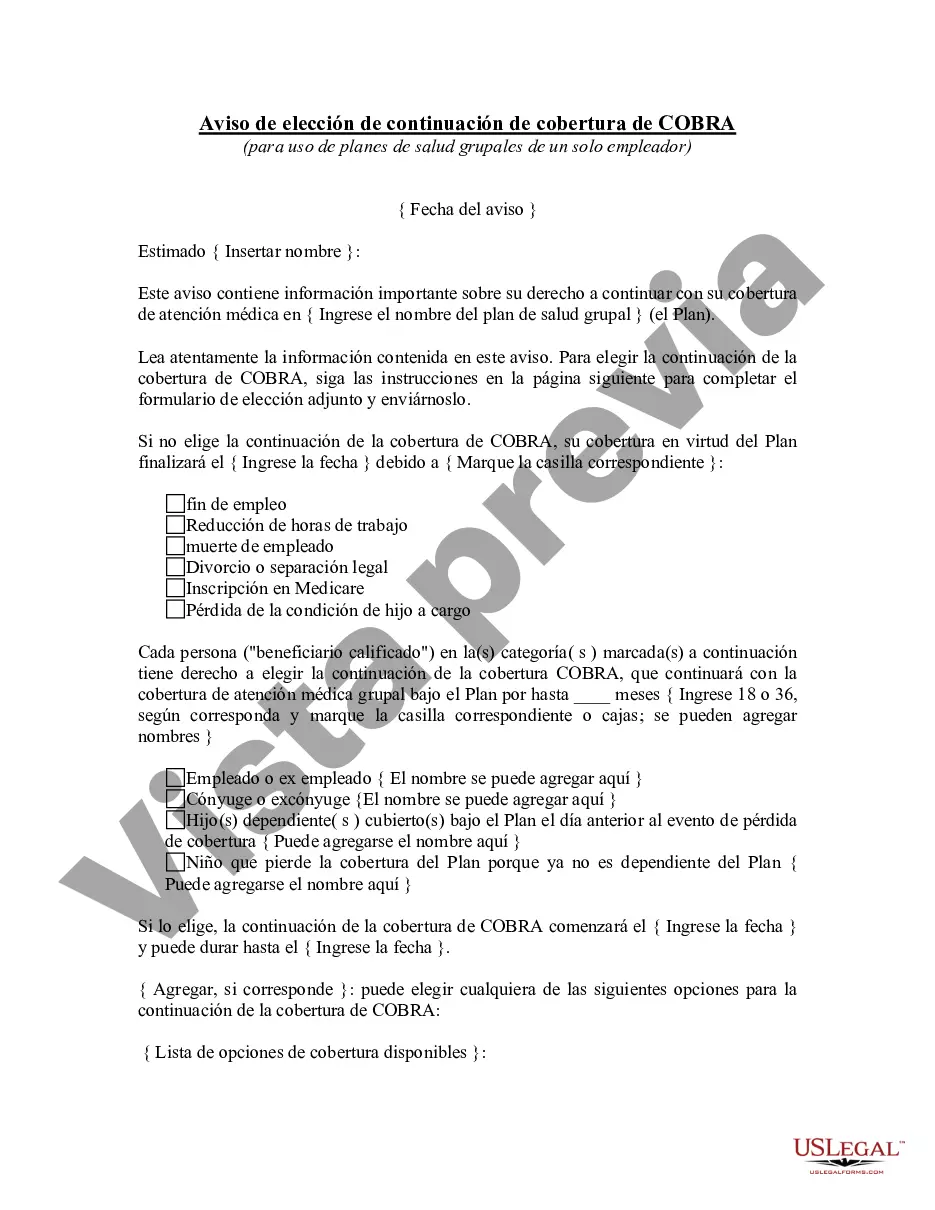
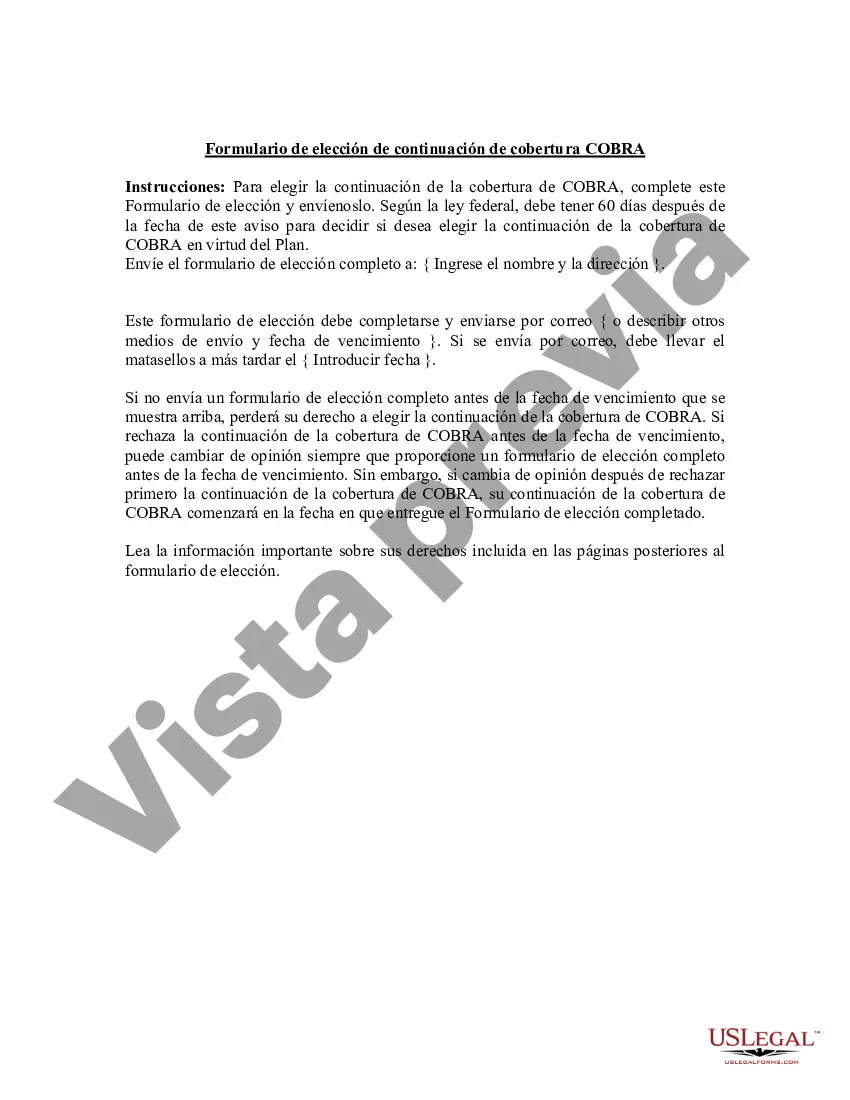
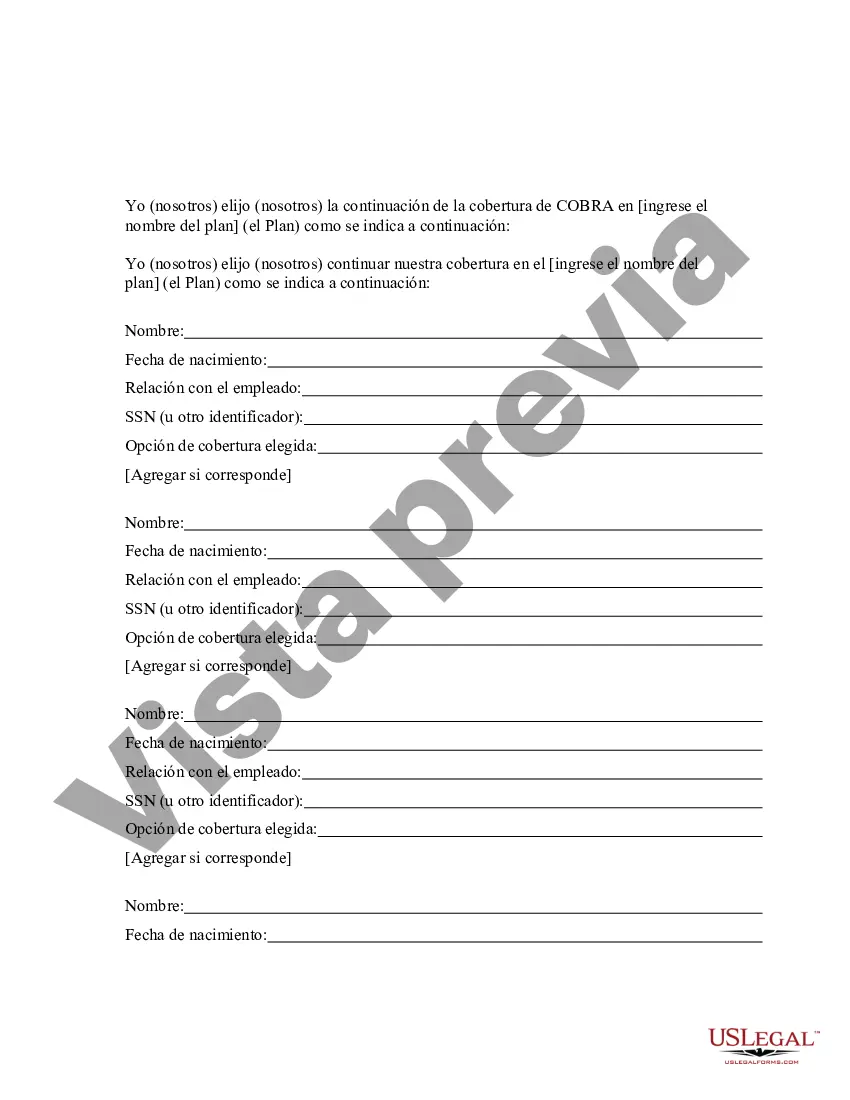
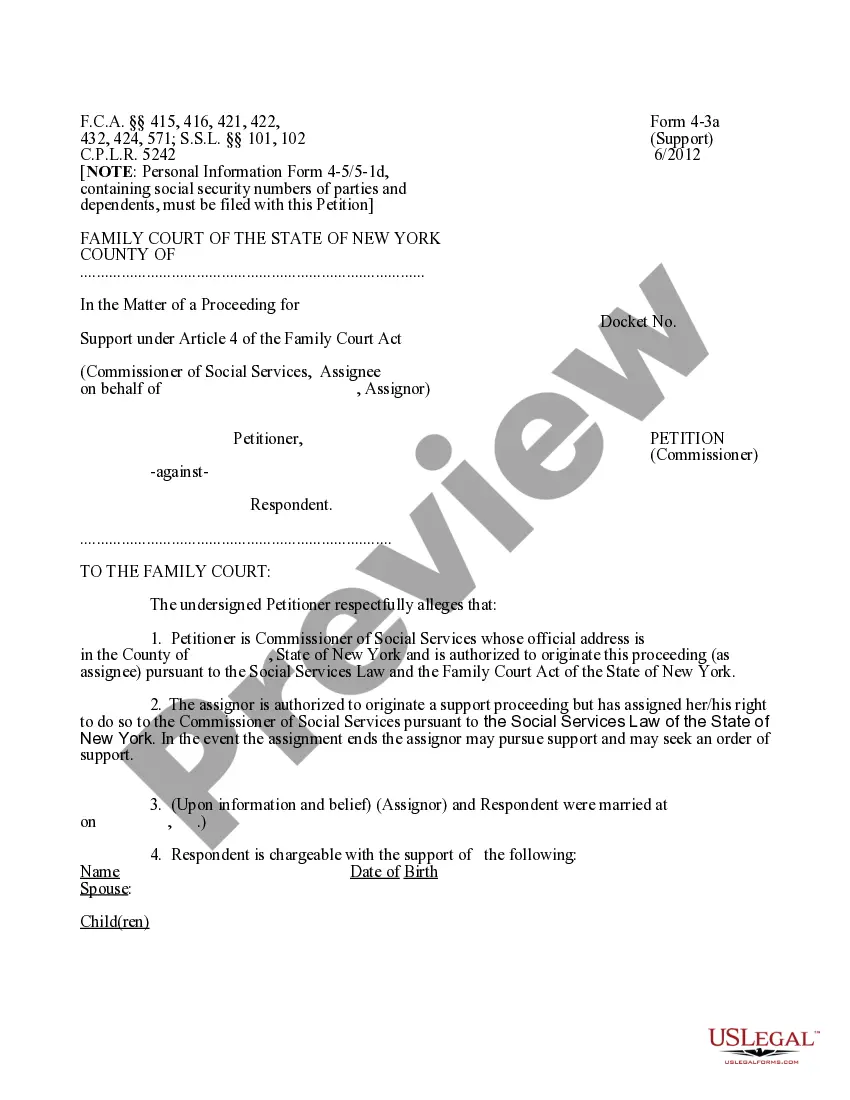
San Diego California COBRA Continuation Coverage Election Notice is a critical document that provides important information to employees and their eligible dependents about their rights to continue health insurance coverage after a qualifying event. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, ensures that individuals can maintain their healthcare benefits temporarily even if they would otherwise lose coverage due to specific circumstances such as job loss, reduction in hours, divorce, or other qualifying events. The San Diego California COBRA Continuation Coverage Election Notice serves as a formal notification to eligible individuals regarding their option to elect continuation