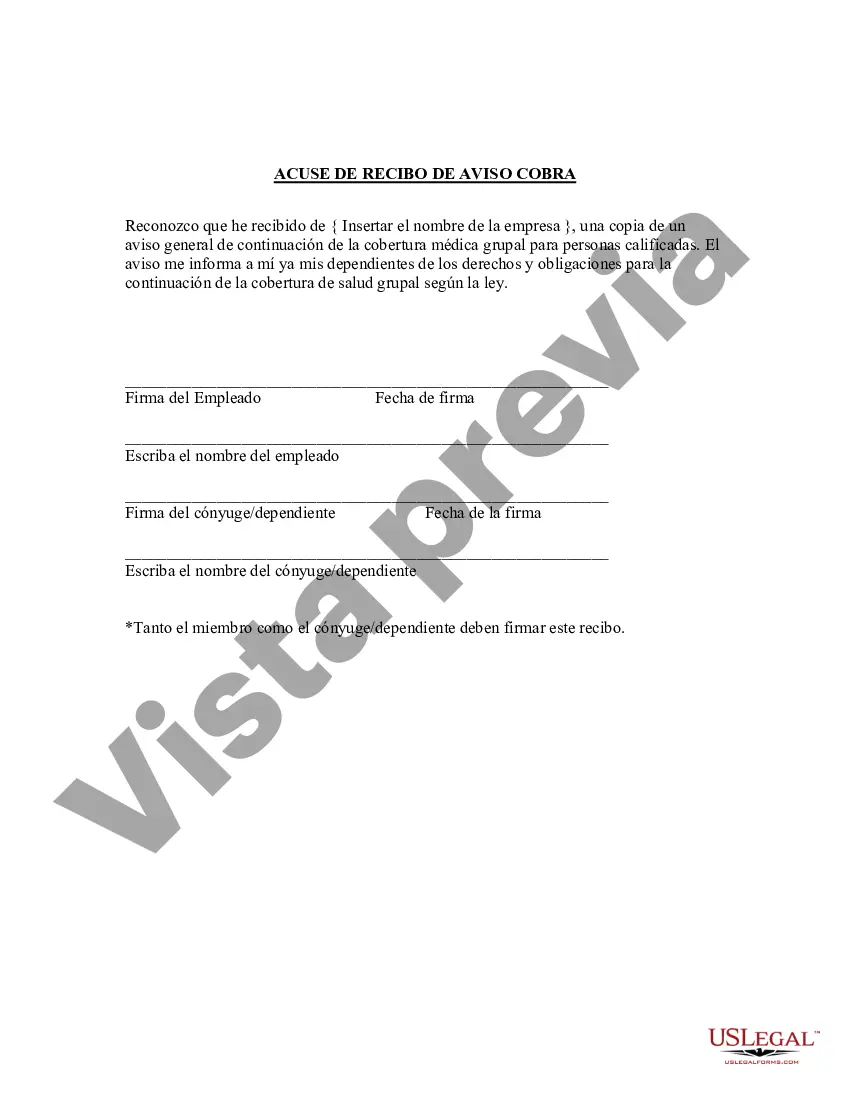
Title: Alameda California Acknowledgment of Receipt of COBRA Notice: Understanding your Rights and Benefits Introduction: In Alameda, California, the Acknowledgment of Receipt of COBRA (Consolidated Omnibus Budget Reconciliation Act) Notice plays a crucial role in ensuring that employees and their dependents are well-informed about their healthcare continuation rights. This detailed description aims to provide comprehensive information about the COBRA Notice in Alameda and its significance in safeguarding individuals' access to healthcare coverage. We will also explore any potential variations or types of COBRA Notices applicable to specific circumstances. 1. What is Alameda California Acknowledgment of Receipt of COBRA Notice? The Alameda California Acknowledgment of Receipt of COBRA Notice is a legally mandated document that serves as proof of receipt for the COBRA Notice provided to eligible employees and their qualified beneficiaries. This notice outlines the employee's rights and responsibilities in continuing their employer-sponsored health insurance benefits after certain qualifying events, such as termination, reduction of work hours, or divorce. 