Oklahoma Introductory COBRA Letter
Description
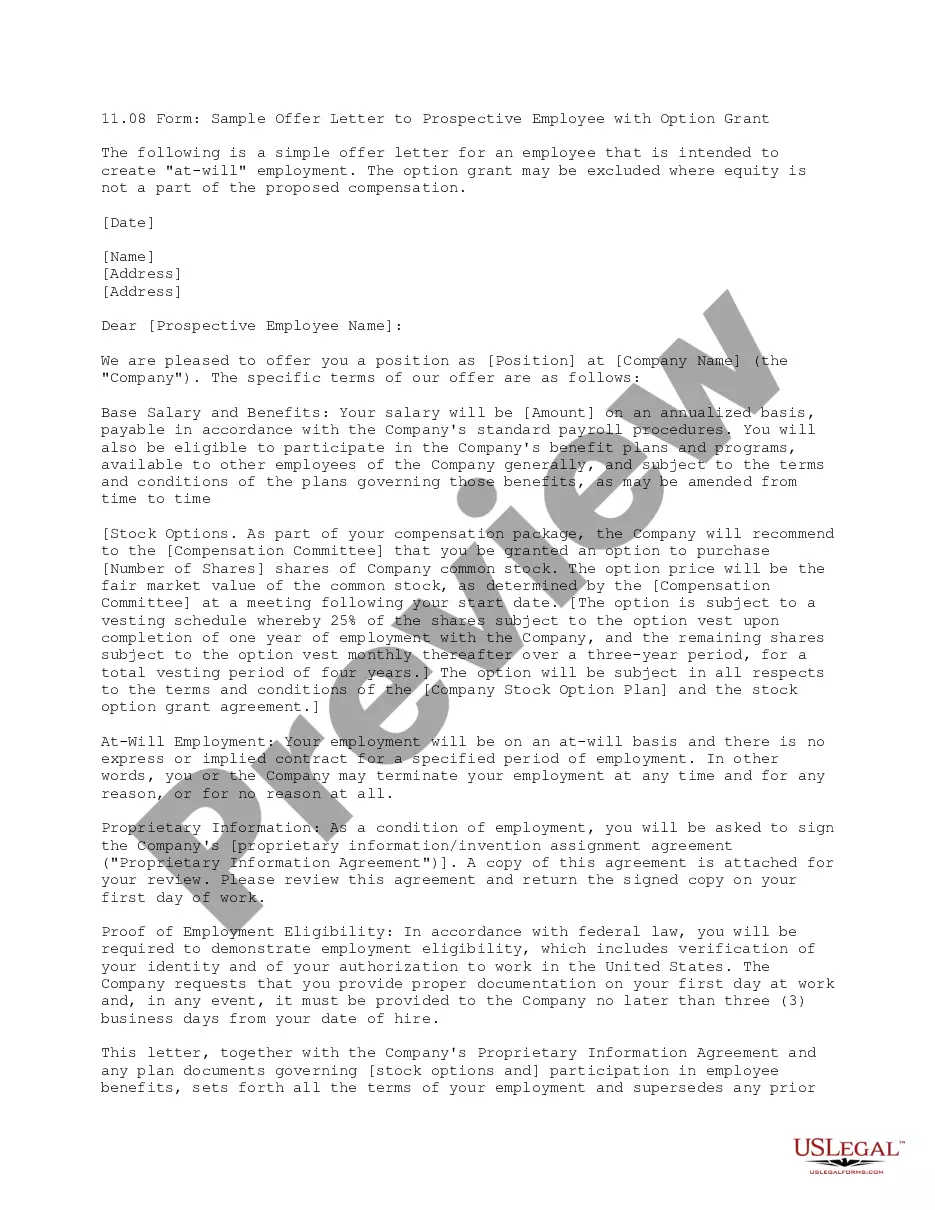
How to fill out Introductory COBRA Letter?
Selecting the optimal legal document format can be quite challenging. Of course, there are numerous templates accessible online, but how can you secure the legal draft you need? Visit the US Legal Forms website.