coverage. It outlines the rights and responsibilities of the individual, including the process and deadlines for making an election, the duration and cost of coverage, and the consequences of not electing COBRA coverage within the specified timeframe. There are various types of San Diego California COBRA Continuation Coverage Election Notices, which may include: 1. General Notice: This notice is provided to all covered employees and their dependents at the time of initial plan enrollment or within the first 90 days of coverage. It provides a comprehensive overview of COBRA rights and obligations, explaining who is eligible for continuation coverage and the steps involved in electing COBRA. 2. Qualifying Event Notice: This notice is sent to employees and their dependents when a qualifying event occurs, such as termination of employment, reduction in hours, divorce or legal separation, or death of the covered employee. It provides specific information about the qualifying event, the individuals who are entitled to elect continuation coverage, and the deadline for making an election. 3. Disability Notice (Extension of Maximum Coverage Period): In certain cases, qualified individuals with a disability may be eligible for an extension of the maximum COBRA coverage period. This notice informs eligible individuals about the criteria for disability extension, the required documentation, and the process for requesting an extension. 4. Termination of Coverage Notice: If COBRA continuation coverage is terminated before the maximum coverage period expires, this notice is sent to affected individuals. It outlines the reason for the termination, the options available for obtaining alternative coverage, and any rights individuals may have under other healthcare laws. It is crucial for employers, plan administrators, and individuals in San Diego, California, to understand and comply with the rules and regulations governing COBRA continuation coverage to ensure seamless and uninterrupted health insurance during times of transition or crisis. The San Diego California COBRA Continuation Coverage Election Notice plays a crucial role in informing individuals about their rights and responsibilities, empowering them to make informed decisions about their healthcare coverage.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.San Diego California Aviso de elección de continuación de cobertura de COBRA - COBRA Continuation Coverage Election Notice
Description
How to fill out San Diego California Aviso De Elección De Continuación De Cobertura De COBRA?
