Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
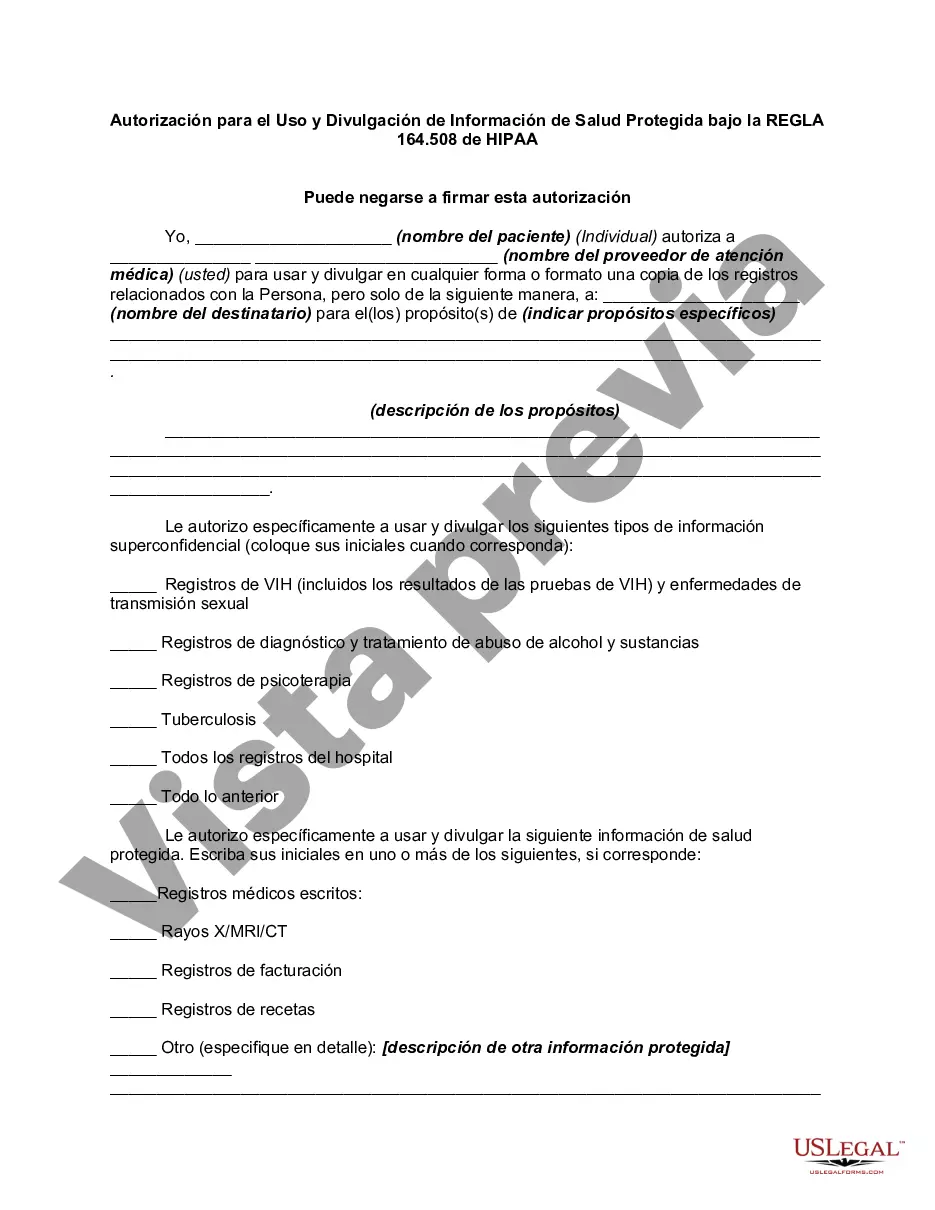
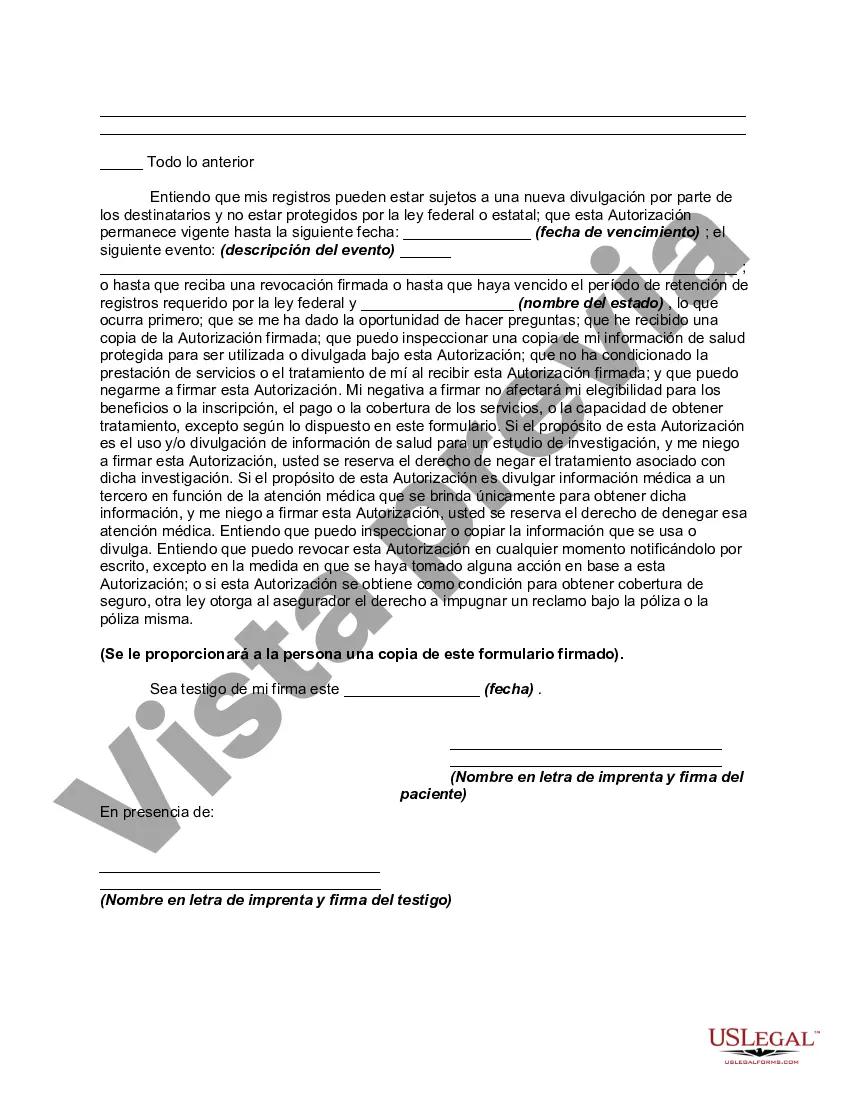
Harris Texas Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 — A Comprehensive Overview Introduction: The Harris Texas Authorization for Use and Disclosure of Protected Health Information (PHI) under HIPAA Rule 164.508 plays a vital role in safeguarding patients' privacy and determining when and how their healthcare information can be shared. This detailed description will provide insight into the purpose, requirements, and different types of authorizations relevant to Harris Texas and HIPAA Rule 164.508. 1. Purpose: The primary purpose of Harris Texas Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 is to give individuals control over the use and disclosure of their sensitive healthcare information. This authorization is a legal document that allows covered entities and healthcare providers to share PHI for specific purposes, ensuring compliance with the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. 2. Key Requirements: To ensure proper authorization and disclosure of PHI, the Harris Texas Authorization must meet the following requirements: — Be in writing and signed by the individual or their legally authorized representative. — Clearly state the purpose of the disclosure. — Identify the specific information being disclosed. — Specify who is authorized to make the disclosure and to whom the disclosure will be made. — Include an expiration date or event triggering the termination of authorization. — Inform individuals of their right to revoke the authorization in writing. 3. Different Types of Harris Texas Authorizations: There are various types of authorizations under Harris Texas Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, including: — General Authorization: This type of authorization permits the disclosure of PHI for a broad range of purposes, such as treatment, payment, and healthcare operations. — Research Authorization: Research-specific authorizations are required when PHI is used for research purposes. These authorizations provide detailed information about the study, the parties involved, and the potential risks involved. — Psychotherapy Note Authorization: This specific authorization allows for the disclosure of psychotherapy notes, which are detailed notes taken by mental health professionals during sessions. Psychotherapy notes have stricter disclosure requirements compared to other types of PHI. — Marketing Authorization: A marketing authorization allows covered entities to use PHI for marketing purposes. This authorization must clearly state that the individual's healthcare information will be used for marketing communication and specify the types of communication involved. Conclusion: In conclusion, the Harris Texas Authorization for Use and Disclosure of Protected Health Information under HIPAA Rule 164.508 is a crucial component in protecting patients' privacy and governing the sharing of their healthcare information. Its various types of authorizations help ensure that PHI is disclosed appropriately and in accordance with HIPAA guidelines. By providing individuals with control over their information, this authorization empowers them to make informed decisions