- US Legal Forms
-
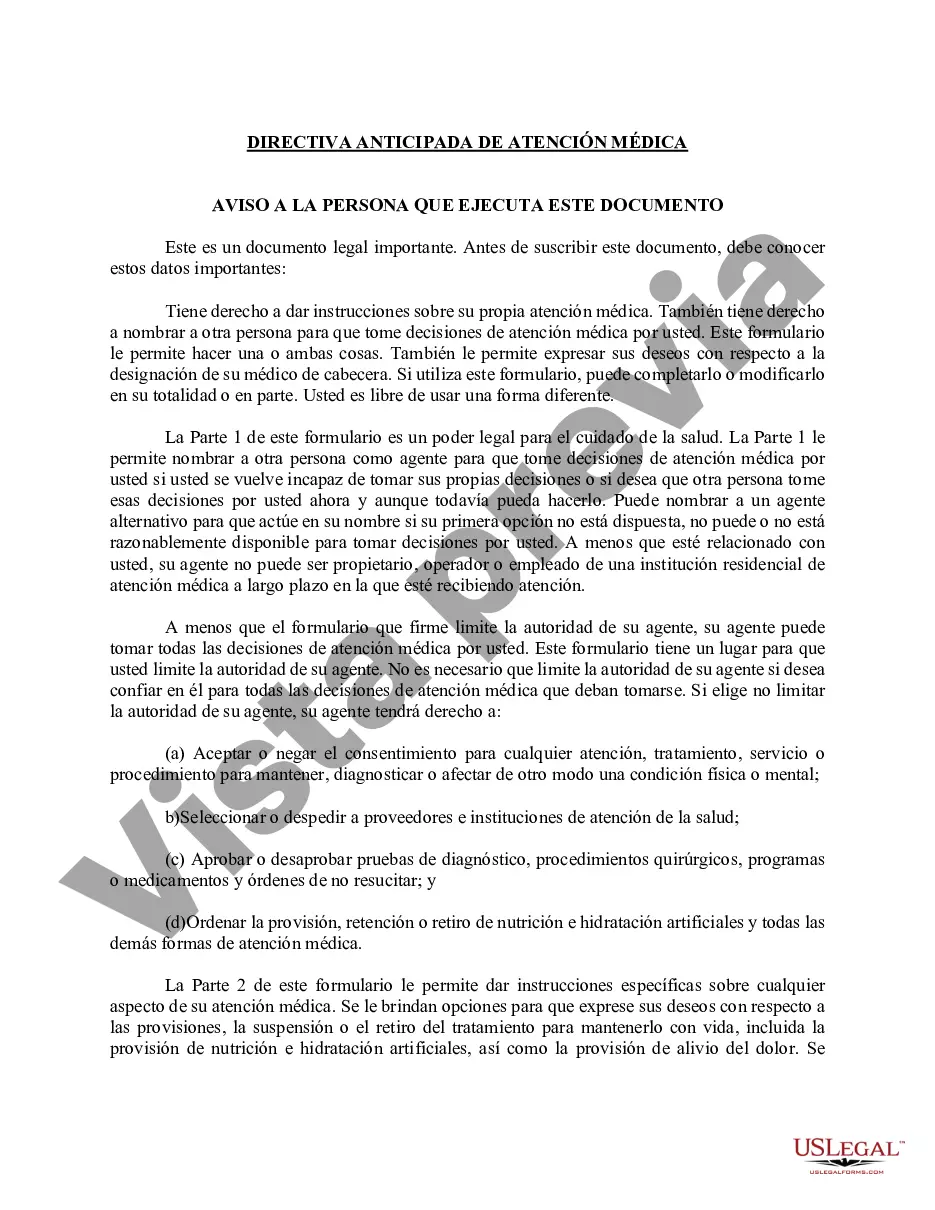
Mississippi Directiva anticipada de atención médica
Mississippi Directiva anticipada de atención médica - Mississippi Advance Healthcare Directive
Description
Viewed forms
How to fill out Mississippi Directiva Anticipada De Atención Médica?
Obtain a printable Mississippi Advance Healthcare Directive in only several mouse clicks in the most extensive catalogue of legal e-forms. Find, download and print out professionally drafted and certified samples on the US Legal Forms website. US Legal Forms is the Top provider of reasonably priced legal and tax templates for US citizens and residents on-line since 1997.
Users who have a subscription, need to log in into their US Legal Forms account, get the Mississippi Advance Healthcare Directive see it saved in the My Forms tab. Users who do not have a subscription are required to follow the steps below:
- Make sure your form meets your state’s requirements.
- If provided, look through form’s description to learn more.
- If available, review the shape to see more content.
- When you are sure the template is right for you, simply click Buy Now.
- Create a personal account.
- Choose a plan.
- through PayPal or credit card.
- Download the form in Word or PDF format.
When you’ve downloaded your Mississippi Advance Healthcare Directive, you are able to fill it out in any web-based editor or print it out and complete it by hand. Use US Legal Forms to get access to 85,000 professionally-drafted, state-specific forms.
