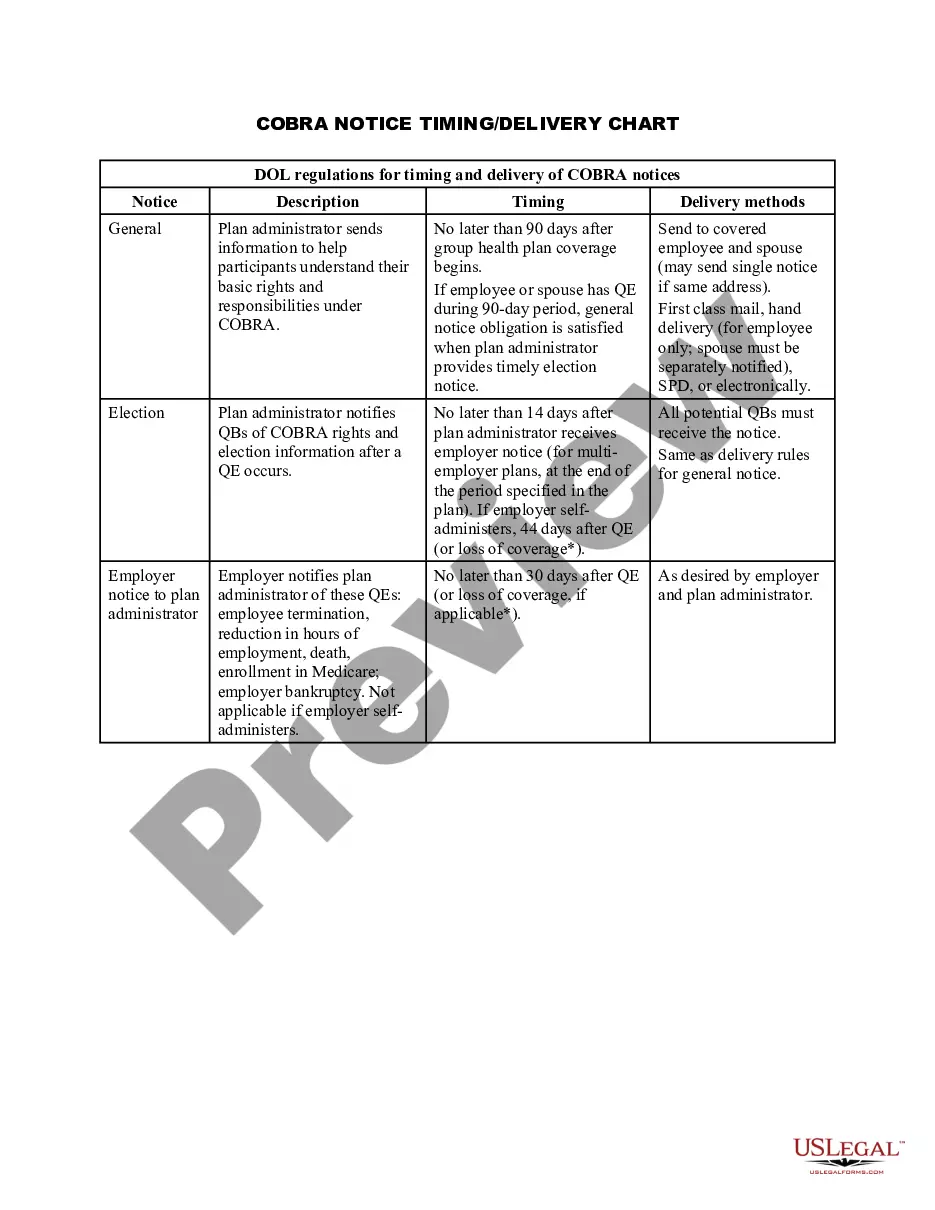
COBRA Notice Timing Delivery Chart
Description Cobra Notice Timing
How to fill out Cobra Timeline Chart?
Employ the most extensive legal library of forms. US Legal Forms is the perfect platform for getting updated COBRA Notice Timing Delivery Chart templates. Our platform offers thousands of legal documents drafted by licensed lawyers and sorted by state.
