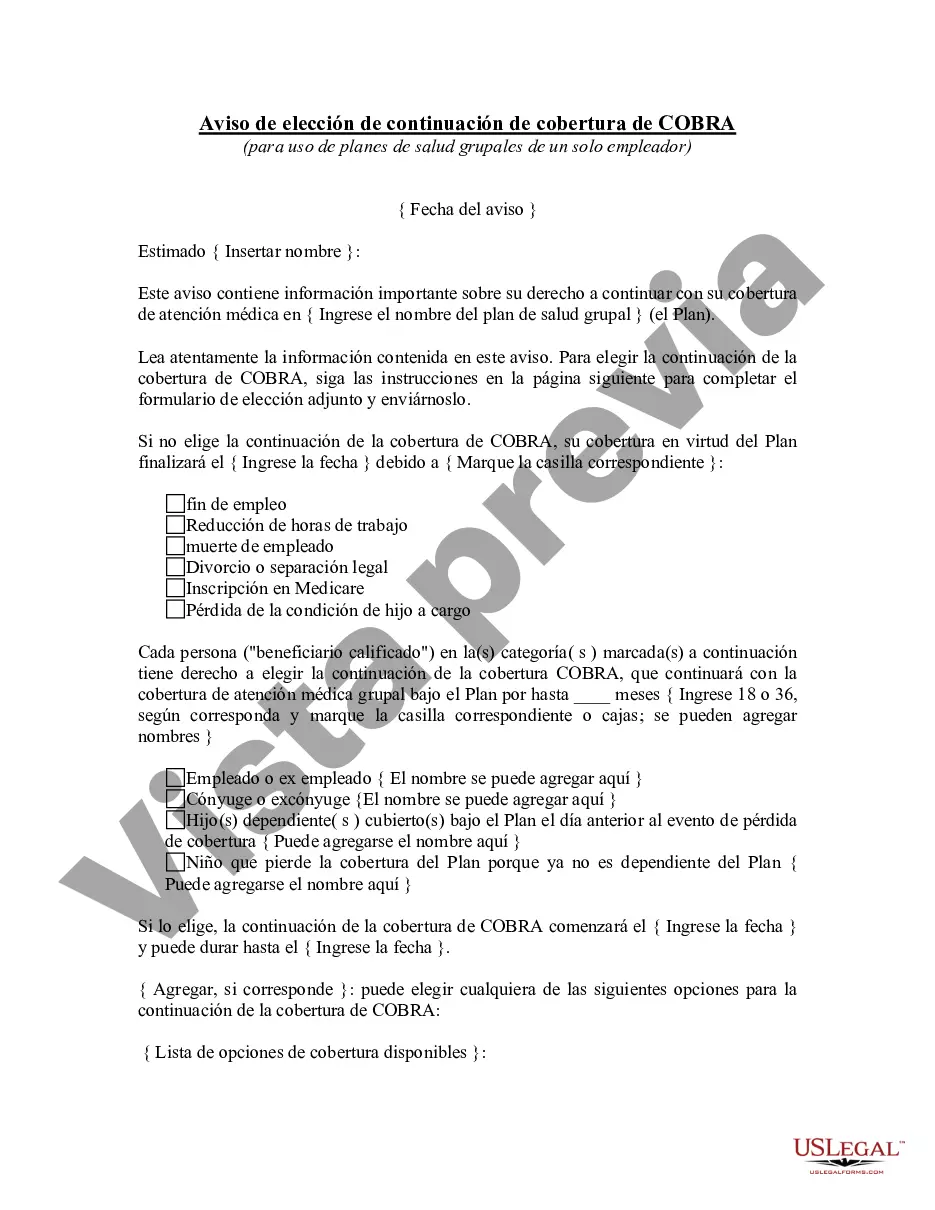
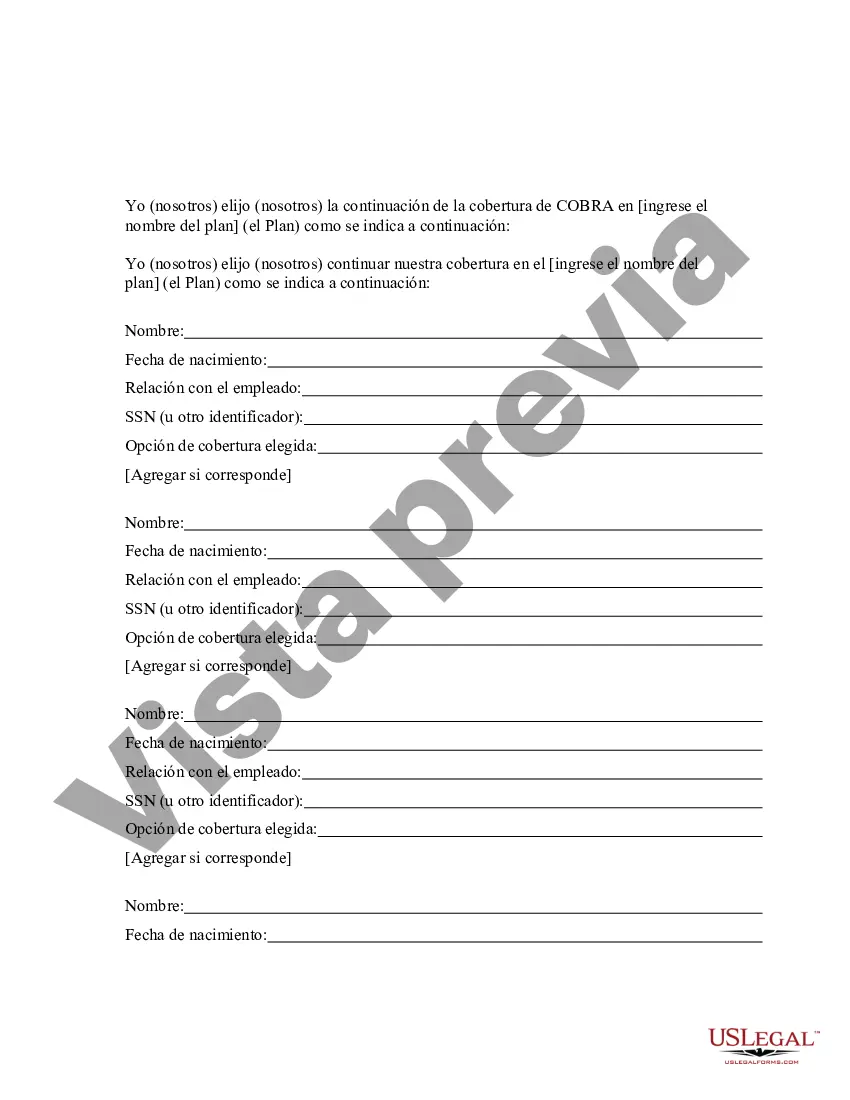
Maine COBRA Continuation Coverage Election Notice is a crucial document sent by employers to employees and their qualified beneficiaries who are entitled to continued health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA) in the state of Maine. This notice provides important information about the rights, options, and deadlines that individuals have in order to elect and maintain their healthcare coverage. The Maine COBRA Continuation Coverage Election Notice outlines the eligibility criteria for COBRA coverage, which includes being enrolled in the employer's health insurance plan at the time of a qualifying event such as job loss, reduction of work hours, or other circumstances that result in loss of coverage. It also specifies the duration of coverage available and the premiums that individuals must pay to continue their health insurance. The notice highlights the procedure for electing COBRA coverage, which typically requires the individual to notify the employer or the designated plan administrator within a specified period (usually 60 days) from the date of the qualifying event. Failure to elect coverage within this timeframe may result in permanent loss of the option to obtain COBRA continuation coverage. In some cases, there may be different types of Maine COBRA Continuation Coverage Election Notices, depending on the specific circumstances of the qualifying event. For instance, there could be notices for employees who have lost their jobs, separate notices for employees whose work hours have been reduced, or notices for employees who have become eligible for Medicare while still being covered under their employer's plan. Each notice would contain instructions and information tailored to the particular situation. Keywords: Maine, COBRA Continuation Coverage Election Notice, employers, employees, qualified beneficiaries, health insurance coverage, Consolidated Omnibus Budget Reconciliation Act, COBRA, rights, options, deadlines, elect, healthcare coverage, eligibility criteria, qualifying event, job loss, reduction of work hours, lost coverage, duration of coverage, premiums, electing COBRA coverage, procedure, plan administrator, failure to elect coverage, permanent loss, notice types, circumstances, specific situation, instructions, information.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Maine Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