Power of Attorney and Living Will / Health Care Directive
Take advantage of personalized templates with US Legal Forms. Complete a simple survey to describe your case and get the appropriate Power of Attorney for your state and situation.
Form Rating
Form popularity
FAQ
Un directiva por anticipado es un documento legal en el que se estipulan como se aplicarA¡n las decisiones de su atenciA³n mA©dica en funciA³n de lo que usted desee a partir del momento en que no pueda tomar decisiones.
Seguros estamos que te interesa, te mencionamos sus ramas para que las tomes en consideracion a la hora de escoger esta carrera.EnfermerAa de salud mental.EnfermerAa geriA¡trica.EnfermerAa de cuidados mA©dicos quirAºrgico.EnfermerAa familiar.EnfermerAa en Obstetricia.EnfermerAa en PediatrAa.
La planificacion anticipada para los cuidados de salud implica conocer los tipos de decisiones que podrAan ser necesarios tomar, considerar estas decisiones con anticipaciA³n y luego informar a otras personastanto a su familia como a sus proveedores de atenciA³n mA©dicaacerca de sus preferencias.
Servicios de salud que abarcan la prevencion, el bienestar y el tratamiento de enfermedades comunes. Los proveedores de servicios de salud primarios incluyen mA©dicos, enfermeros practicantes y asistentes mA©dicos. TambiA©n pueden coordinar sus cuidados de salud con especialistas.
Una planificacion estratA©gica de salud es un sistema que busca ordenar acciones en los centros de salud, hospitales pAºblicos, privados o clAnicas para establecer objetivos relacionados con mejoras en procesos de servicio u optimizaciA³n de recursos mA©dicos.
El cuidado preventivo ayuda a detectar o prevenir enfermedades graves y problemas de salud antes de que empeoren. Algunos ejemplos de cuidado preventivo son los chequeos anuales, inmunizaciones y vacunas antigripales, y ciertas pruebas y examenes mA©dicos. Esto tambiA©n se conoce como cuidado de rutina.
La meta del cuidado medico de apoyo es prevenir o tratar lo antes posible los sAntomas de una enfermedad, los efectos secundarios del tratamiento y los problemas psicolA³gicos, sociales y espirituales relacionados con una enfermedad o su tratamiento.
La meta del cuidado medico de apoyo es prevenir o tratar lo antes posible los sAntomas de una enfermedad, los efectos secundarios del tratamiento y los problemas psicolA³gicos, sociales y espirituales relacionados con una enfermedad o su tratamiento.
La planificacion anticipada de la atenciA³n mA©dica es el proceso mediante el cual se decide la atenciA³n mA©dica que se recibirA¡ en el futuro. Ayuda a garantizar que pueda cumplirse su voluntad si no puede expresar sus propios deseos.
Mississippi Directiva anticipada de atención médica Related Searches
-
directiva anticipada en ingles
-
texas poa form
-
texas most form pdf
-
https hhs texas gov laws regulations forms
-
texas advance directives
More info
Trusted and secure by over 3 million people of the world’s leading companies
Living Wills - General - Mississippi
Related Mississippi Legal Forms
(a) "Adult" means an individual who is eighteen (18) years of age or older. (b) "Advance health-care directive" means an individual instruction or a power of attorney for health care. (c) "Agent" means an individual designated in a power of attorney for health care to make a health-care decision for the individual granting the power. (d) "Capacity" means an individual's ability to understand the significant benefits, risks, and alternatives to proposed health care and to make and communicate a health-care decision. (e) "Emancipated minor" means an individual under the age of eighteen (18) years who:Section 41-41-205: Individual instructions; power of attorney; decisions by primary physician; agents; guardians; validity.(i) Is or has been married; (ii) Has been adjudicated generally emancipated by a court of competent jurisdiction; or (iii) Has been adjudicated emancipated for the purpose of making health-care decisions by a court of competent jurisdiction.(f) "Guardian" means a judicially appointed guardian or conservator having authority to make a health-care decision for an individual. (g) "Health care" means any care, treatment, service, or procedure to maintain,diagnose, or otherwise affect an individual's physical or mental condition. (h) "Health-care decision" means a decision made by an individual or the individual's agent, guardian, or surrogate, regarding the individual's health care,including:(i) Selection and discharge of health-care providers and institutions; (ii) Approval or disapproval of diagnostic tests, surgical procedures, programs of medication, and orders not to resuscitate; and (iii) Directions to provide, withhold or withdraw artificial nutrition and hydration and all other forms of health care.The phrase "health-care decision" does not include decisions made pursuant to Sections 41-39-31 through 41-39-51, the "Anatomical Gift Law." (i) "Health-care institution" means an institution, facility, or agency licensed, certified, or otherwise authorized or permitted by law to provide health care in the ordinary course of business. (j) "Health-care provider" means an individual licensed, certified, or otherwise authorized or permitted by law to provide health care in the ordinary course of business or practice of a profession. (k) "Individual instruction" means an individual's direction concerning a health-care decision for the individual. (l) "Person" means an individual, corporation, business trust, estate, trust,partnership, association, joint venture, government, governmental subdivision, agency, or instrumentality, or any other legal or commercial entity. (m) "Physician" means an individual authorized to practice medicine or osteopathy under Title 73, Chapter 25, Mississippi Code of 1972. (n) "Power of attorney for health care" means the designation of an agent to make health-care decisions for the individual granting the power. (o) "Primary physician" means a physician designated by an individual or the individual's agent, guardian, or surrogate, to have primary responsibility for the individual's health care or, in the absence of a designation or if the designated physician is not reasonably available, a physician who undertakes the responsibility. (p) "Reasonably available" means readily able to be contacted without undue effort and willing and able to act in a timely manner considering the urgency of the patient's health-care needs. (q) "State" means a state of the United States, the District of Columbia, the Commonwealth of Puerto Rico, or a territory or insular possession subject to the jurisdiction of the United States. (r) "Supervising health-care provider" means the primary physician or, if there is no primary physician or the primary physician is not reasonably available,the health-care provider who has undertaken primary responsibility for an individual's health care. (s) "Surrogate" means an individual, other than a patient's agent or guardian, authorized under Sections 41-41-201 through 41-41-229 to make a health-care decision for the patient.
