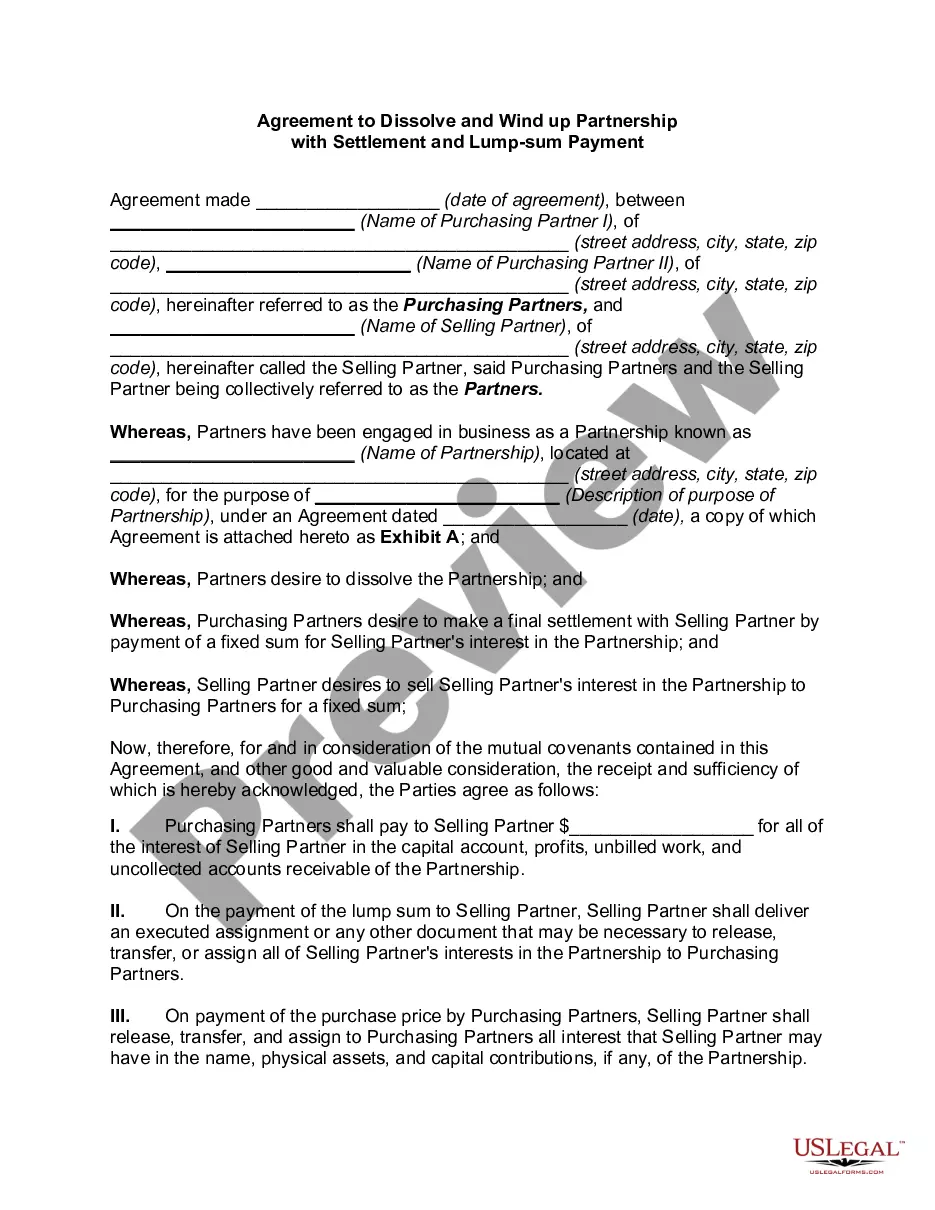
The parties may agree to a different performance. This is called an accord. When the accord is performed, this is called an accord and satisfaction. The original obligation is discharged. In order for there to be an accord and satisfaction, there must be a bona fide dispute; an agreement to settle the dispute; and the performance of the agreement. An example would be settlement of a lawsuit for breach of contract. The parties might settle for less than the amount called for under the contract.
