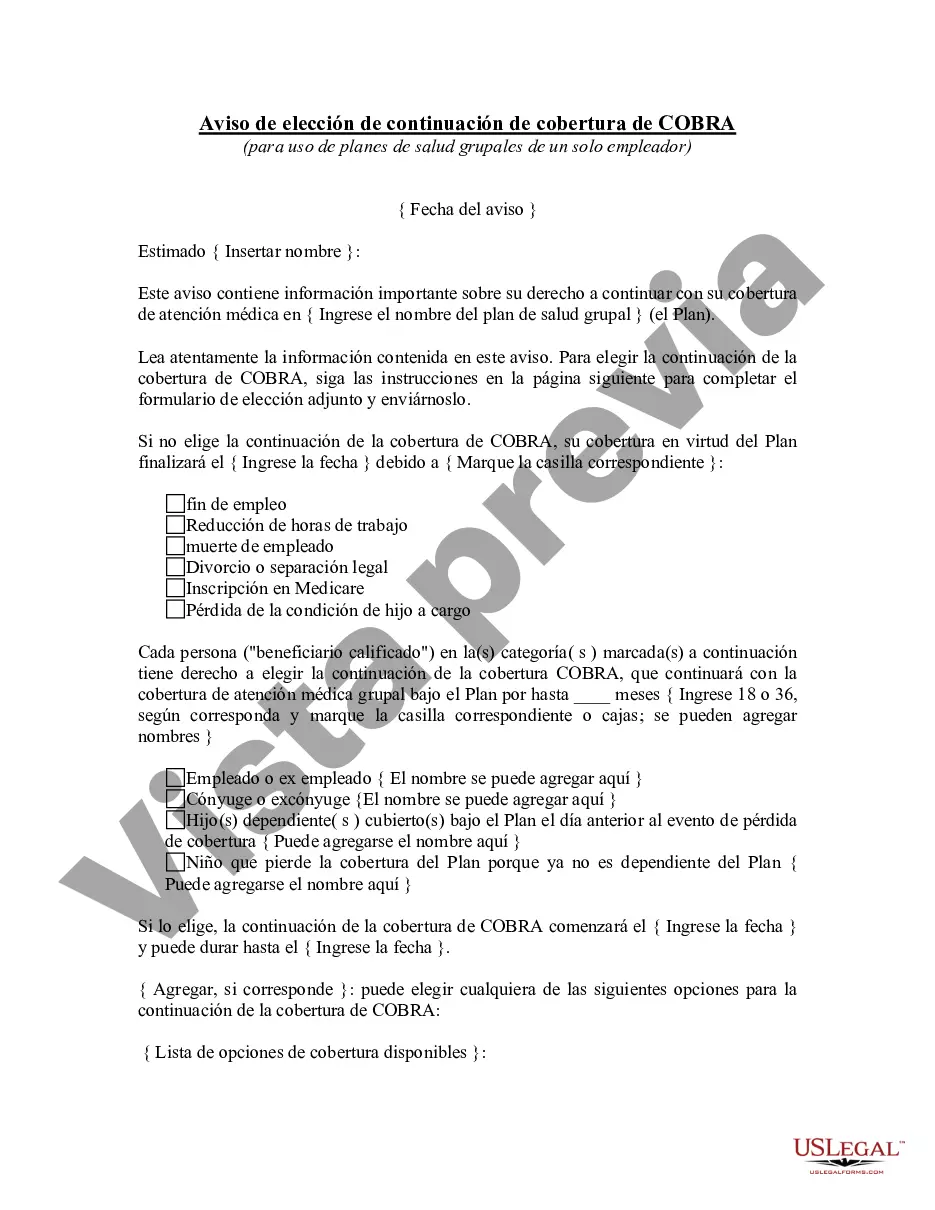
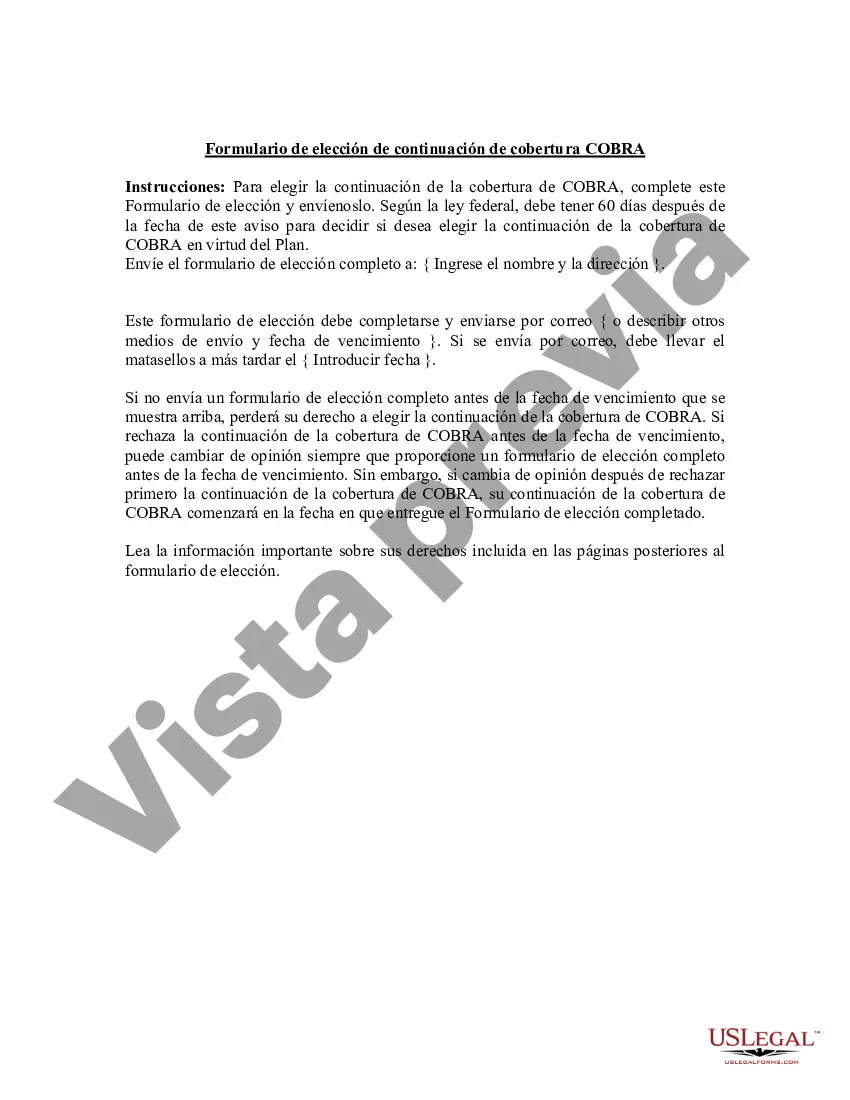
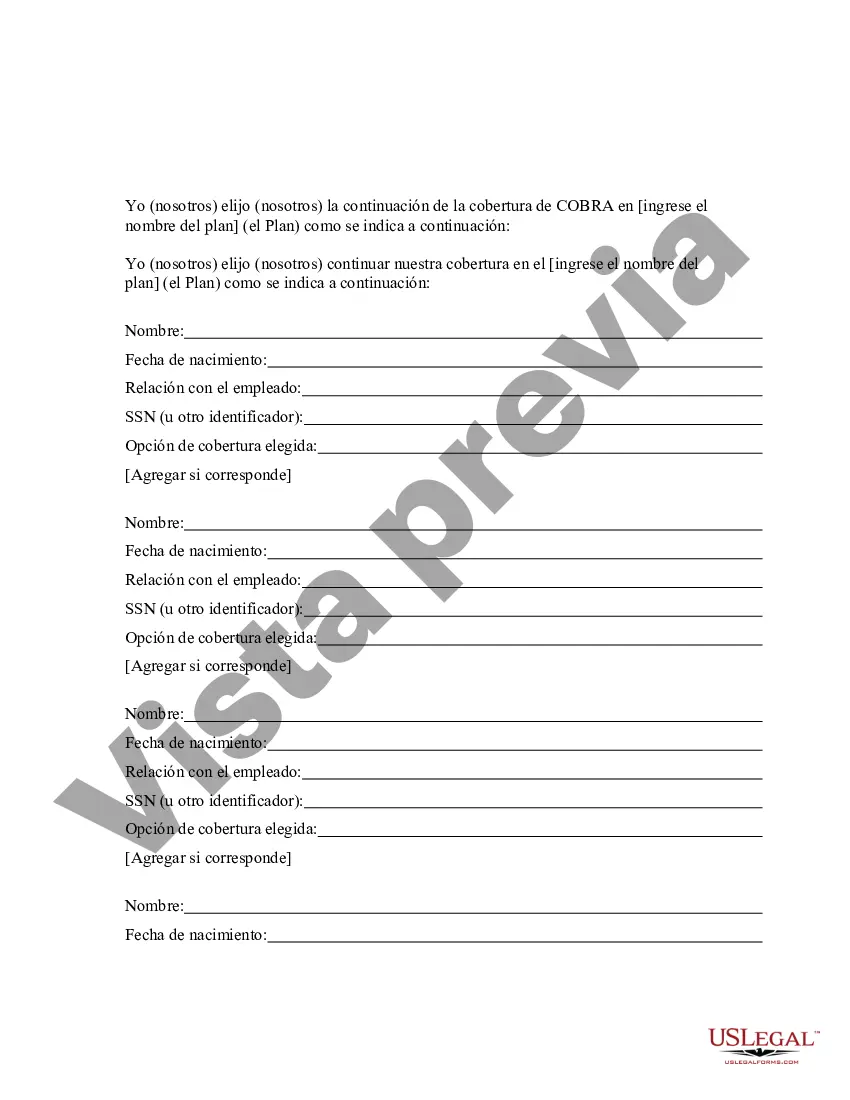
Houston Texas COBRA Continuation Coverage Election Notice is a document that provides crucial information to individuals and their dependents when they experience a qualifying event that may lead to a loss of group health insurance coverage. This notice is essential for ensuring that individuals have the option to continue their health insurance coverage for a specified period of time, even after leaving their job or experiencing another qualifying event. The Houston Texas COBRA Continuation Coverage Election Notice contains detailed information about the COBRA continuation coverage options available to eligible individuals. It includes relevant dates, instructions, and how to elect and pay for coverage. This notice is typically sent by the employer or the health insurance plan administrator to the eligible individuals and their dependents within a specified timeframe after the qualifying event occurs. There are a few variations or types of COBRA Continuation Coverage Election Notice that may be issued based on the circumstances. These may include: 1. General COBRA Continuation Coverage Election Notice: This type of notice is sent to eligible individuals who experience a qualifying event that results in a loss of group health insurance coverage. It provides an overview of the COBRA continuation coverage rights and options available to these individuals. 2. COBRA Continuation Coverage Election Notice for Dependents: This notice specifically addresses qualified dependents who are eligible for COBRA continuation coverage due to the covered employee's qualifying event. It outlines the coverage options and enrollment procedures for these dependents. 