(1) An adult or emancipated minor may give an individual instruction. The instruction may be oral or written. The instruction may be limited to take effect only if a specified condition arises. (2) An adult or emancipated minor may execute a power of attorney for health care, which may authorize the agent to make any health-care decision the principal could have made while having capacity. The power remains in effect notwithstanding the principal's later incapacity and may include individual instructions. Unless related to the principal by blood, marriage, or adoption, an agent may not be an owner, operator, or employee of a residential long-term health-care institution at which the principal is receiving care. The power must be in writing, contain the date of its execution, be signed by the principal, and be witnessed by one (1) of the following methods:Section 41-41-207:(a) Be signed by at least two (2) individuals each of whom witnessed either the signing of the instrument by the principal or the principal's acknowledgement of the signature or of the instrument. See Form.(3) None of the following may be used as witness for a power of attorney for health care:(a) A health-care provider; (b) An employee of a health-care provider or facility; or (c) The agent.(4) At least one (1) of the individuals used as a witness for a power of attorney for health care shall be someone who is neither:(a) A relative of the principal by blood, marriage or adoption; nor (b) An individual who would be entitled to any portion of the estate of the principal upon his or her death under any will or codicil thereto of the principal existing at the time of execution of the power of attorney for health care or by operation of law then existing.(5) Unless otherwise specified in a power of attorney for health care, the authority of an agent becomes effective only upon a determination that the principal lacks capacity, and ceases to be effective upon a determination that the principal has recovered capacity. (6) Unless otherwise specified in a written advance health-care directive, a determination that an individual lacks or has recovered capacity, or that another condition exists that affects an individual instruction or the authority of an agent, must be made by the primary physician. (7) An agent shall make a health-care decision in accordance with the principal's individual instructions, if any, and other wishes to the extent known to the agent. Otherwise, the agent shall make the decision in accordance with the agent's determination of the principal's best interest. In determining the principal's best interest, the agent shall consider the principal's personal values to the extent known to the agent. (8) A health-care decision made by an agent for a principal is effective without judicial approval. (9) A written advance health-care directive may include the individual's nomination of a guardian of the person. (10) An advance health-care directive is valid for purposes of Sections 41-41-201 through 41-41-229 if it complies with Sections 41-41-201 through 41-41-229, regardless of when or where executed or communicated.
(1) An individual may revoke the designation of an agent only by a signed writing or by personally informing the supervising health-care provider. (2) An individual may revoke all or part of an advance health-care directive,other than the designation of an agent, at any time and in any manner that communicates an intent to revoke. (3) A health-care provider, agent, guardian, or surrogate who is informed of a revocation shall promptly communicate the fact of the revocation to the supervising health-care provider and to any health-care institution at which the patient is receiving care. (4) A decree of annulment, divorce, dissolution of marriage, or legal separation revokes a previous designation of a spouse as agent unless otherwise specified in the decree or in a power of attorney for health care. (5) An advance health-care directive that conflicts with an earlier advance health-care directive revokes the earlier directive to the extent of the conflict.Section 41-41-209: The following form may be used to create an advance health-care directive. Sections 41-41-201 through 41-41-207 and 41-41-211 through 41-41-229 govern the effect of this or any other writing used to create an advanced health-care directive. Section 41-41-211:
(1) A surrogate may make a health-care decision for a patient who is an adult or emancipated minor if the patient has been determined by the primary physician to lack capacity and no agent or guardian has been appointed or the agent or guardian is not reasonably available. (2) An adult or emancipated minor may designate any individual to act as surrogate by personally informing the supervising health-care provider. In the absence of a designation, or if the designee is not reasonably available, any member of the following classes of the patient's family who is reasonably available, in descending order of priority, may act as surrogate:Section 41-41-213:(a) The spouse, unless legally separated; (b) An adult child; (c) A parent; or (d) An adult brother or sister.(3) If none of the individuals eligible to act as surrogate under subsection (2) is reasonably available, an adult who has exhibited special care and concernfor the patient, who is familiar with the patient's personal values, and who is reasonably available may act as surrogate. (4) A surrogate shall communicate his or her assumption of authority as promptly as practicable to the members of the patient's family specified in subsection (2) who can be readily contacted. (5) If more than one (1) member of a class assumes authority to act as surrogate, and they do not agree on a health-care decision and the supervising health-care provider is so informed, the supervising health-care provider shall comply with the decision of a majority of the members of that class who have communicated their views to the provider. If the class is evenly divided concerning the health-care decision and the supervising health-care provider is so informed, that class and all individuals having lower priority are disqualified from making the decision. (6) A surrogate shall make a health-care decision in accordance with the patient's individual instructions, if any,and other wishes to the extent known to the surrogate. Otherwise, the surrogate shall make the decision in accordance with the surrogate's