Alaska COBRA Notice Timing Delivery Chart
Description
How to fill out COBRA Notice Timing Delivery Chart?
If you need to comprehensive, download, or print valid document templates, utilize US Legal Forms, the largest compilation of legal forms available on the Internet.
Employ the site's simple and user-friendly search feature to locate the documents you seek.
A range of templates for commercial and personal use are organized by categories and states or keywords.
Step 3. If you are not satisfied with the form, use the Search field at the top of the page to find other versions in the legal form format.
Step 4. Once you have found the form you require, select the Purchase now button. Choose the pricing plan you prefer and input your information to sign up for an account.
- Access US Legal Forms to find the Alaska COBRA Notice Timing Delivery Chart with just a few clicks.
- If you are already a US Legal Forms customer, Log In to your account and then click the Download button to retrieve the Alaska COBRA Notice Timing Delivery Chart.
- You can also access forms you previously obtained in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Ensure you have selected the correct form for your specific city/state.
- Step 2. Use the Preview option to view the form’s details. Don’t forget to read the description.
Form popularity
FAQ
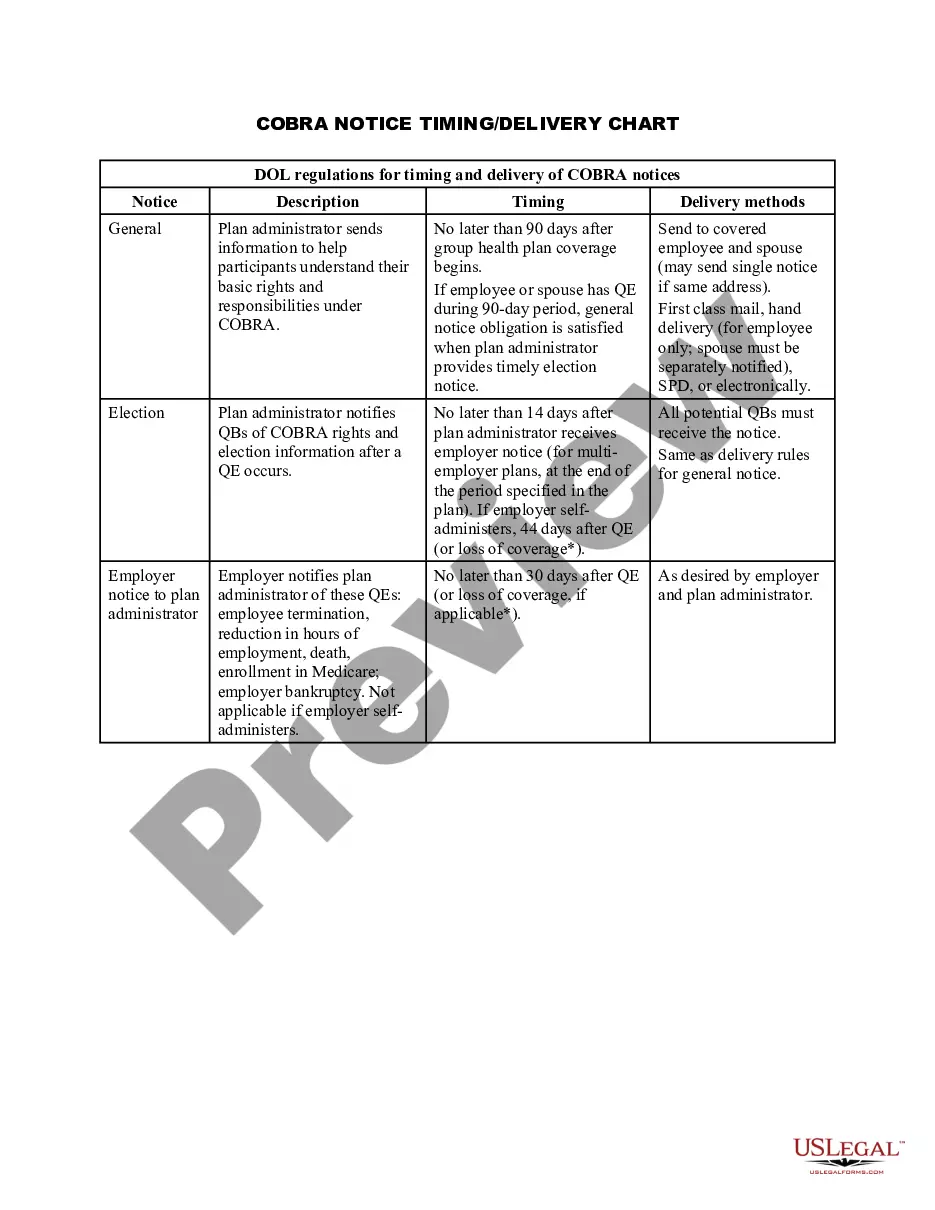
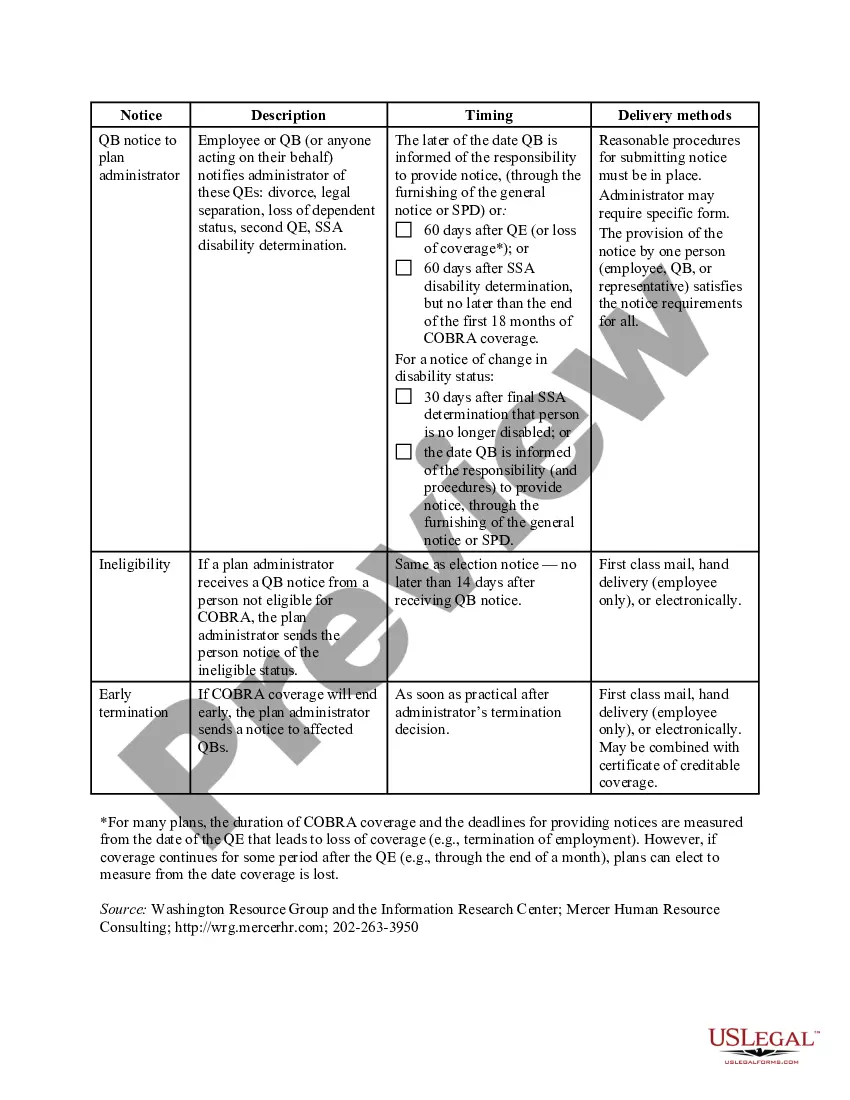
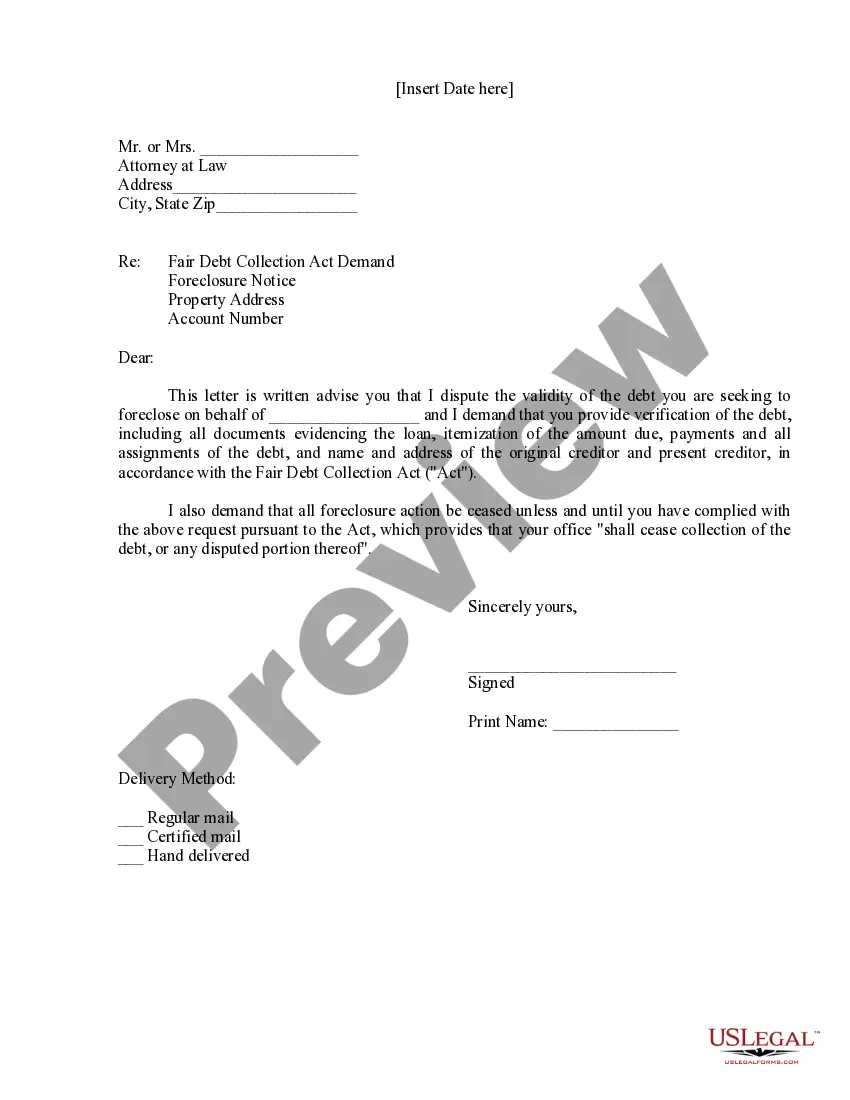
Legally, if your employer is subject to COBRA requirements, they must notify the organization's group health plan administrator within 30 days of your last day with your employer. At that point, the plan administrator then has 14 days to notify the former employee of their COBRA rights.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
COBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
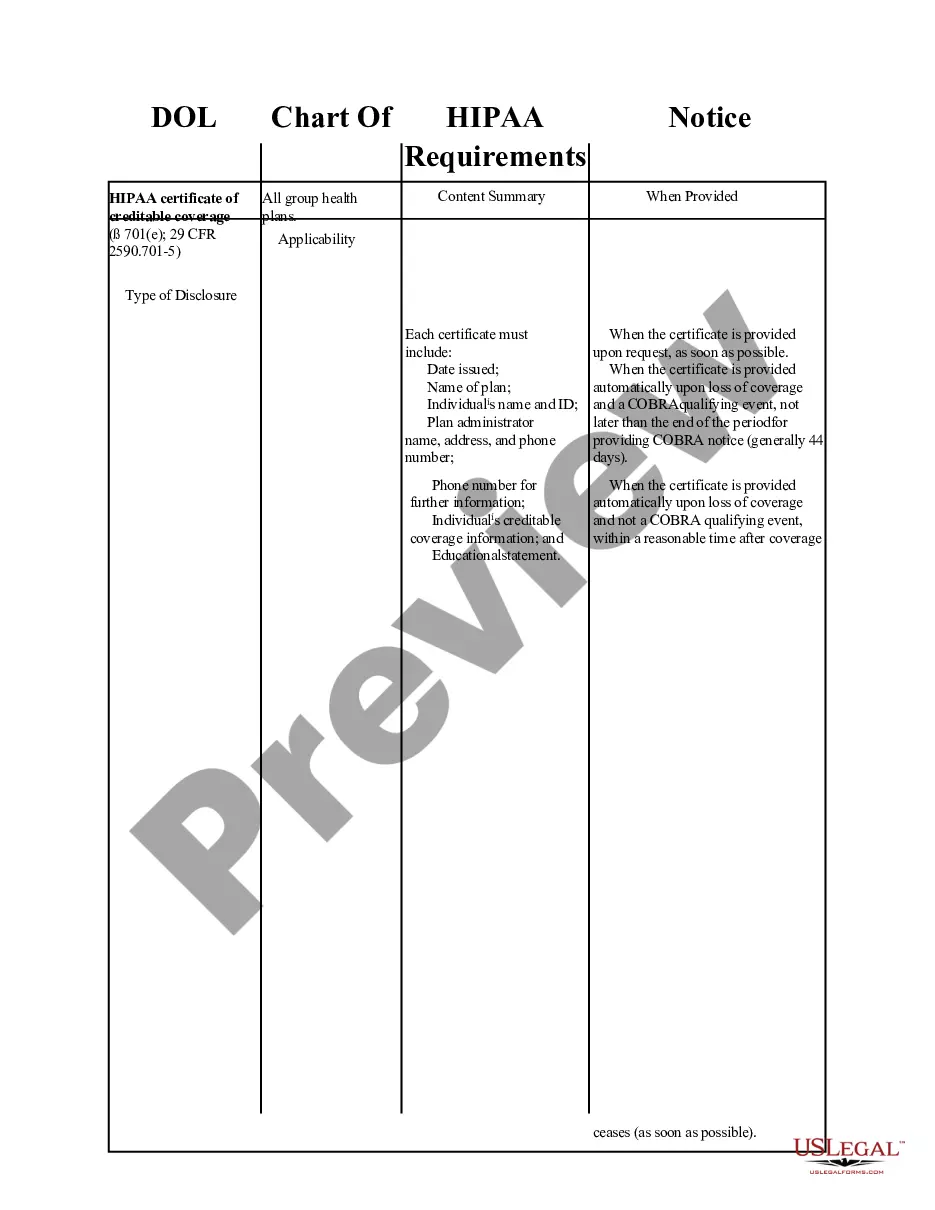
If you need further information about COBRA, ACA, HIPAA, or ERISA, visit the Employee Benefits Security Administration's (EBSA) Website at dol.gov/ebsa/complianceassistance.html. Or you may contact EBSA electronically at askebsa.dol.gov or call toll free 1-866-444-3272.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
COBRA is automatically available to you if you stop working at a qualified employer that provided group health insurance, but your participation in the program is not automatic. You must complete an enrollment form within the specified period of time and pay your first insurance premium.
Conclusion. Anyone eligible for COBRA insurance benefits has 2 months following the date of the end of their coverage, or the day they receive a COBRA notification, to enroll in a COBRA coverage plan.