Denied Claim Agreement For Primary Eob In Kings
Description
Form popularity
FAQ
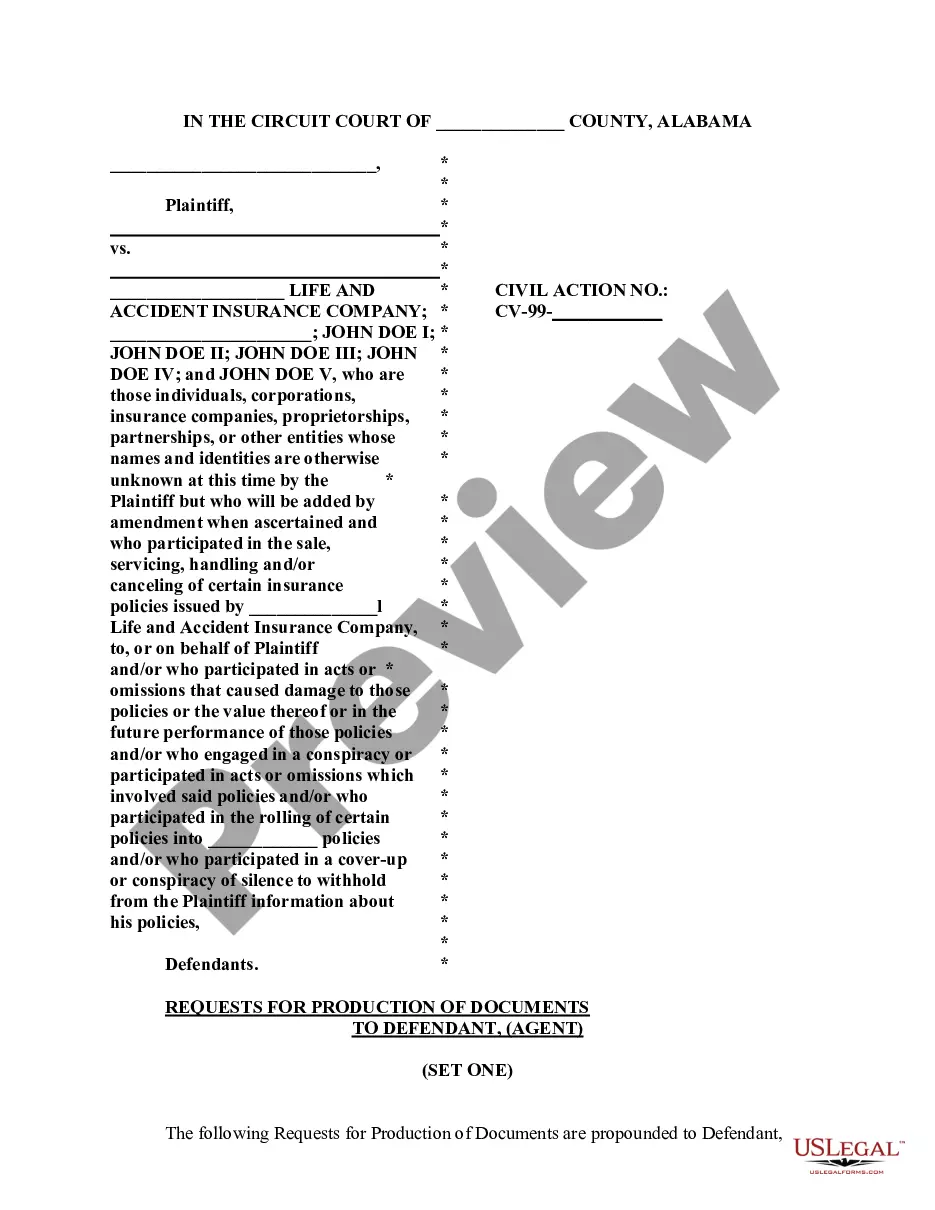
Some basic pointers for handling claims denials are outlined below. Carefully review all notifications regarding the claim. Be persistent. Don't delay. Get to know the appeals process. Maintain records on disputed claims. Remember that help is available.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
What to Do if Your Insurance Company Denies Your Claim in India? Correct the Data. Inform your insurer about reinitiating the claim. Proper Documentation. In case the reason why your claim was not accepted was a missing document, then make sure to provide that document this time. Prove that Hospitalization was Recommended.
A claim that is not submitted within 365 days of the date of service will not be considered for payment. If a client is not yet eligible for Medicaid, providers must submit the claim using either 999999999 or 000000000 as the recipient identification number.
You can start the appeal process by calling your insurance provider. Ask for more details about the denial and review your appeal options. Your insurance agent can walk you through the appeals process to help get you started.
The first step in resolving a denied insurance claim is to understand why it was denied. Carefully review the denial notice you received from the insurance company to determine the reason for the denial. This may include issues with the diagnosis, treatment plan, or documentation provided.
Remark code M129 indicates that there is an issue with the documentation related to an x-ray; specifically, it means that the indicator which confirms the availability of the x-ray for review is either missing, incomplete, or invalid. This needs to be addressed for the claim to be processed correctly.
CO 109 denial code indicates that the claim was rejected due to coordination of benefits (COB) issues. Coordination of benefits refers to situations where a patient is covered by multiple insurance policies, and the primary and secondary insurers have not coordinated their payment responsibilities appropriately.
CO 129 Payment denied – prior processing information incorrect. Void/replacement error. CO 135 No discharge date permitted for interim claims. CO 151 All dates of service on claim must be within same calendar month, except discharge date can be 1st day of following month.
Denial code 273 is when the healthcare provider exceeded the coverage or program guidelines, resulting in the claim being denied.