determination of the patient's best interest. In determining the patient's best interest, the surrogate shall consider the patient's personal values to the extent known to the surrogate. (7) A health-care decision made by a surrogate for a patient is effective without judicial approval. (8) An individual at any time may disqualify another, including a member of the individual's family, from acting as the individual's surrogate by a signed writing or by personally informing the supervising health-care provider of the disqualification. (9) A surrogate may not be an owner, operator, or employee of a residential long-term health-care institution at which the patient is receiving care unless related to the patient by blood, marriage, or adoption, except in the case of a patient of a state-operated facility who has no person listed in subsection (2) reasonably available to act as a surrogate. (10) A supervising health-care provider may require an individual claiming the right to act as surrogate for a patient to provide a written declaration under penalty of perjury stating facts and circumstances reasonably sufficient to establish the claimed authority.
(1) A guardian shall comply with the ward's individual instructions and may not revoke the ward's advance health-care directive unless the appointing court expressly so authorizes. (2) Absent a court order to the contrary, a health-care decision of an agent takes precedence over that of a guardian. (3) A health-care decision made by a guardian for the ward is effective without judicial approval.Section 41-41-215:
(1) Before implementing a health-care decision made for a patient, a supervising health-care provider, if possible, shall promptly communicate to the patient the decision made and the identity of the person making the decision. (2) A supervising health-care provider who knows of the existence of an advance health-care directive, a revocation of an advance health-care directive, or a designation or disqualification of a surrogate, shall promptly record its existence in the patient's health-care record and, if it is in writing, shall request a copy and if one is furnished shall arrange for its maintenance in the health-care record. (3) A primary physician who makes or is informed of a determination that a patient lacks or has recovered capacity, or that another condition exists which affects an individual instruction or the authority of an agent, guardian, or surrogate, shall promptly record the determination in the patient's health-care record and communicate the determination to the patient, if possible, and to any person then authorized to make health-care decisions for the patient. (4) Except as provided in subsections (5) and (6), a health-care provider or institution providing care to a patient shall:Section 41-41-217: Unless otherwise specified in an advance health-care directive, a person then authorized to make health-care decisions for a patient has the same rights as the patient to request, receive, examine, copy and consent to the disclosure of medical or any other health-care information. Section 41-41-219:(a) Comply with an individual instruction of the patient and with a reasonable interpretation of that instruction made by a person then authorized to make health-care decisions for the patient; and (b) Comply with a health-care decision for the patient made by a person then authorized to make health-care decisions for the patient to the same extent as if the decision had been made by the patient while having capacity.(5) A health-care provider may decline to comply with an individual instruction or health-care decision for reasons of conscience. A health-care institution may decline to comply with an individual instruction or health-care decision if the instruction or decision is contrary to a policy of the institution which is expressly based on reasons of conscience and if the policy was timely communicated to the patient or to a person then authorized to make health-care decisions for the patient. (6) A health-care provider or institution may decline to comply with an individual instruction or health-care decision that requires medically ineffective health care or health care contrary to generally accepted health-care standards applicable to the health-care provider or institution. (7) A health-care provider or institution that declines to comply with an individual instruction or health-care decision shall:(a) Promptly so inform the patient, if possible, and any person then authorized to make health-care decisions for the patient; (b) Provide continuing care to the patient until a transfer can be effected; and (c) Unless the patient or person then authorized to make health-care decisions for the patient refuses assistance, immediately make all reasonable efforts to assist in the transfer of the patient to another health-care provider or institution that is willing to comply with the instruction or decision.(8) A health-care provider or institution may not require or prohibit the execution or revocation of an advance health-care directive as a condition for providing health care. (9) If the patient who is an adult or emancipated minor has been determined by the primary physician to lack capacity to make a health-care decision and an agent, guardian or surrogate is not reasonably available, consent may be given by an owner, operator or employee of a residential long-term health care institution at which the patient is a resident if there is no advance health-care directive to the contrary and a licensed physician who is not an owner, operator or employee of the residential long-term health care institution at which the patient is a resident has determined that the patient is in need of health care. This power to consent is limited to the terms of this subsection (9) and shall not be construed to repeal or otherwise affect the prohibition of Section 41-41-211 (9) relating to owners, operators, or employees of long-term health care institutions. The consent given pursuant to this subsection shall be limited to the health care services determined necessary by the licensed physician and shall in no event include the power to consent to or direct withholding or discontinuing any life support, nutrition, hydration or other treatment, care or support. When consent is obtained under this subsection, compliance with these requirements shall be stated in the patient's health-care record.