This service provides thousands of templates, including the Oklahoma Introductory COBRA Letter, which you can utilize for business and personal purposes. All documents are vetted by professionals and comply with state and federal regulations.
If you are already registered, Log In to your account and click the Download button to obtain the Oklahoma Introductory COBRA Letter. Use your account to search through the legal documents you have previously purchased. Navigate to the My documents section of your account and download another copy of the document you need.
US Legal Forms is the largest repository of legal documents where you can find a variety of document templates. Utilize this service to obtain professionally crafted papers that adhere to state requirements.
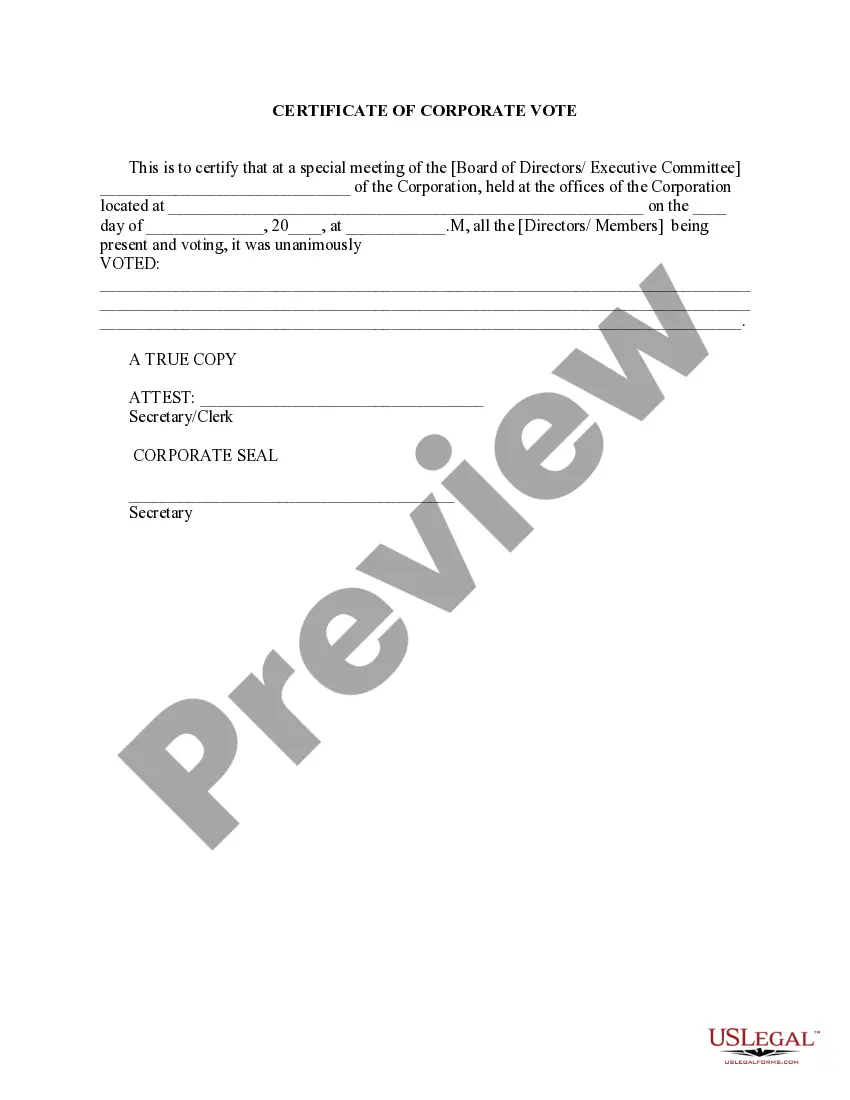
- First, ensure you have selected the correct form for your area/county. You can review the form using the Preview button and read the form description to confirm it is right for you.
- If the form does not fulfill your requirements, use the Search field to find the appropriate form.
- Once you are certain that the form is suitable, click the Get Now button to acquire the form.
- Choose the pricing plan you prefer and enter the necessary information. Create your account and complete your order using your PayPal account or credit card.
- Select the document format and download the legal document format to your device.