To get a template from US Legal Forms, users just need to sign up for an account first. If you are already registered on our service, log in and choose the document you are looking for and purchase it. After buying forms, users can see them in the My Forms section.
To obtain a US Legal Forms subscription online, follow the steps below:
- Find out if the Form name you’ve found is state-specific and suits your requirements.
- In case the form features a Preview option, utilize it to review the sample.
- If the sample doesn’t suit you, make use of the search bar to find a better one.
- Hit Buy Now if the sample meets your requirements.
- Select a pricing plan.
- Create a free account.
- Pay via PayPal or with yourr credit/credit card.
- Choose a document format and download the sample.
- As soon as it’s downloaded, print it and fill it out.
Save your effort and time using our platform to find, download, and complete the Form name. Join a large number of pleased subscribers who’re already using US Legal Forms!
Cobra Notice Template Form popularity
Notice Chart Other Form Names
Cobra Election Timeline FAQ
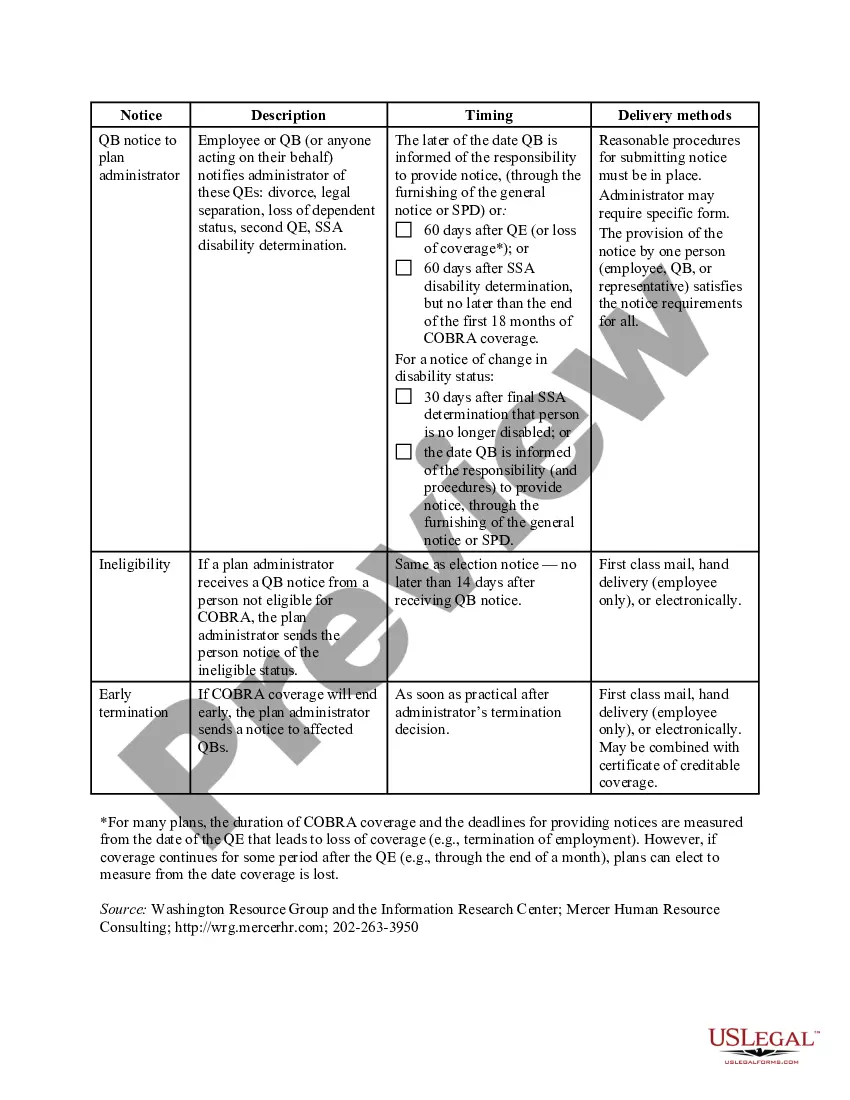
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
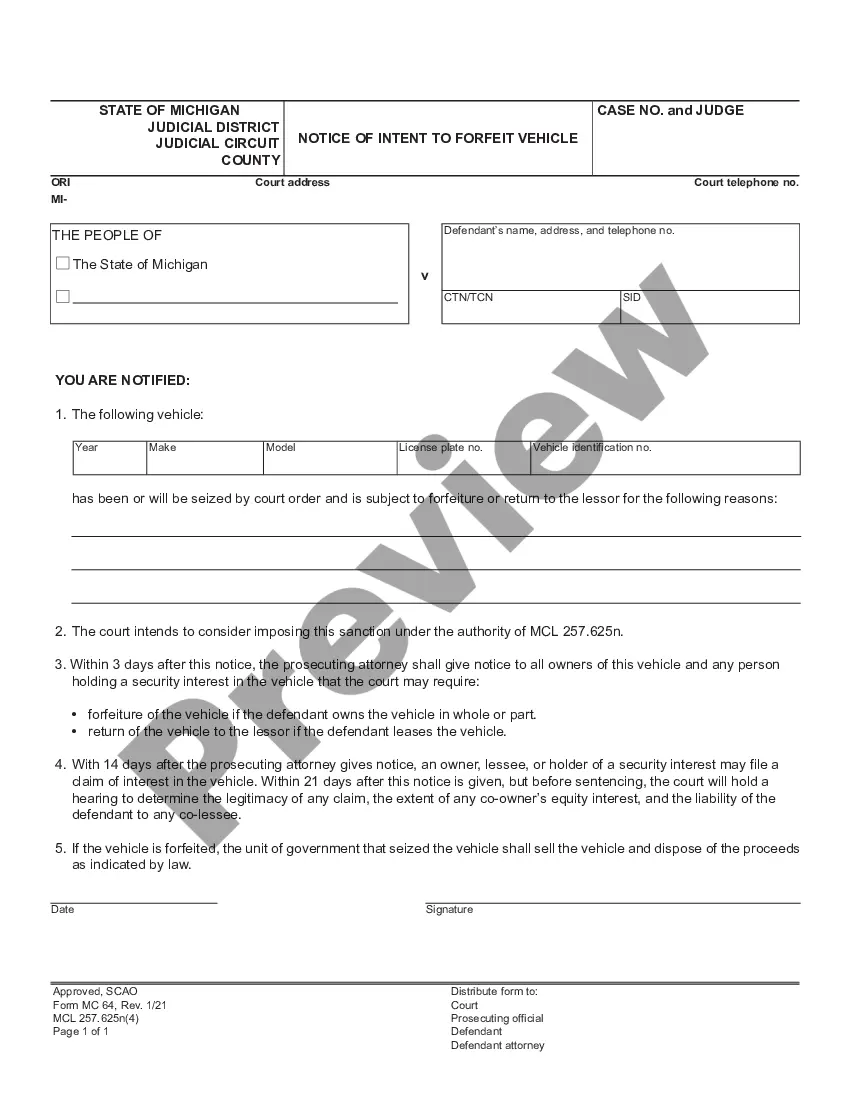
An employer that is subject to COBRA requirements is required to notify its group health plan administrator within 30 days after an employee's employment is terminated, or employment hours are reduced.
Notices properly mailed are generally considered provided on the date sent, regardless of whether they're actually received. 1. COBRA Initial Notice must be provided. Within 30 days after the employee first becomes enrolled in the group health plan.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
COBRA Coverage Timeline An employee who's eligible for Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage must elect it within 60 days of their insurance termination date, or the date that the employee recieved their COBRA notification, whichever is later.
The insurance company. COBRA Election Notice. After receiving a notice of a qualifying event, the plan must provide the qualified beneficiaries with an election notice within 14 days. The election notice describes their rights to continuation coverage and how to make an election.
The employer must notify the plan within 30 days of the event. You (the covered employee or one of the qualified beneficiaries) must notify the plan if the qualifying event is divorce, legal separation, or a child's loss of dependent status under the plan.