(1) A health-care provider or institution acting in good faith and in accordance with generally accepted health-care standards applicabl to the health-care provider or institution is not subject to civil or criminal liability or to discipline for unprofessional conduct for:Section 41-41-221:(a) Complying with a health-care decision of a person apparently having authority to make a health-care decision for a patient, including a decision to withhold or withdraw health care; (b) Declining to comply with a health-care decision of a person based on a belief that the person then lacked authority; or (c) Complying with an advance health-care directive and assuming that the directive was valid when made and has not been revoked or terminated.(2) An individual acting as agent or surrogate under Sections 41-41-201 through 41-41-229 is not subject to civil or criminal liability or to discipline for unprofessional conduct for health-care decisions made in good faith.
(1) A health-care provider or institution that intentionally violates Sections 41-41-201 through 41-41-229 is subject to liability to the aggrieved individual for damages of Five Hundred Dollars ($500.00) or actual damages resulting from the violation, whichever is greater, plus reasonable attorney's fees. (2) A person who intentionally falsifies, forges, conceals, defaces, or obliterates an individual's advance health-care directive or a revocation of an advance health-care directive without the individual's consent, or who coerces or fraudulently induces an individual to give, revoke, or not to give an advance health-care directive, is subject to liability to that individual for damages of Twenty-five Hundred Dollars ($2,500.00) or actual damages resulting from the action, whichever is greater, plus reasonable attorney's fees.Section 41-41-223:
(1) Sections 41-41-201 through 41-41-229 do not affect the right of an individual to make health-care decisions while having capacity to do so. (2) An individual is presumed to have capacity to make a health-care decision, to give or revoke an advance health-care directive, and to designate or disqualify a surrogate.Section 41-41-225: A copy of a written advance health-care directive, revocation of an advance health-care directive, or designation or disqualification of a surrogate has the same effect as the original. Section 41-41-227:
(1) Sections 41-41-201 through 41-41-229 do not create a presumption concerning the intention of an individual who has not made or who has revoked an advance health-care directive. (2) Death resulting from the withholding or withdrawal of health care in accordance with Sections 41-41-201 through 41-41-229 does not for any purpose constitute a suicide or homicide or legally impair or invalidate a policy of insurance or an annuity providing a death benefit, notwithstanding any term of the policy or annuity to the contrary. (3) Sections 41-41-201 through 41-41-229 do not authorize mercy killing, assisted suicide, euthanasia, or the provision, withholding, or withdrawal of health care, to the extent prohibited by other statutes of this state. (4) Sections 41-41-201 through 41-41-229 do not authorize or require a health-care provider or institution to provide health care contrary to generally accepted health-care standards applicable to the health-care provider or institution. (5) Sections 41-41-201 through 41-41-229 do not authorize an agent or surrogate to consent to the admission of an individual to a mental health-care institution unless the individual's written advance health-care directive expressly so provides. (6) Sections 41-41-201 through 41-41-229 do not affect other statutes of this state governing treatment for mental illness of an individual involuntarily committed to a mental health-care institution. (7) Sections 41-41-201 through 41-41-229 do not apply to Sections 41-41-31 through 41-41-39, which govern the performance of abortions, or Sections 41-41-51 through 41-41-63, which govern the performance of abortions upon minors.Section 41-41-229: On petition of a patient, the patient's agent, guardian, or surrogate, a health-care provider or institution involved with the patient's care, or an individual described in Section 41-41-211(2) or (3), any court of competent jurisdiction may enjoin or direct a health-care decision or order other equitable relief. A proceeding under this section shall be governe by the Mississippi Rules of Civil Procedure. Note: All Information and Previews are subject to the Disclaimer located on the main forms page, and also linked at the bottom of all search results.