about the use and disclosure of their protected health information.Harris Texas Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 — A Comprehensive Overview Introduction: The Harris Texas Authorization for Use and Disclosure of Protected Health Information (PHI) under HIPAA Rule 164.508 plays a vital role in safeguarding patients' privacy and determining when and how their healthcare information can be shared. This detailed description will provide insight into the purpose, requirements, and different types of authorizations relevant to Harris Texas and HIPAA Rule 164.508. 1. Purpose: The primary purpose of Harris Texas Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 is to give individuals control over the use and disclosure of their sensitive healthcare information. This authorization is a legal document that allows covered entities and healthcare providers to share PHI for specific purposes, ensuring compliance with the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. 2. Key Requirements: To ensure proper authorization and disclosure of PHI, the Harris Texas Authorization must meet the following requirements: — Be in writing and signed by the individual or their legally authorized representative. — Clearly state the purpose of the disclosure. — Identify the specific information being disclosed. — Specify who is authorized to make the disclosure and to whom the disclosure will be made. — Include an expiration date or event triggering the termination of authorization. — Inform individuals of their right to revoke the authorization in writing. 3. Different Types of Harris Texas Authorizations: There are various types of authorizations under Harris Texas Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, including: — General Authorization: This type of authorization permits the disclosure of PHI for a broad range of purposes, such as treatment, payment, and healthcare operations. — Research Authorization: Research-specific authorizations are required when PHI is used for research purposes. These authorizations provide detailed information about the study, the parties involved, and the potential risks involved. — Psychotherapy Note Authorization: This specific authorization allows for the disclosure of psychotherapy notes, which are detailed notes taken by mental health professionals during sessions. Psychotherapy notes have stricter disclosure requirements compared to other types of PHI. — Marketing Authorization: A marketing authorization allows covered entities to use PHI for marketing purposes. This authorization must clearly state that the individual's healthcare information will be used for marketing communication and specify the types of communication involved. Conclusion: In conclusion, the Harris Texas Authorization for Use and Disclosure of Protected Health Information under HIPAA Rule 164.508 is a crucial component in protecting patients' privacy and governing the sharing of their healthcare information. Its various types of authorizations help ensure that PHI is disclosed appropriately and in accordance with HIPAA guidelines. By providing individuals with control over their information, this authorization empowers them to make informed decisions about the use and disclosure of their protected health information.
