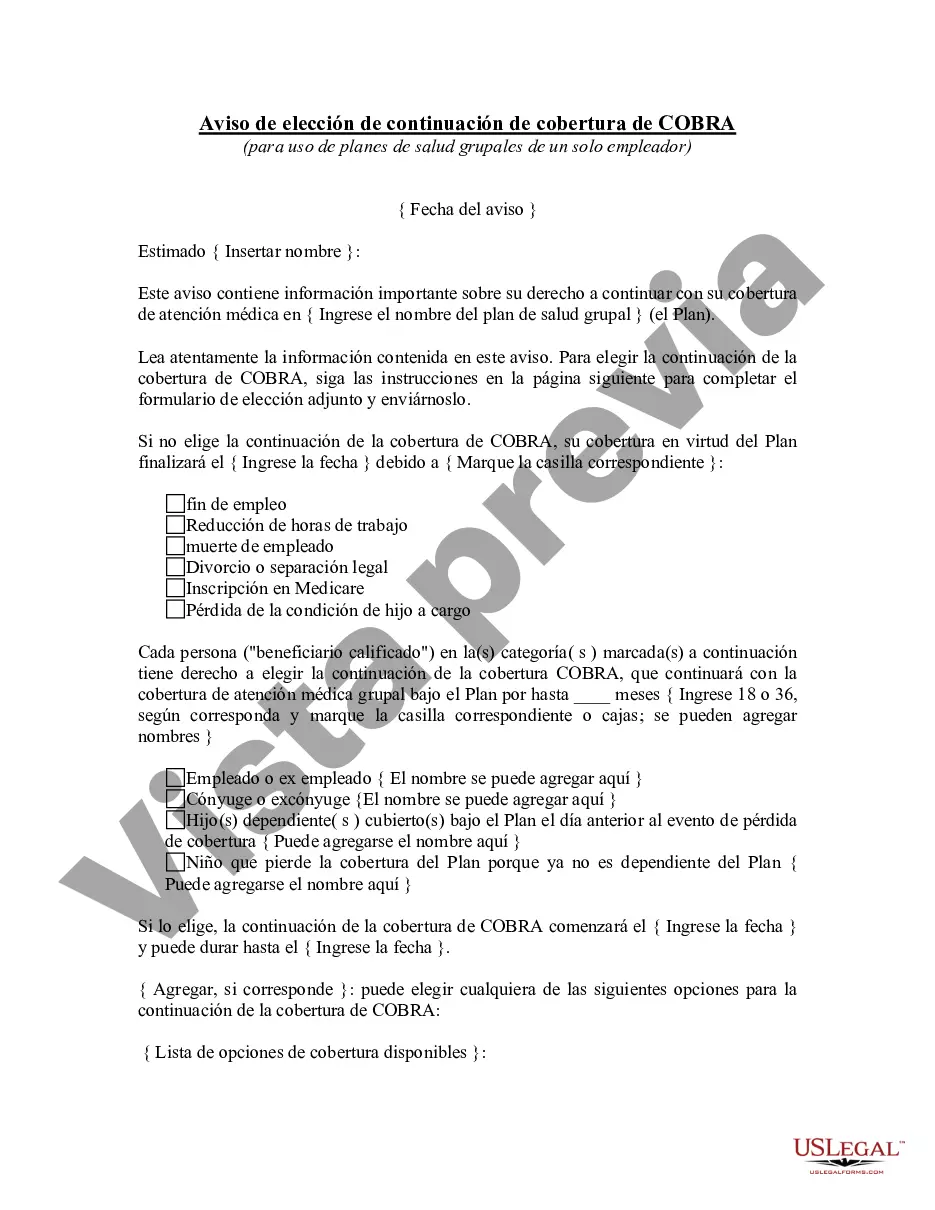
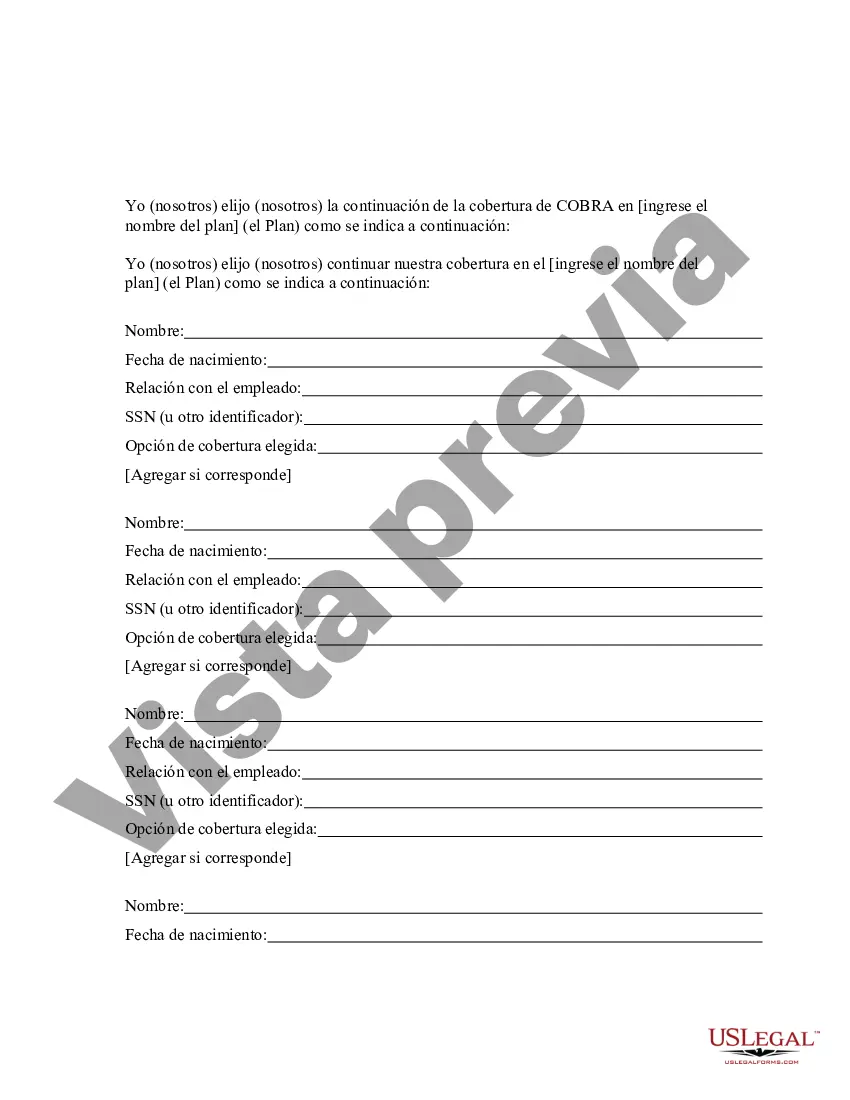
The New Jersey COBRA Continuation Coverage Election Notice is a crucial document that provides important information regarding healthcare coverage options to individuals who experience a qualifying event, such as job loss or reduction in work hours, resulting in the loss of health insurance benefits. It is mandated by the Consolidated Omnibus Budget Reconciliation Act (COBRA) and is specific to the state of New Jersey. This notice aims to inform individuals about their rights and options to continue their health insurance coverage through the COBRA program. By law, employers with 20 or more employees must offer this coverage to eligible employees and their dependents. The New Jersey COBRA Continuation Coverage Election Notice ensures that individuals are aware of these rights and can make an informed decision regarding their healthcare coverage. The notice typically includes essential details such as the employee's eligibility for COBRA coverage, the qualifying event that triggered the need for COBRA, the duration and cost of coverage, and the steps individuals need to take to elect coverage. It also outlines the consequences of not electing COBRA continuation coverage within the specified timeframe. Keywords: New Jersey, COBRA Continuation Coverage Election Notice, healthcare coverage options, qualifying event, job loss, reduction in work hours, health insurance benefits, Consolidated Omnibus Budget Reconciliation Act, COBRA program, eligible employees, dependents, informed decision, healthcare coverage, COBRA coverage, duration, cost of coverage, elect coverage, consequences, specified timeframe. Different types of New Jersey COBRA Continuation Coverage Election Notices may exist based on the specific circumstances or qualifying events, such as: 1. New Jersey COBRA Continuation Coverage Election Notice for Job Loss: This notice is issued to employees who have been terminated from their job and have lost their health insurance benefits as a result. 2. New Jersey COBRA Continuation Coverage Election Notice for Reduction in Work Hours: This notice is provided to employees whose work hours have been significantly reduced, leading to the loss of health insurance benefits. 3. New Jersey COBRA Continuation Coverage Election Notice for Divorce or Legal Separation: In cases where an employee and their spouse were covered under the employer's health insurance plan, and they go through a divorce or legal separation, this notice is issued to inform them of their COBRA rights and options. 