Living Wills - General - Mississippi
Related Mississippi Legal Forms
(a) "Adult" means an individual who is eighteen (18) years of age or older. (b) "Advance health-care directive" means an individual instruction or a power of attorney for health care. (c) "Agent" means an individual designated in a power of attorney for health care to make a health-care decision for the individual granting the power. (d) "Capacity" means an individual's ability to understand the significant benefits, risks, and alternatives to proposed health care and to make and communicate a health-care decision. (e) "Emancipated minor" means an individual under the age of eighteen (18) years who:Section 41-41-205: Individual instructions; power of attorney; decisions by primary physician; agents; guardians; validity.(i) Is or has been married; (ii) Has been adjudicated generally emancipated by a court of competent jurisdiction; or (iii) Has been adjudicated emancipated for the purpose of making health-care decisions by a court of competent jurisdiction.(f) "Guardian" means a judicially appointed guardian or conservator having authority to make a health-care decision for an individual. (g) "Health care" means any care, treatment, service, or procedure to maintain,diagnose, or otherwise affect an individual's physical or mental condition. (h) "Health-care decision" means a decision made by an individual or the individual's agent, guardian, or surrogate, regarding the individual's health care,including:(i) Selection and discharge of health-care providers and institutions; (ii) Approval or disapproval of diagnostic tests, surgical procedures, programs of medication, and orders not to resuscitate; and (iii) Directions to provide, withhold or withdraw artificial nutrition and hydration and all other forms of health care.The phrase "health-care decision" does not include decisions made pursuant to Sections 41-39-31 through 41-39-51, the "Anatomical Gift Law." (i) "Health-care institution" means an institution, facility, or agency licensed, certified, or otherwise authorized or permitted by law to provide health care in the ordinary course of business. (j) "Health-care provider" means an individual licensed, certified, or otherwise authorized or permitted by law to provide health care in the ordinary course of business or practice of a profession. (k) "Individual instruction" means an individual's direction concerning a health-care decision for the individual. (l) "Person" means an individual, corporation, business trust, estate, trust,partnership, association, joint venture, government, governmental subdivision, agency, or instrumentality, or any other legal or commercial entity. (m) "Physician" means an individual authorized to practice medicine or osteopathy under Title 73, Chapter 25, Mississippi Code of 1972. (n) "Power of attorney for health care" means the designation of an agent to make health-care decisions for the individual granting the power. (o) "Primary physician" means a physician designated by an individual or the individual's agent, guardian, or surrogate, to have primary responsibility for the individual's health care or, in the absence of a designation or if the designated physician is not reasonably available, a physician who undertakes the responsibility. (p) "Reasonably available" means readily able to be contacted without undue effort and willing and able to act in a timely manner considering the urgency of the patient's health-care needs. (q) "State" means a state of the United States, the District of Columbia, the Commonwealth of Puerto Rico, or a territory or insular possession subject to the jurisdiction of the United States. (r) "Supervising health-care provider" means the primary physician or, if there is no primary physician or the primary physician is not reasonably available,the health-care provider who has undertaken primary responsibility for an individual's health care. (s) "Surrogate" means an individual, other than a patient's agent or guardian, authorized under Sections 41-41-201 through 41-41-229 to make a health-care decision for the patient.
(1) An adult or emancipated minor may give an individual instruction. The instruction may be oral or written. The instruction may be limited to take effect only if a specified condition arises. (2) An adult or emancipated minor may execute a power of attorney for health care, which may authorize the agent to make any health-care decision the principal could have made while having capacity. The power remains in effect notwithstanding the principal's later incapacity and may include individual instructions. Unless related to the principal by blood, marriage, or adoption, an agent may not be an owner, operator, or employee of a residential long-term health-care institution at which the principal is receiving care. The power must be in writing, contain the date of its execution, be signed by the principal, and be witnessed by one (1) of the following methods:Section 41-41-207:(a) Be signed by at least two (2) individuals each of whom witnessed either the signing of the instrument by the principal or the principal's acknowledgement of the signature or of the instrument. See Form.(3) None of the following may be used as witness for a power of attorney for health care:(a) A health-care provider; (b) An employee of a health-care provider or facility; or (c) The agent.(4) At least one (1) of the individuals used as a witness for a power of attorney for health care shall be someone who is neither:(a) A relative of the principal by blood, marriage or adoption; nor (b) An individual who would be entitled to any portion of the estate of the principal upon his or her death under any will or codicil thereto of the principal existing at the time of execution of the power of attorney for health care or by operation of law then existing.(5) Unless otherwise specified in a power of attorney for health care, the authority of an agent becomes effective only upon a determination that the principal lacks capacity, and ceases to be effective upon a determination that the principal has recovered capacity. (6) Unless otherwise specified in a written advance health-care directive, a determination that an individual lacks or has recovered capacity, or that another condition exists that affects an individual instruction or the authority of an agent, must be made by the primary physician. (7) An agent shall make a health-care decision in accordance with the principal's individual instructions, if any, and other wishes to the extent known to the agent. Otherwise, the agent shall make the decision in accordance with the agent's determination of the principal's best interest. In determining the principal's best interest, the agent shall consider the principal's personal values to the extent known to the agent. (8) A health-care decision made by an agent for a principal is effective without judicial approval. (9) A written advance health-care directive may include the individual's nomination of a guardian of the person. (10) An advance health-care directive is valid for purposes of Sections 41-41-201 through 41-41-229 if it complies with Sections 41-41-201 through 41-41-229, regardless of when or where executed or communicated.