- Complete, edit, print, and sign the received Oklahoma Introductory COBRA Letter.
Form popularity
FAQ
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
COBRA is a federal law that lets you keep yourself and your family covered by your employee health plan. Coverage is only available for a limited time (often 18 months) after you leave your job or lose coverage through your employer. You pay the full monthly premium, including any amount that your employer had paid.
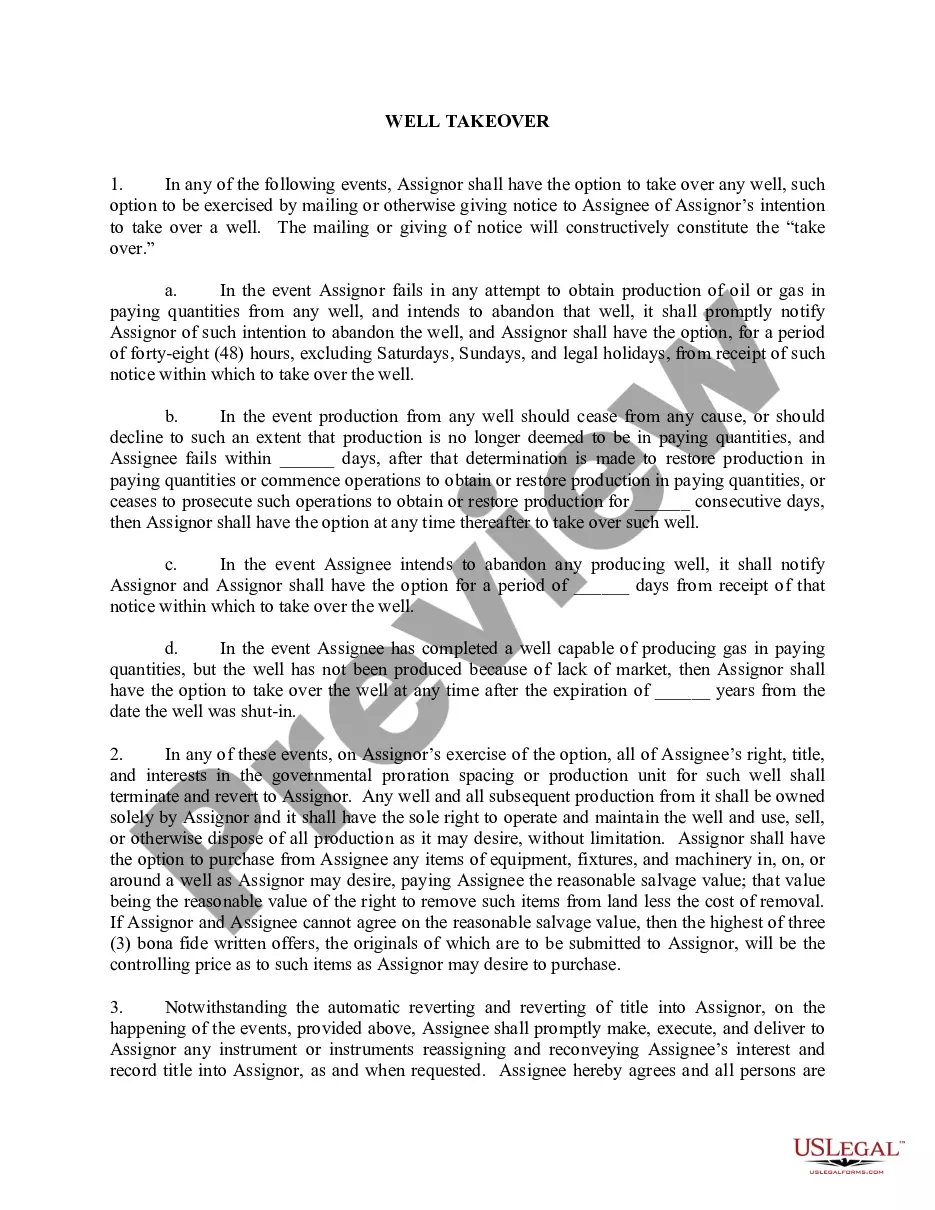
Oklahoma requires limited continuation of healthcare plan coverage for employees whose employer is not covered by the federal Consolidated Omnibus Budget Reconciliation Act (COBRA) (OK Stat. Tit. 36 Sec. 4509).