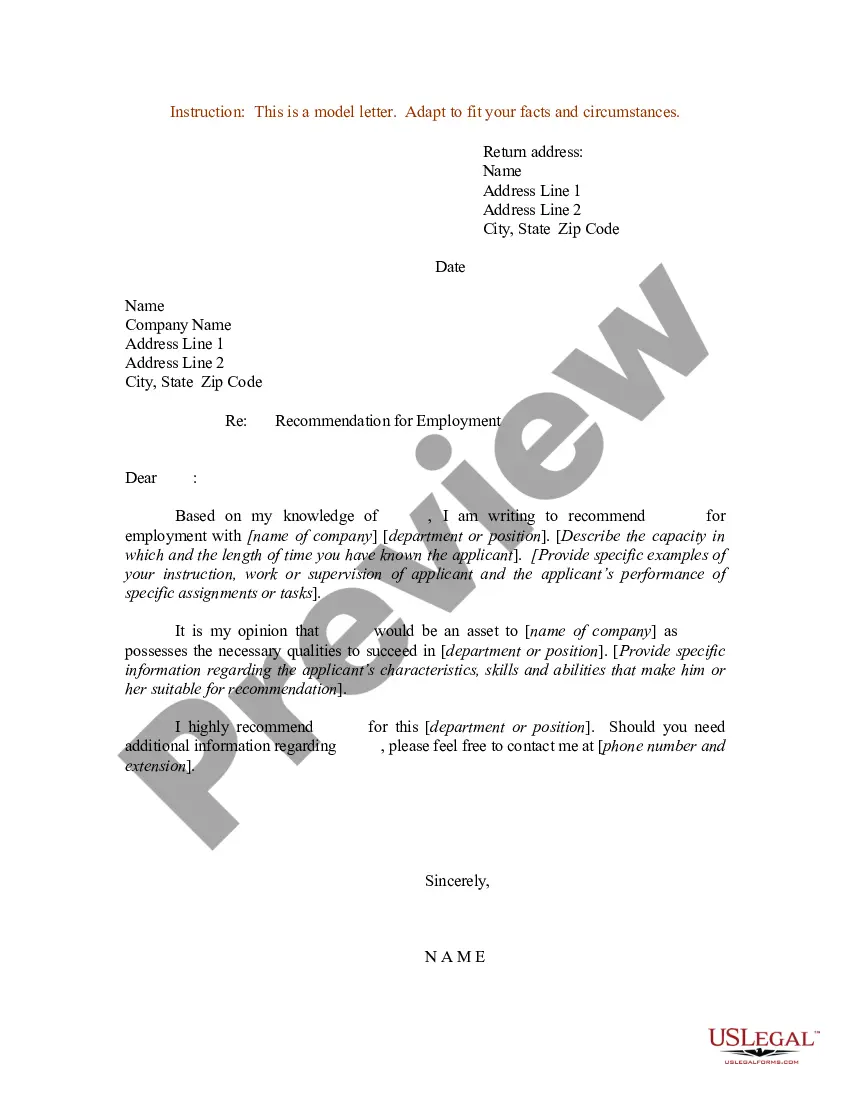
A document routine always accompanies any legal activity you make. Creating a business, applying or accepting a job offer, transferring property, and lots of other life scenarios require you prepare formal documentation that differs from state to state. That's why having it all collected in one place is so helpful.
US Legal Forms is the largest online collection of up-to-date federal and state-specific legal forms. On this platform, you can easily find and get a document for any personal or business purpose utilized in your region, including the San Diego COBRA Continuation Coverage Election Notice.
Locating forms on the platform is extremely straightforward. If you already have a subscription to our library, log in to your account, find the sample through the search field, and click Download to save it on your device. After that, the San Diego COBRA Continuation Coverage Election Notice will be available for further use in the My Forms tab of your profile.