2. Key Elements of the Acknowledgment of Receipt of COBRA Notice: The Acknowledgment of Receipt of COBRA Notice typically includes the following essential information: — Employee details: Name, address, contact information, and the employer's name. — Qualifying event: A clear description of the event that triggered the COBRA coverage, such as termination, reduction in hours, etc. — COBRA benefits: Explanation of the continuation coverage options, duration, and associated costs. — Deadline for election: A specific timeframe within which the employee or qualified beneficiary must respond to elect COBRA coverage. Failure to meet the deadline may result in loss of benefits. — Contact information: Details of the plan administrator or the party responsible for administering COBRA benefits, including their address and contact information. 3. Importance of the Acknowledgment of Receipt of COBRA Notice: The Acknowledgment of Receipt of COBRA Notice carries significant importance for both employers and employees. Here are some key reasons why it is crucial: — Legal compliance: Employers are legally required to provide the COBRA Notice to eligible employees and qualified beneficiaries to ensure they are aware of their rights to continue their healthcare coverage. — Notification and information: The notice acts as a clear and concise informational tool, providing employees with details about their COBRA rights, options, and responsibilities. — Record-keeping: The acknowledgment serves as documented evidence that the COBRA Notice was received by the employee or qualified beneficiary, protecting both parties' rights and interests. Types of Alameda California Acknowledgment of Receipt of COBRA Notice: While there may not be specific variations or types of Acknowledgment of Receipt of COBRA Notice that are unique to Alameda, California, different templates may be used based on the employer or plan administrator's preferences. However, the content and purpose of the notice remain consistent across these variations. Conclusion: In Alameda, California, the Acknowledgment of Receipt of COBRA Notice ensures that employees and their qualified beneficiaries are well-informed about their healthcare continuation rights. This legally mandated notification acts as a vital tool in safeguarding individuals' access to healthcare coverage during qualifying events. Employers must carefully administer the notice, emphasizing the importance of receiving acknowledgment in a timely manner.