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
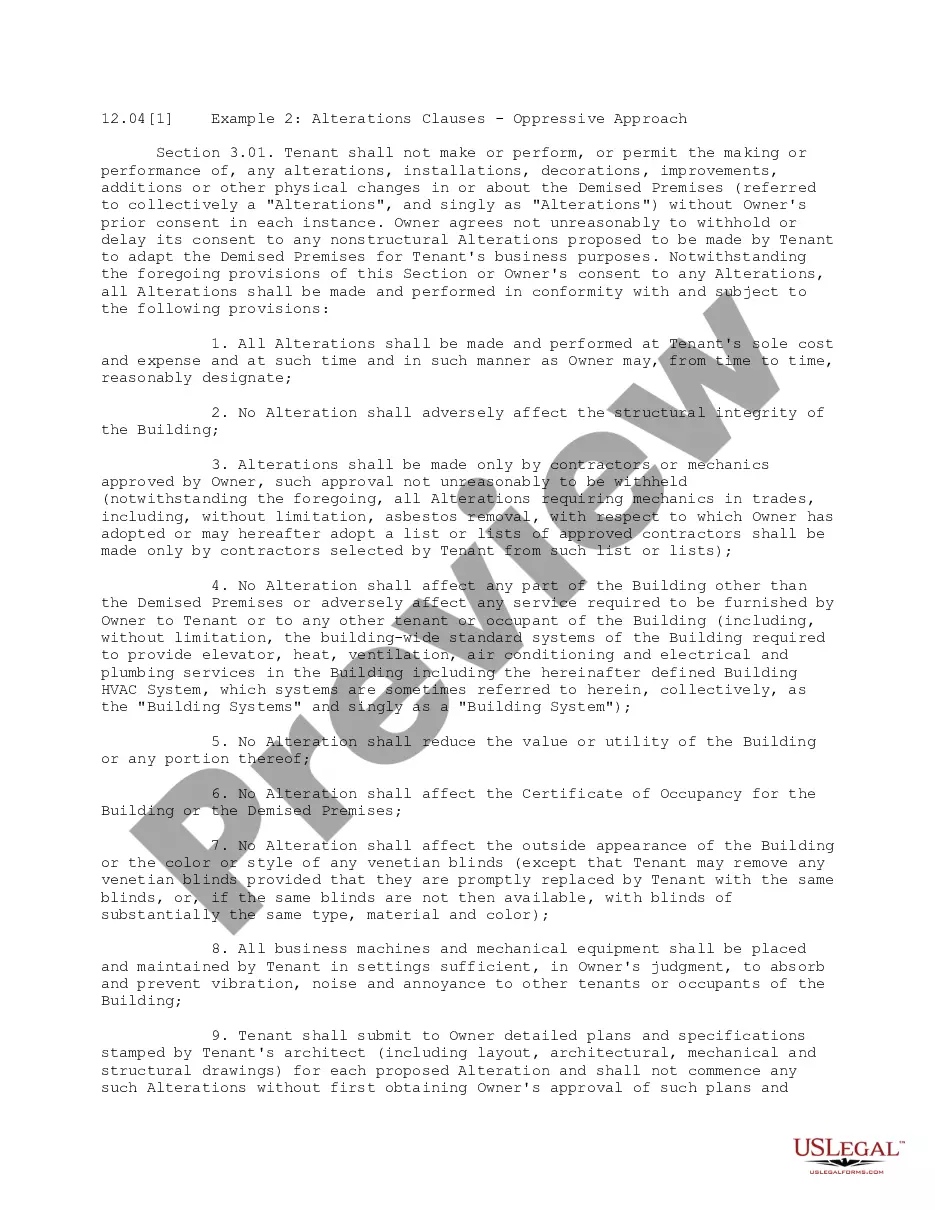
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.