Alaska Acknowledgment of Receipt of COBRA Notice
Description
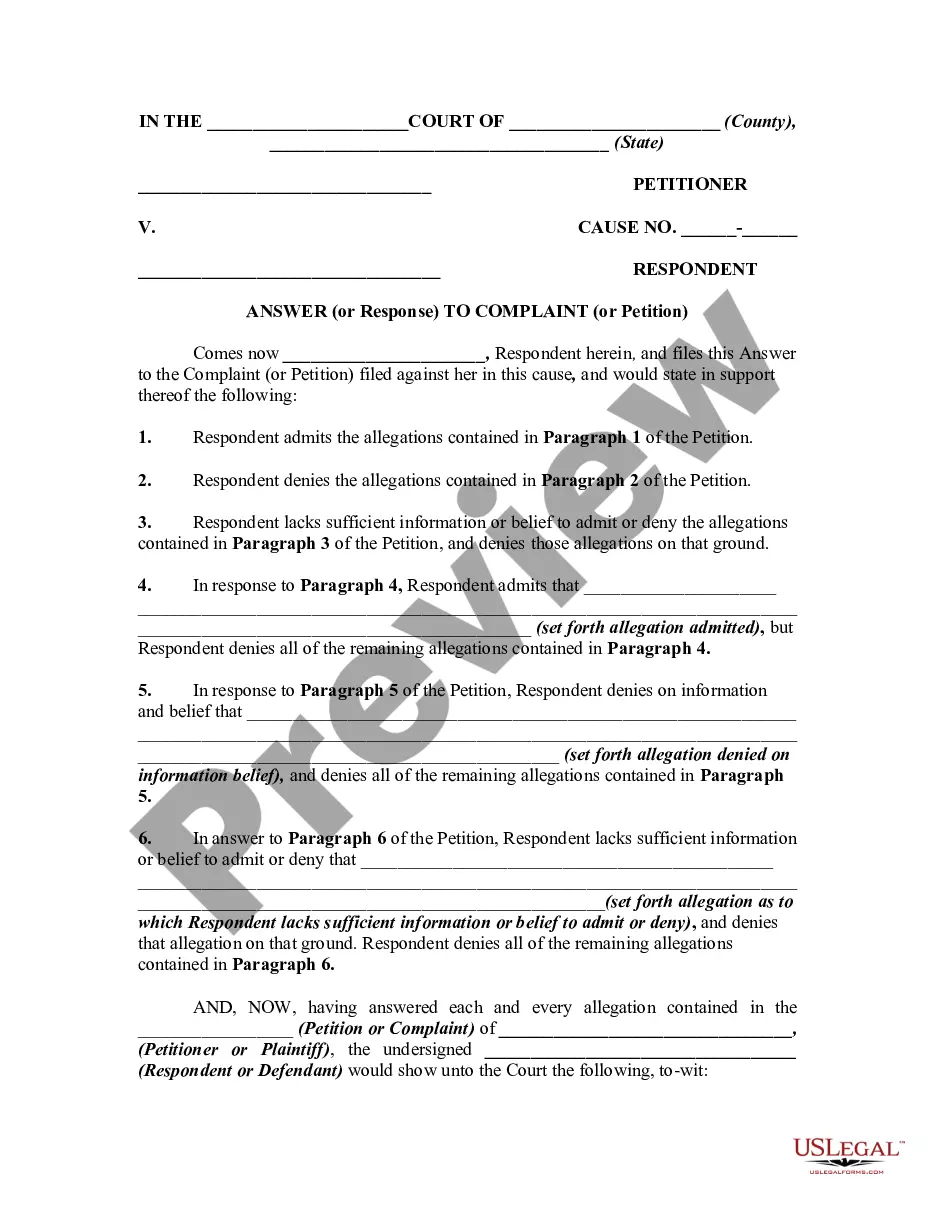
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
Finding the appropriate legal document format can be a challenge. Clearly, there are numerous templates accessible online, but how do you identify the legal template you require? Utilize the US Legal Forms website.
The platform provides a vast array of templates, such as the Alaska Acknowledgment of Receipt of COBRA Notice, which you can utilize for both business and personal purposes. Each of the documents is reviewed by experts and complies with federal and state regulations.
If you are already registered, Log In to your account and click the Acquire button to obtain the Alaska Acknowledgment of Receipt of COBRA Notice. Use your account to review the legal documents you have previously purchased. Navigate to the My documents section of your account and download another copy of the file you need.
Select the file format and download the legal document template to your device. Complete, modify, print, and sign the received Alaska Acknowledgment of Receipt of COBRA Notice. US Legal Forms is the largest collection of legal forms where you can find a variety of document templates. Use the service to obtain properly crafted documents that adhere to state guidelines.
- First, ensure you have selected the correct form for your area/county.
- You can review the form using the Review button and read the form details to confirm it is suitable for you.
- If the form does not satisfy your needs, utilize the Search field to locate the appropriate form.
- Once you are confident that the form is accurate, click on the Acquire now button to obtain the form.
- Choose the pricing plan you prefer and enter the necessary information.
- Create your profile and pay for the order using your PayPal account or credit card.