How to fill out Maine Aviso De Elección De Continuación De Cobertura De COBRA?
Choosing the right legitimate document web template can be a battle. Of course, there are tons of layouts available on the Internet, but how can you obtain the legitimate type you want? Take advantage of the US Legal Forms internet site. The assistance provides thousands of layouts, like the Maine COBRA Continuation Coverage Election Notice, which can be used for organization and personal needs. Every one of the varieties are examined by experts and fulfill federal and state demands.
When you are currently authorized, log in to your profile and then click the Download switch to have the Maine COBRA Continuation Coverage Election Notice. Make use of your profile to search from the legitimate varieties you might have bought earlier. Check out the My Forms tab of the profile and get yet another version of your document you want.
When you are a fresh end user of US Legal Forms, allow me to share straightforward directions for you to adhere to:
- Very first, make certain you have chosen the proper type for the area/region. You are able to check out the form using the Preview switch and look at the form outline to make sure this is basically the best for you.
- In the event the type does not fulfill your expectations, utilize the Seach discipline to find the appropriate type.
- When you are sure that the form is suitable, go through the Acquire now switch to have the type.
- Choose the pricing program you need and enter in the necessary info. Build your profile and pay for an order using your PayPal profile or credit card.
- Select the submit structure and download the legitimate document web template to your device.
- Total, modify and printing and signal the obtained Maine COBRA Continuation Coverage Election Notice.
US Legal Forms is definitely the largest catalogue of legitimate varieties where you can discover a variety of document layouts. Take advantage of the service to download skillfully-made documents that adhere to state demands.