If you are dealing with US Legal Forms for the first time, adhere to this quick guide to obtain the San Diego COBRA Continuation Coverage Election Notice:
- Make sure you have opened the correct page with your localised form.
- Use the Preview mode (if available) and scroll through the template.
- Read the description (if any) to ensure the form satisfies your needs.
- Search for another document via the search tab in case the sample doesn't fit you.
- Click Buy Now when you find the required template.
- Select the appropriate subscription plan, then sign in or register for an account.
- Select the preferred payment method (with credit card or PayPal) to proceed.
- Choose file format and save the San Diego COBRA Continuation Coverage Election Notice on your device.
- Use it as needed: print it or fill it out electronically, sign it, and file where requested.
This is the easiest and most reliable way to obtain legal documents. All the samples available in our library are professionally drafted and verified for correspondence to local laws and regulations. Prepare your paperwork and manage your legal affairs effectively with the US Legal Forms!
Form popularity
FAQ
Cualquier plan de seguro que cumpla con el requisito de la Ley del Cuidado de Salud de Bajo Precio para tener cobertura de salud.
Si cubriste sin interrupcion un minimo de ocho cotizaciones semanales antes de perder tu trabajo, tu y tus beneficiarios tienen derecho a recibir asistencia medica y de maternidad, quirurgica, farmaceutica y hospitalaria durante las ocho semanas posteriores a tu baja del empleo.
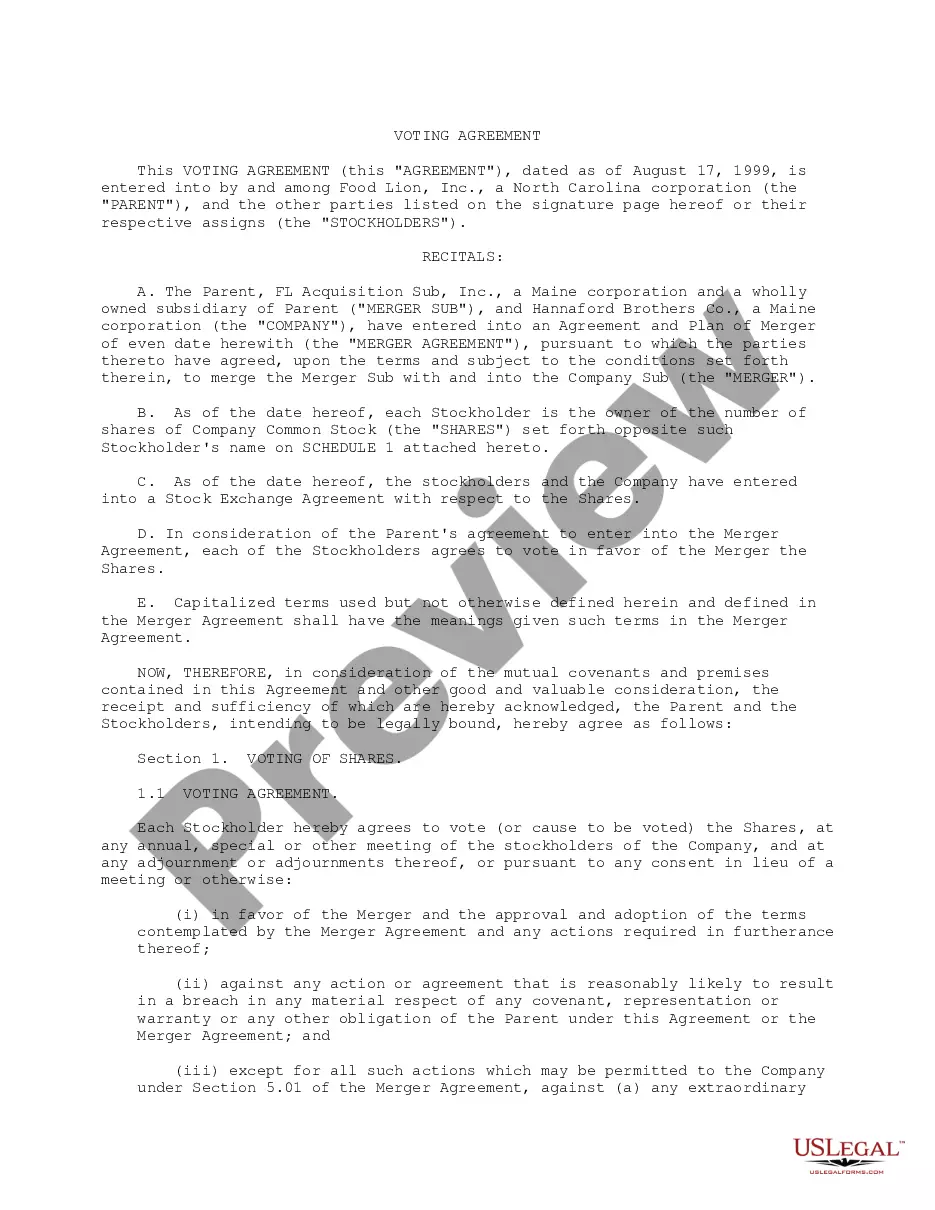
COBRA establece reglas acerca de como y cuando debera ofrecerse y proporcionarse continuacion de cobertura, como pueden elegir los empleados y sus familias la continuacion de cobertura y cuales circunstancias justifican cancelar la continuacion de cobertura.
La ley COBRA provee a las personas en ciertas circunstancias la opcion de conservar el seguro medico obtenido con un empleador por una extension de tiempo adicional tras haber dejado de trabajar en caso de no poder obtener cobertura a traves del empleo de sus conyuges ni en el mercado de seguros medicos.