(1) An individual may revoke the designation of an agent only by a signed writing or by personally informing the supervising health-care provider. (2) An individual may revoke all or part of an advance health-care directive,other than the designation of an agent, at any time and in any manner that communicates an intent to revoke. (3) A health-care provider, agent, guardian, or surrogate who is informed of a revocation shall promptly communicate the fact of the revocation to the supervising health-care provider and to any health-care institution at which the patient is receiving care. (4) A decree of annulment, divorce, dissolution of marriage, or legal separation revokes a previous designation of a spouse as agent unless otherwise specified in the decree or in a power of attorney for health care. (5) An advance health-care directive that conflicts with an earlier advance health-care directive revokes the earlier directive to the extent of the conflict.Section 41-41-209: The following form may be used to create an advance health-care directive. Sections 41-41-201 through 41-41-207 and 41-41-211 through 41-41-229 govern the effect of this or any other writing used to create an advanced health-care directive. Section 41-41-211:
(1) A surrogate may make a health-care decision for a patient who is an adult or emancipated minor if the patient has been determined by the primary physician to lack capacity and no agent or guardian has been appointed or the agent or guardian is not reasonably available. (2) An adult or emancipated minor may designate any individual to act as surrogate by personally informing the supervising health-care provider. In the absence of a designation, or if the designee is not reasonably available, any member of the following classes of the patient's family who is reasonably available, in descending order of priority, may act as surrogate:Section 41-41-213:(a) The spouse, unless legally separated; (b) An adult child; (c) A parent; or (d) An adult brother or sister.(3) If none of the individuals eligible to act as surrogate under subsection (2) is reasonably available, an adult who has exhibited special care and concernfor the patient, who is familiar with the patient's personal values, and who is reasonably available may act as surrogate. (4) A surrogate shall communicate his or her assumption of authority as promptly as practicable to the members of the patient's family specified in subsection (2) who can be readily contacted. (5) If more than one (1) member of a class assumes authority to act as surrogate, and they do not agree on a health-care decision and the supervising health-care provider is so informed, the supervising health-care provider shall comply with the decision of a majority of the members of that class who have communicated their views to the provider. If the class is evenly divided concerning the health-care decision and the supervising health-care provider is so informed, that class and all individuals having lower priority are disqualified from making the decision. (6) A surrogate shall make a health-care decision in accordance with the patient's individual instructions, if any,and other wishes to the extent known to the surrogate. Otherwise, the surrogate shall make the decision in accordance with the surrogate's determination of the patient's best interest. In determining the patient's best interest, the surrogate shall consider the patient's personal values to the extent known to the surrogate. (7) A health-care decision made by a surrogate for a patient is effective without judicial approval. (8) An individual at any time may disqualify another, including a member of the individual's family, from acting as the individual's surrogate by a signed writing or by personally informing the supervising health-care provider of the disqualification. (9) A surrogate may not be an owner, operator, or employee of a residential long-term health-care institution at which the patient is receiving care unless related to the patient by blood, marriage, or adoption, except in the case of a patient of a state-operated facility who has no person listed in subsection (2) reasonably available to act as a surrogate. (10) A supervising health-care provider may require an individual claiming the right to act as surrogate for a patient to provide a written declaration under penalty of perjury stating facts and circumstances reasonably sufficient to establish the claimed authority.
(1) A guardian shall comply with the ward's individual instructions and may not revoke the ward's advance health-care directive unless the appointing court expressly so authorizes. (2) Absent a court order to the contrary, a health-care decision of an agent takes precedence over that of a guardian. (3) A health-care decision made by a guardian for the ward is effective without judicial approval.Section 41-41-215:
(1) Before implementing a health-care decision made for a patient, a supervising health-care provider, if possible, shall promptly communicate to the patient the decision made and the identity of the person making the decision. (2) A supervising health-care provider who knows of the existence of an advance health-care directive, a revocation of an advance health-care directive, or a designation or disqualification of a surrogate, shall promptly record its existence in the patient's health-care record and, if it is in writing, shall request a copy and if one is furnished shall arrange for its maintenance in the health-care record. (3) A primary physician who makes or is informed of a determination that a patient lacks or has recovered capacity, or that another condition exists which affects an individual instruction or the authority of an agent, guardian, or surrogate, shall promptly record the determination in the patient's health-care record and communicate the determination to the patient, if possible, and to any person then authorized to make health-care decisions for the patient. (4) Except as provided in subsections (5) and (6), a health-care provider or institution providing care to a patient shall:Section 41-41-217: Unless otherwise specified in an advance health-care directive, a person then authorized to make health-care decisions for a patient has the same rights as the patient to request, receive, examine, copy and consent to the disclosure of medical or any other health-care information. Section 41-41-219:(a) Comply with an individual instruction of the patient and with a reasonable interpretation of that instruction made by a person then authorized to make health-care decisions for the patient; and (b) Comply with a health-care decision for the patient made by a person then authorized to make health-care decisions for the patient to the same extent as if the decision had been made by the patient while having capacity.(5) A health-care provider may decline to comply with an individual instruction or health-care decision for reasons of conscience. A health-care institution may decline to comply with an individual instruction or health-care decision if the instruction or decision is contrary to a policy of the institution which is expressly based on reasons of conscience and if the policy was timely communicated to the patient or to a person then authorized to make health-care decisions for the patient. (6) A health-care provider or institution may decline to comply with an individual instruction or health-care decision that requires medically ineffective health care or health care contrary to generally accepted health-care standards applicable to the health-care provider or institution. (7) A health-care provider or institution that declines to comply with an individual instruction or health-care decision shall:(a) Promptly so inform the patient, if possible, and any person then authorized to make health-care decisions for the patient; (b) Provide continuing care to the patient until a transfer can be effected; and (c) Unless the patient or person then authorized to make health-care decisions for the patient refuses assistance, immediately make all reasonable efforts to assist in the transfer of the patient to another health-care provider or institution that is willing to comply with the instruction or decision.(8) A health-care provider or institution may not require or prohibit the execution or revocation of an advance health-care directive as a condition for providing health care. (9) If the patient who is an adult or emancipated minor has been determined by the primary physician to lack capacity to make a health-care decision and an agent, guardian or surrogate is not reasonably available, consent may be given by an owner, operator or employee of a residential long-term health care institution at which the patient is a resident if there is no advance health-care directive to the contrary and a licensed physician who is not an owner, operator or employee of the residential long-term health care institution at which the patient is a resident has determined that the patient is in need of health care. This power to consent is limited to the terms of this subsection (9) and shall not be construed to repeal or otherwise affect the prohibition of Section 41-41-211 (9) relating to owners, operators, or employees of long-term health care institutions. The consent given pursuant to this subsection shall be limited to the health care services determined necessary by the licensed physician and shall in no event include the power to consent to or direct withholding or discontinuing any life support, nutrition, hydration or other treatment, care or support. When consent is obtained under this subsection, compliance with these requirements shall be stated in the patient's health-care record.
