Cuyahoga County, Ohio, Qualifying Event Notice Information for Employers to Plan Administrators Cuyahoga County, located in the state of Ohio, follows certain guidelines and procedures when it comes to qualifying event notice information for employers to communicate with plan administrators. Qualifying events are specific life events that may trigger changes or adjustments to an employee's benefit plan coverage. Employers in Cuyahoga County have a responsibility to inform their plan administrators promptly about these qualifying events to facilitate smooth transitions and appropriate adjustments to benefit plans. The following are some different types of qualifying events that employers need to provide notice for: 1. Marriage and divorce: When an employee gets married or divorced, both events are considered qualifying events that can affect benefit plan coverage. The employer must notify the plan administrator to make necessary changes in the employee's coverage. 2. Birth or adoption of a child: The birth or adoption of a child is a qualifying event that may require adjustments to the employee's benefit plans, such as adding the child to the healthcare insurance coverage or enrolling them in a dependent care account. Employers need to notify the plan administrator to facilitate these changes. 3. Termination of employment: If an employee's employment is terminated, it is vital for the employer to inform the plan administrator promptly. This allows the plan administrator to offer continuation coverage options, such as COBRA (Consolidated Omnibus Budget Reconciliation Act), to the terminated employee and their eligible dependents. 4. Loss of dependent status: If an employee's dependent no longer qualifies as a dependent under the benefit plan's eligibility criteria, it is necessary for the employer to inform the plan administrator. This helps in ensuring accurate benefit coverage and eligibility determinations. 5. Change in work hours: A significant change in an employee's work hours, such as a reduction or increase in hours that affects their eligibility for certain benefits, is a qualifying event. Employers are responsible for notifying the plan administrator to adjust the benefit plans accordingly. 6. Enrollment in Medicare or Medicaid: When an employee becomes eligible for Medicare or Medicaid, the employer needs to notify the plan administrator. Such events might trigger adjustments in benefit plans to align with the employee's new coverage options. The Cuyahoga County qualifying event notice information for employers to plan administrators should include relevant details such as the name of the employee, the nature of the qualifying event, the date on which the event occurred, and any supporting documentation that may be applicable (e.g., marriage certificate, birth certificate, etc.). By effectively communicating qualifying events to plan administrators, employers in Cuyahoga County ensure compliance with regulations and provide efficient coordination between employees, employers, and the administrators of various benefit plans. This helps maintain the integrity of benefit plans and ensures employees receive the appropriate coverage during times of significant life changes.
Cuyahoga Ohio Qualifying Event Notice Information for Employer to Plan Administrator
Description
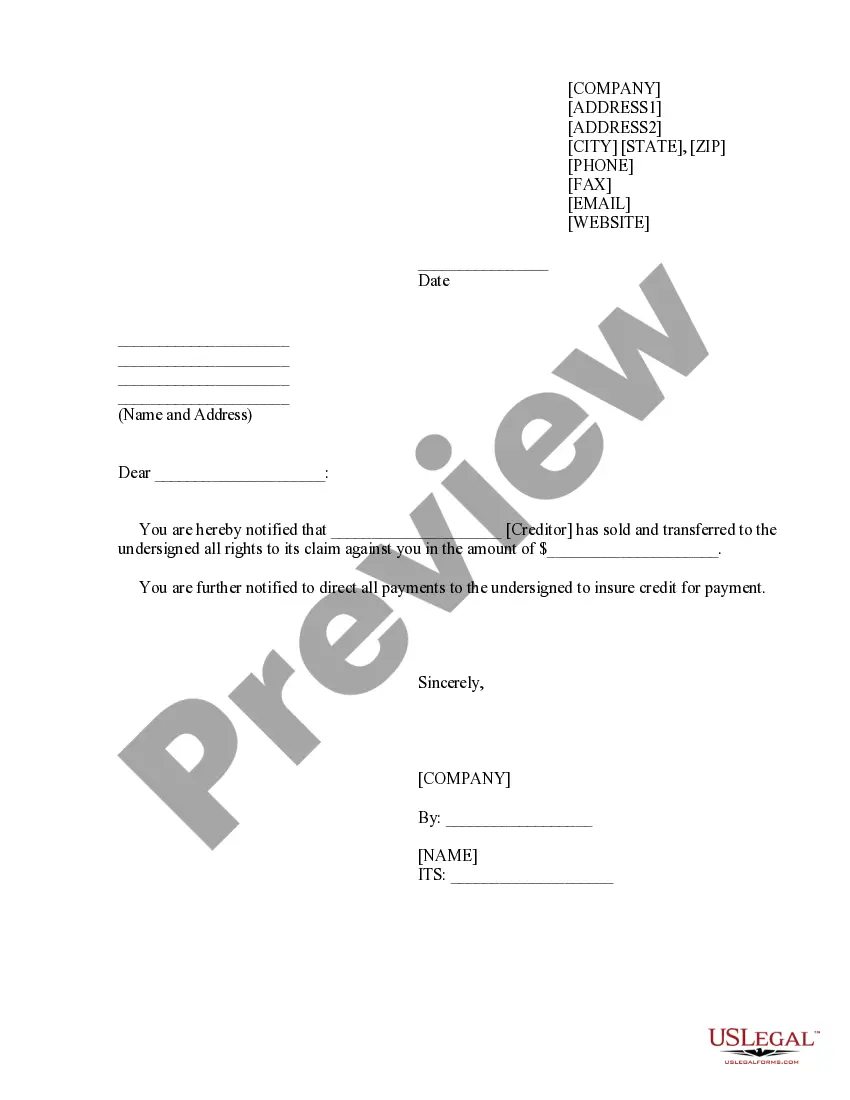
How to fill out Cuyahoga Ohio Qualifying Event Notice Information For Employer To Plan Administrator?
Preparing legal documentation can be difficult. Besides, if you decide to ask an attorney to draft a commercial contract, documents for ownership transfer, pre-marital agreement, divorce paperwork, or the Cuyahoga Qualifying Event Notice Information for Employer to Plan Administrator, it may cost you a fortune. So what is the best way to save time and money and create legitimate forms in total compliance with your state and local laws? US Legal Forms is a great solution, whether you're searching for templates for your personal or business needs.
US Legal Forms is largest online collection of state-specific legal documents, providing users with the up-to-date and professionally checked templates for any scenario accumulated all in one place. Consequently, if you need the latest version of the Cuyahoga Qualifying Event Notice Information for Employer to Plan Administrator, you can easily locate it on our platform. Obtaining the papers takes a minimum of time. Those who already have an account should check their subscription to be valid, log in, and pick the sample using the Download button. If you haven't subscribed yet, here's how you can get the Cuyahoga Qualifying Event Notice Information for Employer to Plan Administrator:
- Look through the page and verify there is a sample for your region.
- Check the form description and use the Preview option, if available, to ensure it's the sample you need.
- Don't worry if the form doesn't suit your requirements - search for the correct one in the header.
- Click Buy Now when you find the needed sample and pick the best suitable subscription.
- Log in or register for an account to purchase your subscription.
- Make a transaction with a credit card or via PayPal.
- Opt for the document format for your Cuyahoga Qualifying Event Notice Information for Employer to Plan Administrator and download it.
When done, you can print it out and complete it on paper or upload the template to an online editor for a faster and more practical fill-out. US Legal Forms enables you to use all the paperwork ever obtained many times - you can find your templates in the My Forms tab in your profile. Try it out now!