Las personas que se encuentran desempleadas pueden atenderse con el seguro de EsSalud durante unos meses despues de haber finalizado el vinculo laboral. A este derecho se le llama periodo de latencia y va depender de la cantidad de aportes que haya realizado el empleador.
Winston Santos, informo este martes que todos los trabajadores suspendidos y sus dependientes directos y adicionales, conservaran su afiliacion al Seguro Familiar de Salud (SFS), por un periodo de 60 dias, dicha medida esta contenida en la Resolucion No.
Es decir, en el momento en que una persona es separada de esa prestacion empiezan a contar las ocho semanas y justo al terminar, un aproximado de dos meses, ya no podra hacer uso de ningun servicio en el IMSS.
En 1985, el gobierno de los Estados Unidos aprobo la Ley Omnibus Consolidada de Reconciliacion Presupuestaria o COBRA, para abreviar.
More info
A woman, left, and a man, center, stand in line to get into the Republican National Convention to cast their ballots. 3 of 5File An employee looks over a voting machine at the U.S. Elections Office in Arlington on Sunday, April 13, 2022. FILE The Twitter application is seen on a digital device, Sunday, April 13, 2022, in San Diego. An employee in the booth that prints ballots looks over the printer, Thursday, March 5, 2023, during a preview of the U.S. Election Office. File U.S. Senator Bernie Sanders addresses the media during a press conference at the U.S. Elections Office, in Arlington, Texas on Friday, March 9, 2023. 10 of 14File Photo taken from the front row seats of the San Diego Convention Center at the start and finish of the 2016 Democratic National Convention in San. Diego on July 23, 2016. 10 of 14File This is an artist's rendering of an electoral vote tally on Jan. 20, 2024, at the Alamo Draft house Hollywood. File A picture taken on Feb. 18, 2024, shows the U.S.
Disclaimer
The materials in this section are taken from public sources. We disclaim all representations or any warranties, express or implied, as to the accuracy, authenticity, reliability, accessibility, adequacy, or completeness of any data in this paragraph. Nevertheless, we make every effort to cite public sources deemed reliable and trustworthy.