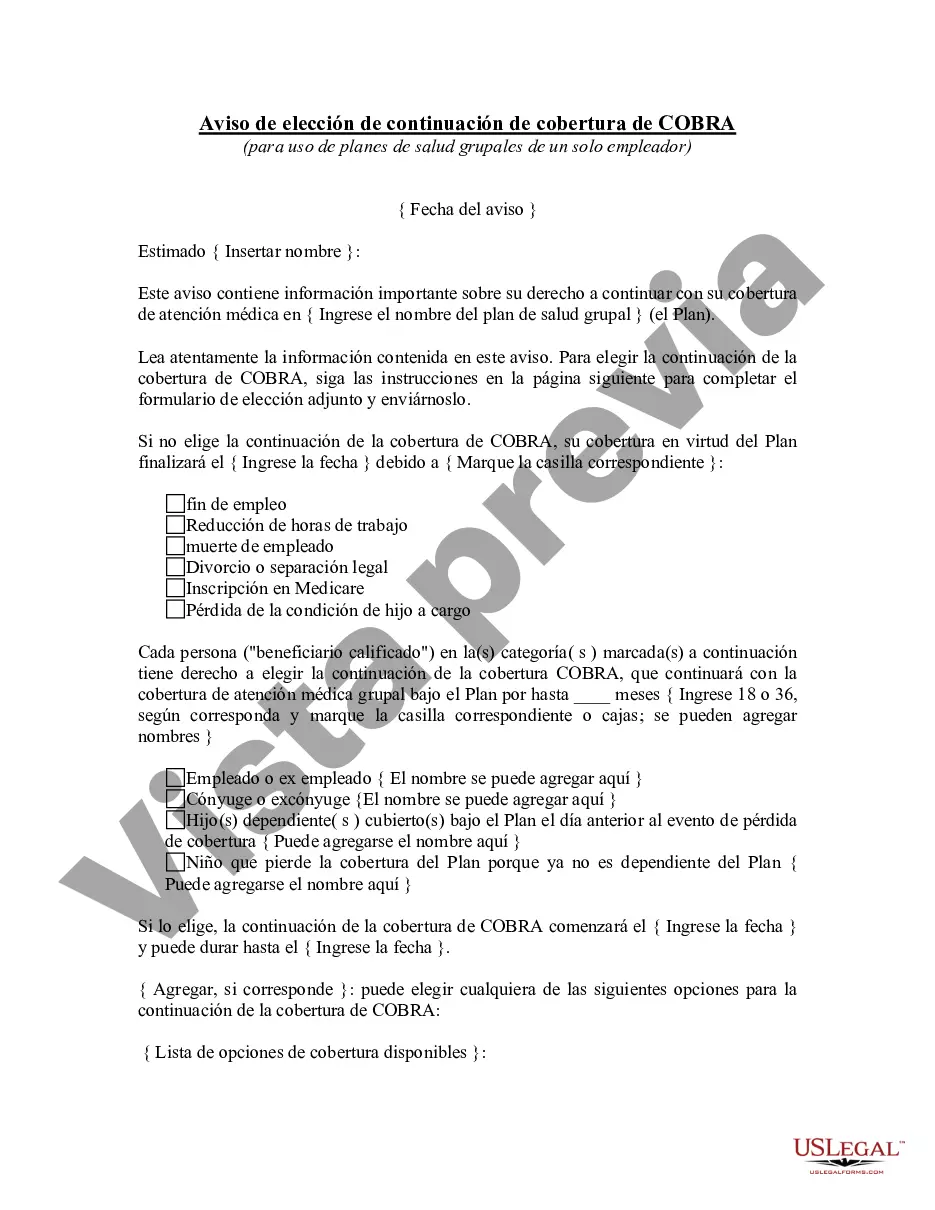
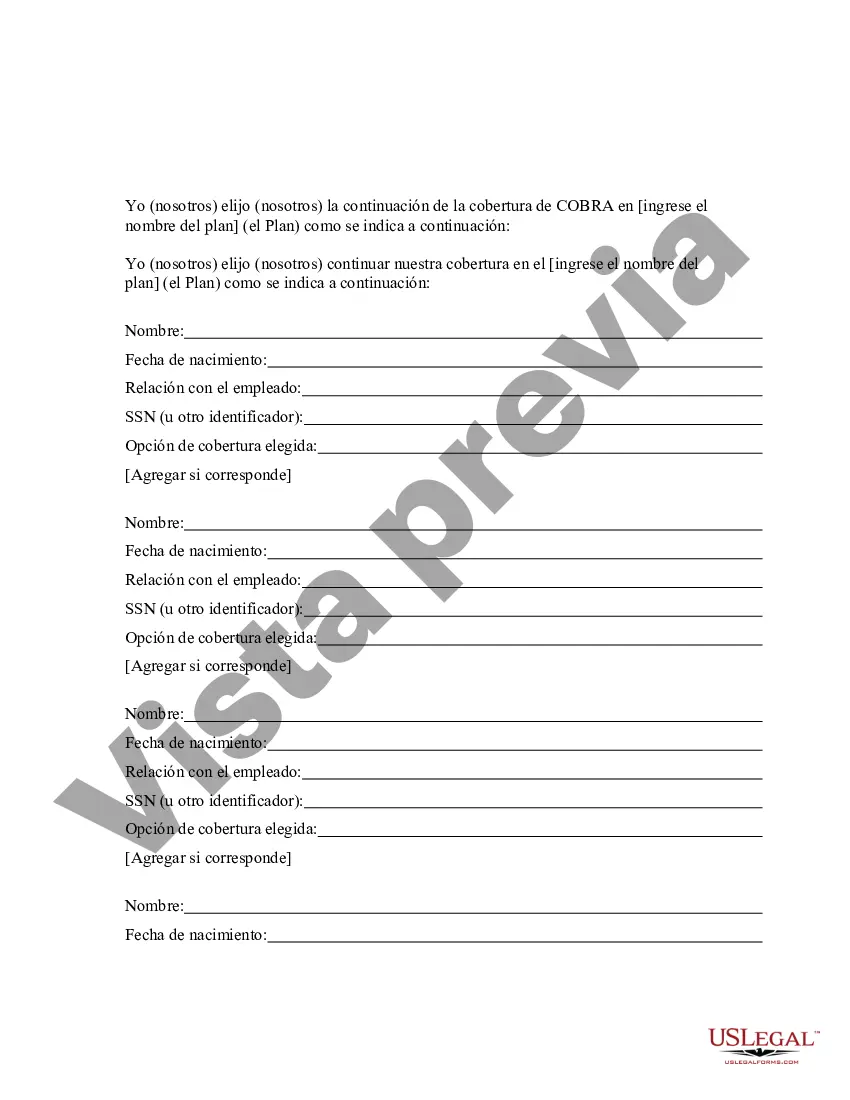
Hennepin County, Minnesota COBRA Continuation Coverage Election Notice is an important document provided to individuals who have experienced a qualifying event that results in the loss of their employer-sponsored health insurance coverage. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, enables eligible employees and their dependents to continue their health insurance coverage for a certain period of time. The Hennepin Minnesota COBRA Continuation Coverage Election Notice serves as a notice to inform individuals about their rights, options, and responsibilities when it comes to continuing their health insurance coverage. It includes crucial information regarding enrollment deadlines, premium costs, coverage details, and how to elect for COBRA coverage. Keywords: Hennepin County, Minnesota, COBRA, Continuation Coverage, Election Notice, health insurance, qualifying event, employer-sponsored, coverage, individuals, dependents, rights, options, responsibilities, enrollment deadlines, premium costs, coverage details, elect, COBRA coverage. Different types of Hennepin Minnesota COBRA Continuation Coverage Election Notice might include: 1. Comprehensive COBRA Continuation Coverage Election Notice: This notice provides detailed information about all aspects of COBRA continuation coverage, including eligibility requirements, coverage period, premium costs, options for adding dependents, and the steps to take to elect for COBRA coverage. 2. Termination of Employment COBRA Continuation Coverage Election Notice: This notice specifically addresses employees who have lost their health insurance coverage due to the termination of their employment. It outlines the necessary steps to maintain health insurance coverage through COBRA, such as the timeframe for electing coverage and premium payment information. 3. Divorce or Legal Separation COBRA Continuation Coverage Election Notice: Designed for individuals who lost their health insurance coverage due to divorce or legal separation, this notice explains the options available for continuing health insurance coverage under COBRA. It provides details about the process of electing coverage, including deadlines and premium payment instructions. 4. Dependent Aging Out COBRA Continuation Coverage Election Notice: This notice is applicable to dependent children who have aged out of their parent's health insurance coverage. It informs them about their rights to continue their health insurance coverage under COBRA and provides them with the necessary information to make an informed decision regarding their coverage. Keywords: Termination of Employment, divorce, legal separation, dependent aging out, coverage period, eligibility requirements, premium payment, dependents, electing coverage, options, health insurance coverage, COBRA continuation coverage.