Para su conveniencia, debajo del texto en español le brindamos la versión completa de este formulario en inglés. For your convenience, the complete English version of this form is attached below the Spanish version.Alameda California Acuse de recibo de la notificación COBRA - Acknowledgment of Receipt of COBRA Notice
Description
How to fill out Alameda California Acuse De Recibo De La Notificación COBRA?
Preparing papers for the business or individual demands is always a huge responsibility. When creating a contract, a public service request, or a power of attorney, it's crucial to take into account all federal and state laws and regulations of the specific region. Nevertheless, small counties and even cities also have legislative provisions that you need to consider. All these aspects make it stressful and time-consuming to draft Alameda Acknowledgment of Receipt of COBRA Notice without professional assistance.
It's easy to avoid spending money on attorneys drafting your paperwork and create a legally valid Alameda Acknowledgment of Receipt of COBRA Notice on your own, using the US Legal Forms web library. It is the most extensive online catalog of state-specific legal documents that are professionally cheched, so you can be sure of their validity when choosing a sample for your county. Earlier subscribed users only need to log in to their accounts to save the required document.
In case you still don't have a subscription, follow the step-by-step instruction below to obtain the Alameda Acknowledgment of Receipt of COBRA Notice:
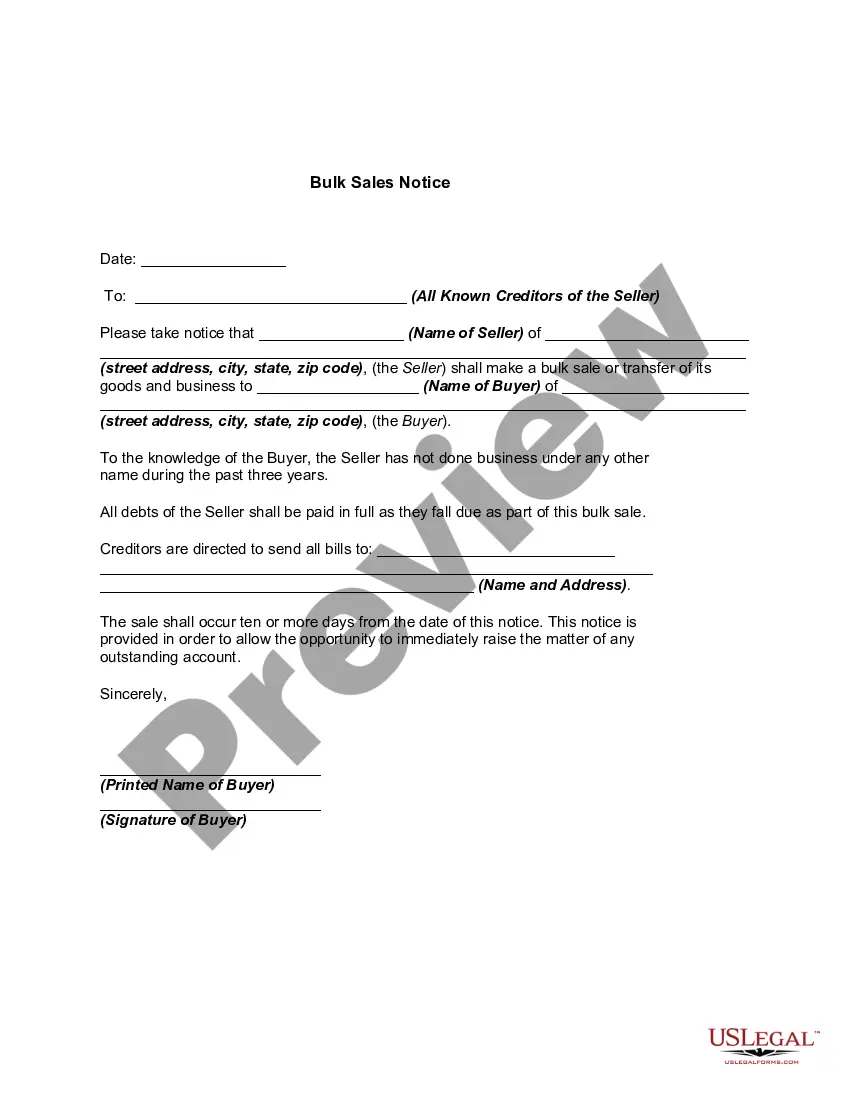
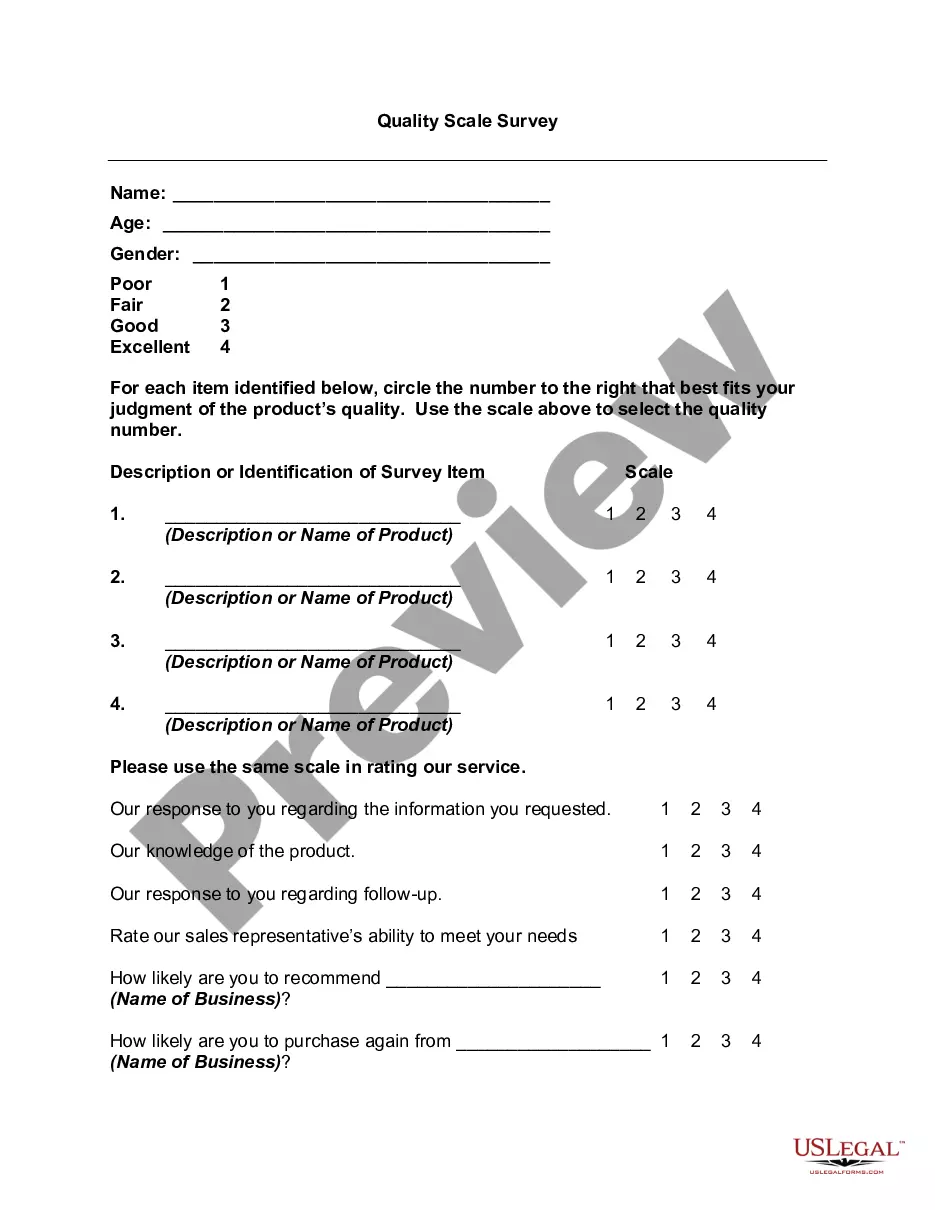
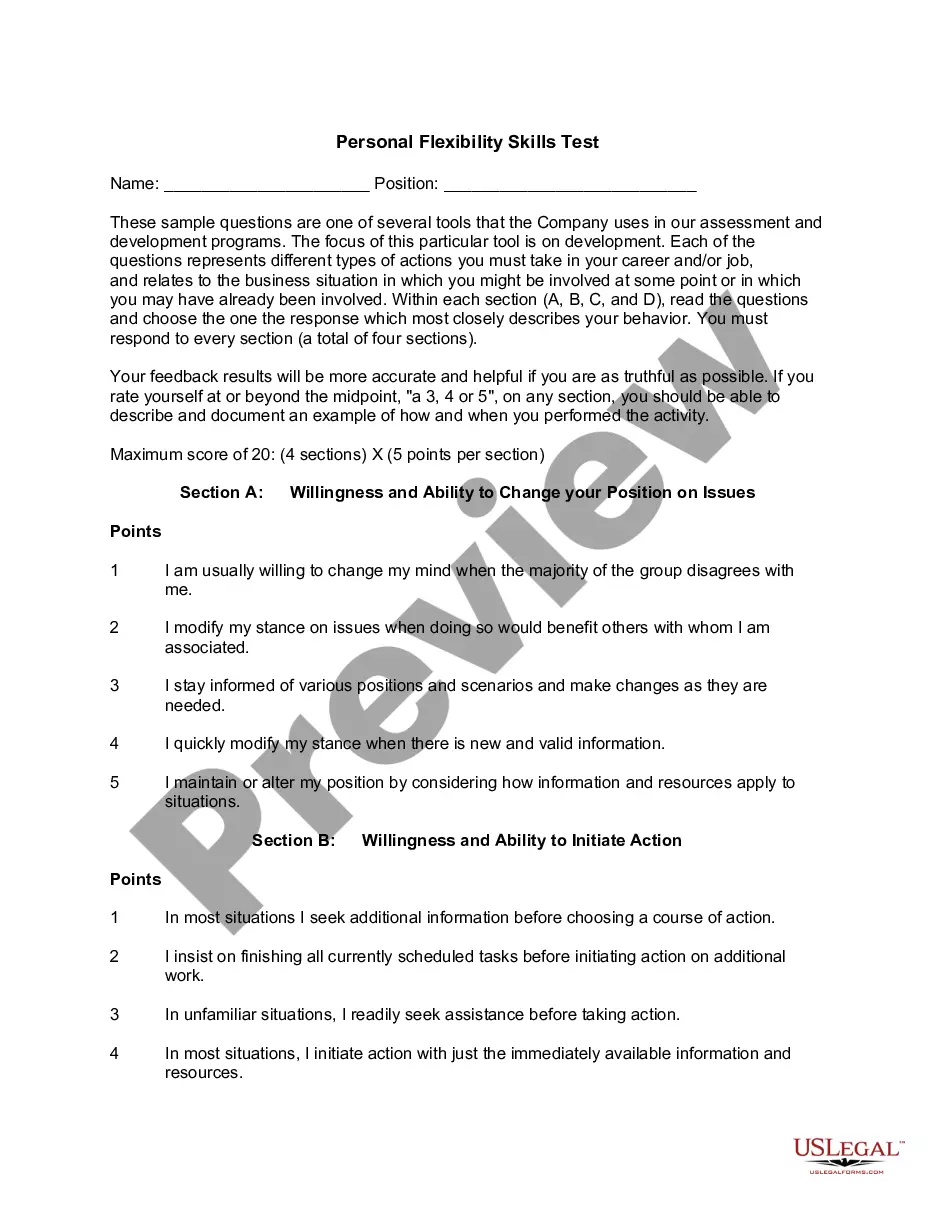
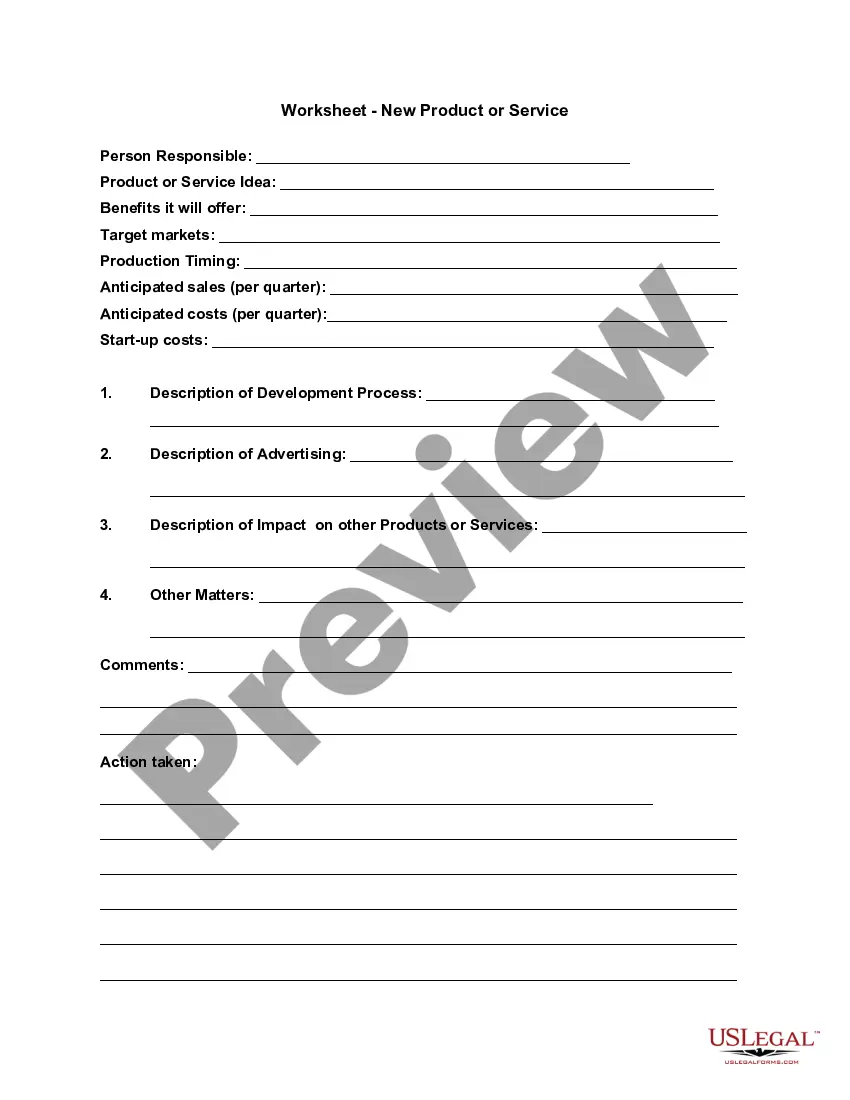
- Examine the page you've opened and check if it has the sample you need.
- To achieve this, use the form description and preview if these options are available.
- To find the one that satisfies your requirements, use the search tab in the page header.
- Double-check that the template complies with juridical standards and click Buy Now.
- Pick the subscription plan, then sign in or create an account with the US Legal Forms.
- Utilize your credit card or PayPal account to pay for your subscription.
- Download the chosen file in the preferred format, print it, or fill it out electronically.
The exceptional thing about the US Legal Forms library is that all the paperwork you've ever acquired never gets lost - you can get it in your profile within the My Forms tab at any moment. Join the platform and easily get verified legal templates for any scenario with just a few clicks!