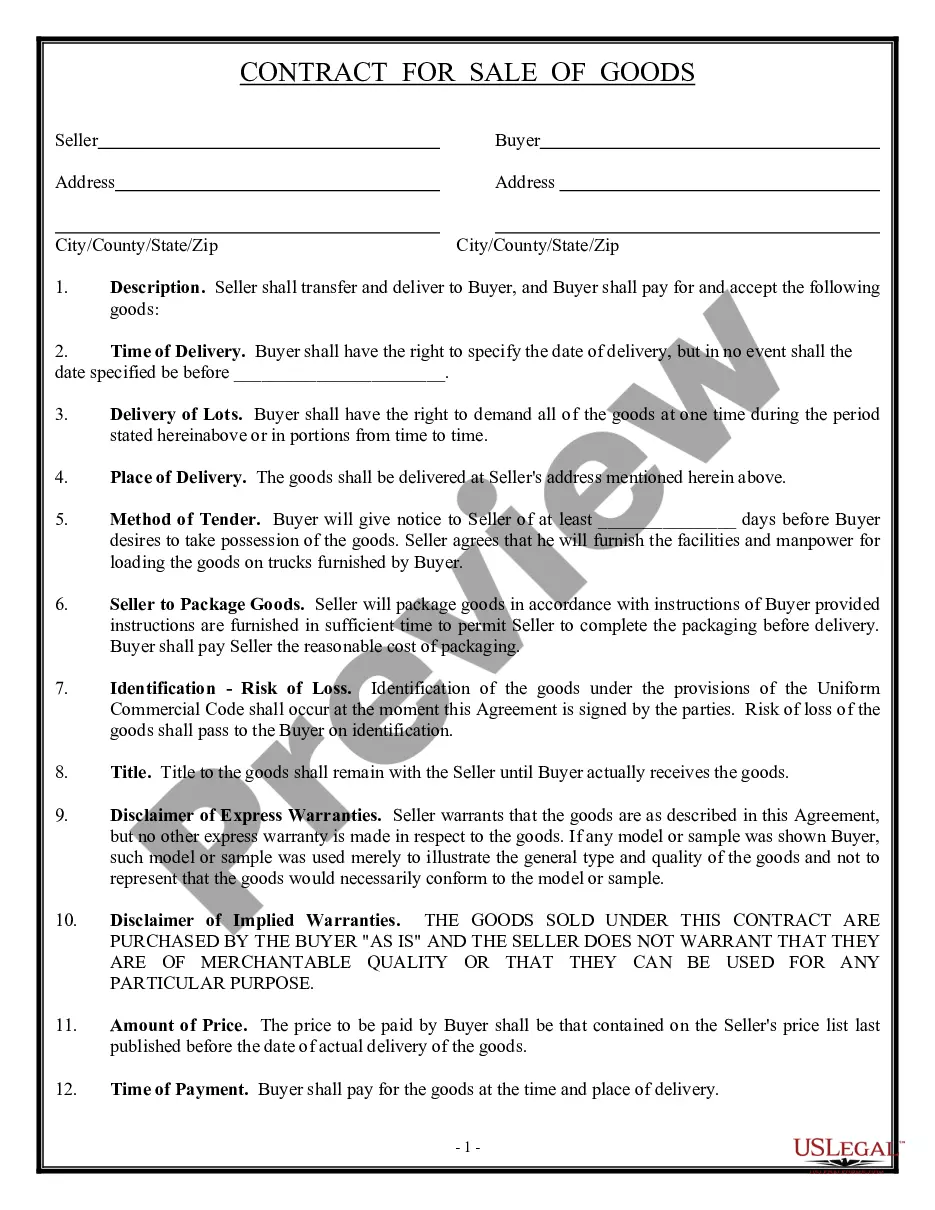
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.