4. New Jersey COBRA Continuation Coverage Election Notice for Dependents Aging Out: If a dependent child of an employee ceases to be eligible for coverage due to reaching the maximum age limit specified by the employer's health insurance plan, this notice is sent to notify the employee of the COBRA continuation coverage available to their dependent. Note: The specific types of notices may vary based on the employer's policies, eligibility criteria, and the circumstances triggering the need for COBRA continuation coverage.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.New Jersey Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
How to fill out New Jersey Aviso De Elección De Continuación De Cobertura De COBRA?
You may invest time online looking for the lawful papers design that fits the federal and state requirements you want. US Legal Forms gives thousands of lawful forms that are examined by professionals. You can actually obtain or produce the New Jersey COBRA Continuation Coverage Election Notice from your service.
If you already have a US Legal Forms accounts, you can log in and then click the Obtain key. After that, you can comprehensive, revise, produce, or indication the New Jersey COBRA Continuation Coverage Election Notice. Each lawful papers design you buy is yours eternally. To have one more copy for any obtained form, proceed to the My Forms tab and then click the corresponding key.
Should you use the US Legal Forms website for the first time, stick to the basic guidelines under:
- Very first, ensure that you have chosen the right papers design for your region/area of your choice. See the form description to make sure you have chosen the proper form. If accessible, use the Review key to search through the papers design as well.
- In order to find one more version of your form, use the Lookup discipline to get the design that meets your requirements and requirements.
- Once you have located the design you would like, just click Acquire now to move forward.
- Pick the prices plan you would like, type in your qualifications, and register for a free account on US Legal Forms.
- Comprehensive the financial transaction. You can use your charge card or PayPal accounts to purchase the lawful form.
- Pick the file format of your papers and obtain it to the product.
- Make alterations to the papers if needed. You may comprehensive, revise and indication and produce New Jersey COBRA Continuation Coverage Election Notice.
Obtain and produce thousands of papers templates while using US Legal Forms Internet site, which provides the greatest selection of lawful forms. Use professional and state-particular templates to deal with your company or specific demands.