Title: Understanding Wisconsin's Summary of Rights and Obligations under COBRA Introduction: The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law that guarantees continuation of health coverage for workers and their families after a job loss or other qualifying events. This summary aims to provide a comprehensive overview of Wisconsin's specific provisions regarding COBRA rights and obligations, ensuring individuals are well-informed about their coverage options during transitional periods. 1. Understanding Wisconsin's COBRA: Wisconsin follows the federal COBRA guidelines, which means the state implements the same set of regulations for continuation of health coverage. However, it is essential to note that there are additional state-specific provisions important for Wisconsin residents to be aware of. 2. Qualifying Events: In Wisconsin, the standard qualifying events for COBRA eligibility include: — Job termination (except for gross misconduct) — Reduction in work hours leading to loss of health benefits — Divorce or legal separation from the covered employee — Death of the covereemployedye— - Loss of dependent child status under the health plan — Medicare entitlement of the covered employee 3. Notice Requirements: Employers in Wisconsin are obligated to provide written notice to eligible individuals within specific time frames. They must inform employees and their families of their rights when they become eligible for COBRA benefits, and also provide timely notice of potential coverage termination or other circumstances impacting their continuation coverage. 4. Coverage Duration and Premiums: Wisconsin adheres to the federal COBRA maximum coverage period, which usually lasts up to 18 months for those who experience qualifying events. However, certain circumstances may allow for extended coverage periods. It's crucial for individuals to understand their rights and obligations in terms of premium payments to ensure uninterrupted coverage. 5. Conversion Rights: In addition to COBRA, Wisconsin maintains conversion rights that allow individuals to convert their group health plan coverage into an individual policy after their COBRA coverage has expired. This option ensures individuals have continued access to health insurance in case they are ineligible for further COBRA coverage. 6. Extensions and Alternate State Programs: While Wisconsin generally follows the federal COBRA guidelines, it's worth noting that there may be other state-specific programs or extensions available to individuals. Exploring these options may provide additional coverage opportunities for workers and their families during transitional periods. Conclusion: Wisconsin's Summary of Rights and Obligations under COBRA provides vital information regarding health coverage continuation for individuals facing qualifying events. By understanding these rights, individuals can make informed decisions about their healthcare options and ensure seamless coverage during challenging times. It is essential for employees and their families to stay updated on Wisconsin's specific provisions to fully benefit from the offered COBRA protections.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Wisconsin Resumen de derechos y obligaciones bajo COBRA - Summary of Rights and Obligations under COBRA
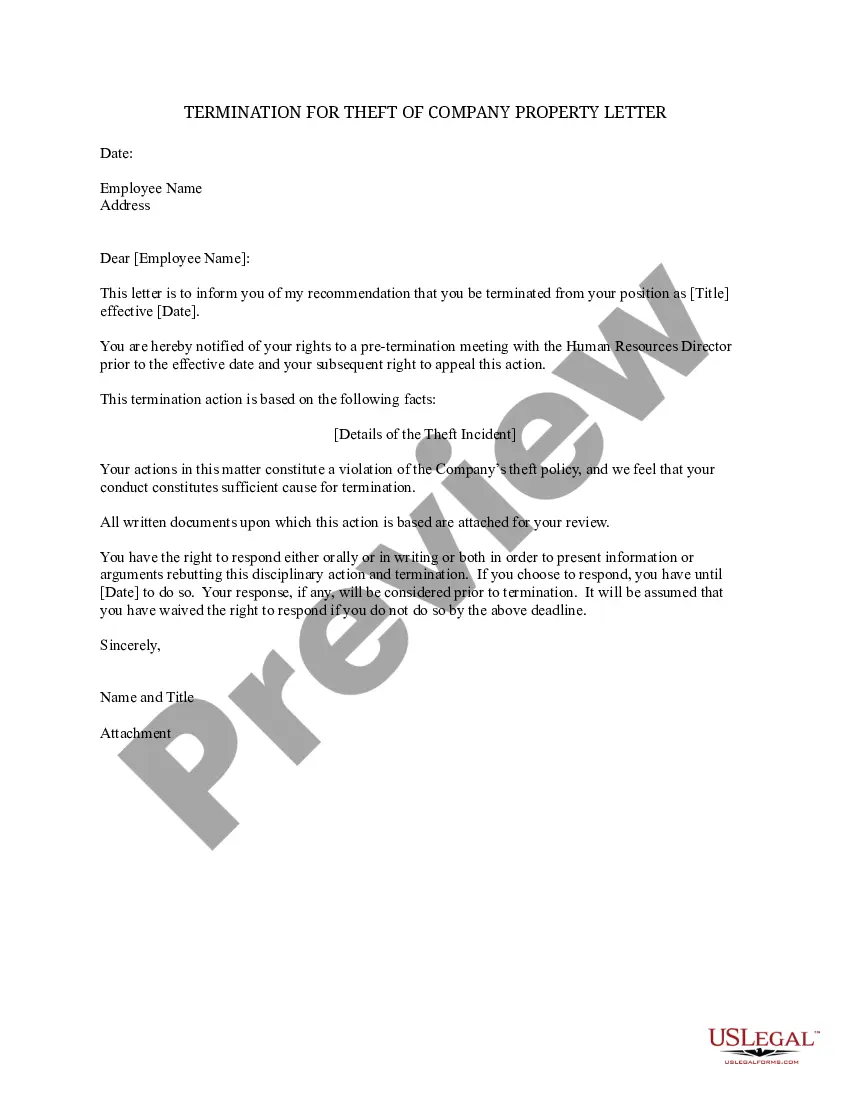
Description
How to fill out Wisconsin Resumen De Derechos Y Obligaciones Bajo COBRA?
Have you been in the place in which you require files for both enterprise or specific functions almost every time? There are plenty of legitimate file templates available on the net, but getting types you can rely on isn`t easy. US Legal Forms gives 1000s of develop templates, such as the Wisconsin Summary of Rights and Obligations under COBRA, which can be created to satisfy state and federal demands.
If you are already informed about US Legal Forms web site and possess a free account, simply log in. Next, you can download the Wisconsin Summary of Rights and Obligations under COBRA web template.
Unless you offer an accounts and want to start using US Legal Forms, adopt these measures:
- Find the develop you want and make sure it is for your correct area/county.
- Utilize the Preview option to check the shape.
- Read the information to actually have chosen the proper develop.
- When the develop isn`t what you are looking for, utilize the Look for discipline to find the develop that fits your needs and demands.
- Once you find the correct develop, click Acquire now.
- Opt for the costs prepare you would like, fill in the desired information to create your account, and pay for the transaction with your PayPal or charge card.
- Decide on a handy file formatting and download your duplicate.
Find all the file templates you may have bought in the My Forms food selection. You can get a further duplicate of Wisconsin Summary of Rights and Obligations under COBRA at any time, if necessary. Just select the necessary develop to download or printing the file web template.
Use US Legal Forms, probably the most considerable variety of legitimate types, to conserve some time and prevent blunders. The support gives appropriately created legitimate file templates that can be used for an array of functions. Create a free account on US Legal Forms and begin generating your way of life easier.