3. COBRA Continuation Coverage Election Notice for Divorced Spouses: In cases of divorce or legal separation, this notice is sent to former spouses who were covered under the employee's group health insurance plan. It includes specific details about the COBRA continuation coverage rights and obligations for the divorced spouse. 4. COBRA Continuation Coverage Election Notice for Disabled Individuals: This type of notice is designed for individuals who become disabled during the initial COBRA continuation coverage period. It explains the extended coverage duration and additional requirements for disabled individuals. 5. COBRA Continuation Coverage Election Notice for Retirees: When an employee retires and loses group health insurance coverage, this notice is sent to inform them about the COBRA continuation coverage options available during retirement. It includes information about the coverage duration and any applicable premium rates. These various types of Houston Texas COBRA Continuation Coverage Election Notices ensure that eligible individuals and their dependents are well-informed about their rights, options, and necessary steps to continue their health insurance coverage. It is important for recipients of these notices to carefully review the information provided and follow the outlined procedures to secure the continuation of their health insurance benefits.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Houston Texas Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
How to fill out Houston Texas Aviso De Elección De Continuación De Cobertura De COBRA?
How much time does it normally take you to create a legal document? Given that every state has its laws and regulations for every life situation, locating a Houston COBRA Continuation Coverage Election Notice suiting all local requirements can be tiring, and ordering it from a professional attorney is often costly. Many web services offer the most common state-specific templates for download, but using the US Legal Forms library is most advantegeous.
US Legal Forms is the most extensive web collection of templates, grouped by states and areas of use. Aside from the Houston COBRA Continuation Coverage Election Notice, here you can get any specific form to run your business or individual deeds, complying with your county requirements. Experts verify all samples for their actuality, so you can be certain to prepare your documentation properly.
Using the service is pretty easy. If you already have an account on the platform and your subscription is valid, you only need to log in, pick the needed sample, and download it. You can retain the file in your profile at any time later on. Otherwise, if you are new to the website, there will be a few more steps to complete before you obtain your Houston COBRA Continuation Coverage Election Notice:
- Examine the content of the page you’re on.
- Read the description of the sample or Preview it (if available).
- Look for another form utilizing the corresponding option in the header.
- Click Buy Now once you’re certain in the selected file.
- Select the subscription plan that suits you most.
- Create an account on the platform or log in to proceed to payment options.
- Make a payment via PalPal or with your credit card.
- Switch the file format if necessary.
- Click Download to save the Houston COBRA Continuation Coverage Election Notice.
- Print the sample or use any preferred online editor to fill it out electronically.
No matter how many times you need to use the acquired document, you can locate all the files you’ve ever downloaded in your profile by opening the My Forms tab. Try it out!