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Hennepin Minnesota Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
How to fill out Hennepin Minnesota Aviso De Elección De Continuación De Cobertura De COBRA?
Preparing legal paperwork can be burdensome. In addition, if you decide to ask a legal professional to draft a commercial contract, documents for proprietorship transfer, pre-marital agreement, divorce paperwork, or the Hennepin COBRA Continuation Coverage Election Notice, it may cost you a lot of money. So what is the best way to save time and money and draw up legitimate documents in total compliance with your state and local regulations? US Legal Forms is an excellent solution, whether you're searching for templates for your personal or business needs.
US Legal Forms is biggest online collection of state-specific legal documents, providing users with the up-to-date and professionally checked forms for any scenario collected all in one place. Therefore, if you need the current version of the Hennepin COBRA Continuation Coverage Election Notice, you can easily find it on our platform. Obtaining the papers requires a minimum of time. Those who already have an account should check their subscription to be valid, log in, and pick the sample using the Download button. If you haven't subscribed yet, here's how you can get the Hennepin COBRA Continuation Coverage Election Notice:
- Look through the page and verify there is a sample for your area.
- Check the form description and use the Preview option, if available, to make sure it's the sample you need.
- Don't worry if the form doesn't satisfy your requirements - look for the correct one in the header.
- Click Buy Now when you find the needed sample and select the best suitable subscription.
- Log in or register for an account to pay for your subscription.
- Make a transaction with a credit card or via PayPal.
- Opt for the file format for your Hennepin COBRA Continuation Coverage Election Notice and download it.
Once done, you can print it out and complete it on paper or upload the template to an online editor for a faster and more convenient fill-out. US Legal Forms allows you to use all the documents ever obtained many times - you can find your templates in the My Forms tab in your profile. Try it out now!