(1) A health-care provider or institution acting in good faith and in accordance with generally accepted health-care standards applicabl to the health-care provider or institution is not subject to civil or criminal liability or to discipline for unprofessional conduct for:Section 41-41-221:(a) Complying with a health-care decision of a person apparently having authority to make a health-care decision for a patient, including a decision to withhold or withdraw health care; (b) Declining to comply with a health-care decision of a person based on a belief that the person then lacked authority; or (c) Complying with an advance health-care directive and assuming that the directive was valid when made and has not been revoked or terminated.(2) An individual acting as agent or surrogate under Sections 41-41-201 through 41-41-229 is not subject to civil or criminal liability or to discipline for unprofessional conduct for health-care decisions made in good faith.
(1) A health-care provider or institution that intentionally violates Sections 41-41-201 through 41-41-229 is subject to liability to the aggrieved individual for damages of Five Hundred Dollars ($500.00) or actual damages resulting from the violation, whichever is greater, plus reasonable attorney's fees. (2) A person who intentionally falsifies, forges, conceals, defaces, or obliterates an individual's advance health-care directive or a revocation of an advance health-care directive without the individual's consent, or who coerces or fraudulently induces an individual to give, revoke, or not to give an advance health-care directive, is subject to liability to that individual for damages of Twenty-five Hundred Dollars ($2,500.00) or actual damages resulting from the action, whichever is greater, plus reasonable attorney's fees.Section 41-41-223:
(1) Sections 41-41-201 through 41-41-229 do not affect the right of an individual to make health-care decisions while having capacity to do so. (2) An individual is presumed to have capacity to make a health-care decision, to give or revoke an advance health-care directive, and to designate or disqualify a surrogate.Section 41-41-225: A copy of a written advance health-care directive, revocation of an advance health-care directive, or designation or disqualification of a surrogate has the same effect as the original. Section 41-41-227:
(1) Sections 41-41-201 through 41-41-229 do not create a presumption concerning the intention of an individual who has not made or who has revoked an advance health-care directive. (2) Death resulting from the withholding or withdrawal of health care in accordance with Sections 41-41-201 through 41-41-229 does not for any purpose constitute a suicide or homicide or legally impair or invalidate a policy of insurance or an annuity providing a death benefit, notwithstanding any term of the policy or annuity to the contrary. (3) Sections 41-41-201 through 41-41-229 do not authorize mercy killing, assisted suicide, euthanasia, or the provision, withholding, or withdrawal of health care, to the extent prohibited by other statutes of this state. (4) Sections 41-41-201 through 41-41-229 do not authorize or require a health-care provider or institution to provide health care contrary to generally accepted health-care standards applicable to the health-care provider or institution. (5) Sections 41-41-201 through 41-41-229 do not authorize an agent or surrogate to consent to the admission of an individual to a mental health-care institution unless the individual's written advance health-care directive expressly so provides. (6) Sections 41-41-201 through 41-41-229 do not affect other statutes of this state governing treatment for mental illness of an individual involuntarily committed to a mental health-care institution. (7) Sections 41-41-201 through 41-41-229 do not apply to Sections 41-41-31 through 41-41-39, which govern the performance of abortions, or Sections 41-41-51 through 41-41-63, which govern the performance of abortions upon minors.Section 41-41-229: On petition of a patient, the patient's agent, guardian, or surrogate, a health-care provider or institution involved with the patient's care, or an individual described in Section 41-41-211(2) or (3), any court of competent jurisdiction may enjoin or direct a health-care decision or order other equitable relief. A proceeding under this section shall be governe by the Mississippi Rules of Civil Procedure. Note: All Information and Previews are subject to the Disclaimer located on the main forms page, and also linked at the bottom of all search results.