Alaska General Notice of Preexisting Condition Exclusion is an important document that outlines the policyholder's rights and limitations regarding preexisting medical conditions under health insurance plans in the state of Alaska. This notice is typically presented to individuals who are applying for or enrolled in health insurance coverage and serves as a vital tool to educate them about the policy's provisions related to preexisting conditions. The notice emphasizes the need for individuals to be aware of how their preexisting conditions can affect their coverage and clarifies the various exclusions that may be imposed. This enables policyholders to make informed decisions regarding their health insurance options and be prepared for any potential limitations or restrictions on coverage related to their preexisting conditions. The Alaska General Notice of Preexisting Condition Exclusion helps individuals understand that insurance providers retain the right to exclude coverage for treatment related to preexisting conditions for a specific timeframe. This exclusion period often varies and depends on the specific insurance plan chosen. By disclosing this information in the notice, insurance companies aim to be transparent with individuals regarding how preexisting conditions may impact their coverage. Different types of Alaska General Notice of Preexisting Condition Exclusion may include: 1. Standard Preexisting Condition Exclusion: This exclusion specifies that any medical condition, illness, or injury that existed before the individual's health insurance coverage began will not be covered for a certain period. This exclusion period typically ranges from six months to one year, allowing insurance providers to limit coverage for related treatments during the initial phase of the policy. 2. Modified Preexisting Condition Exclusion: In some cases, insurance plans may modify the standard exclusion by reducing the waiting period or exempting certain preexisting conditions from the exclusion entirely. These modifications are intended to provide more comprehensive coverage for certain individuals or conditions, offering a more flexible approach to preexisting condition exclusions. 3. Group Insurance Exclusion: This type of exclusion is specific to group health insurance plans. The Alaska General Notice of Preexisting Condition Exclusion for group plans typically focuses on how preexisting conditions can impact coverage for new enrolled or employees joining the group plan. It outlines the waiting periods and restrictions that may apply to individuals who have preexisting conditions when joining the plan. Overall, the Alaska General Notice of Preexisting Condition Exclusion is an essential document that ensures transparency between insurance providers and policyholders regarding preexisting conditions and the limitations they may impose. By understanding the details outlined in this notice, individuals can make well-informed decisions when choosing health insurance coverage and be prepared for any limitations related to their preexisting conditions.
Alaska General Notice of Preexisting Condition Exclusion
Description
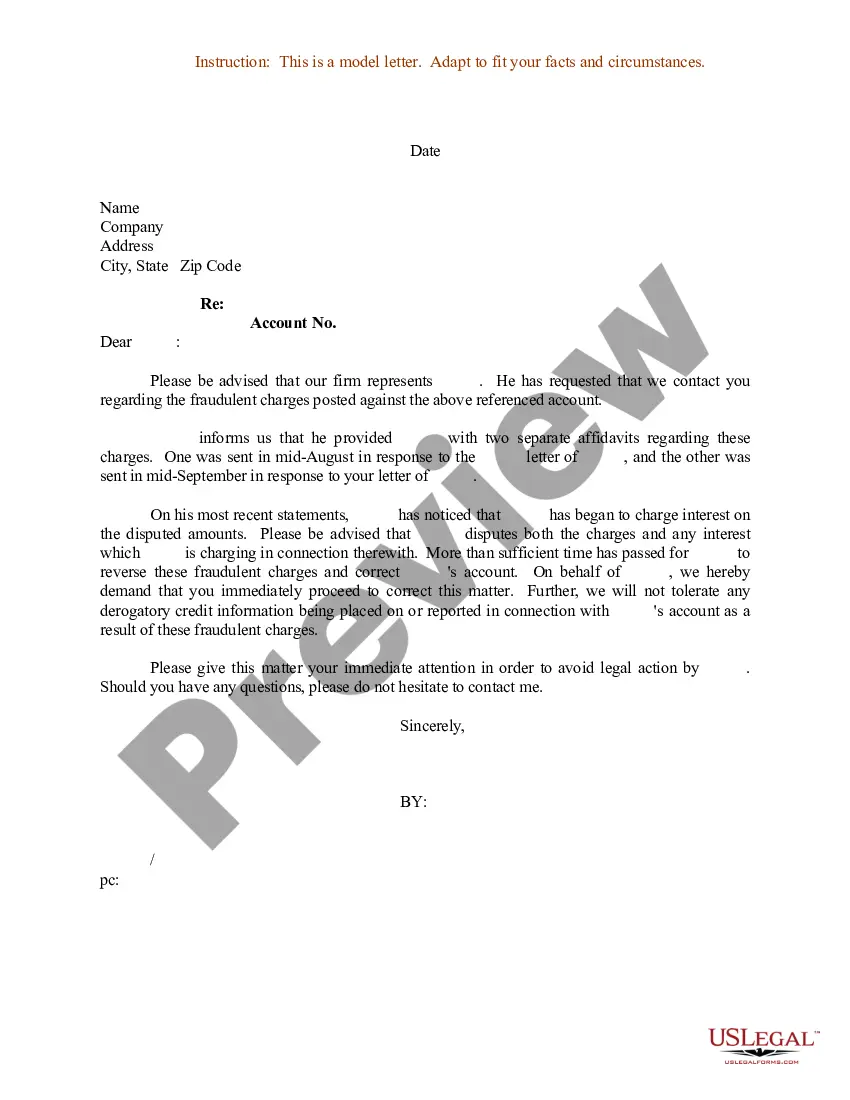
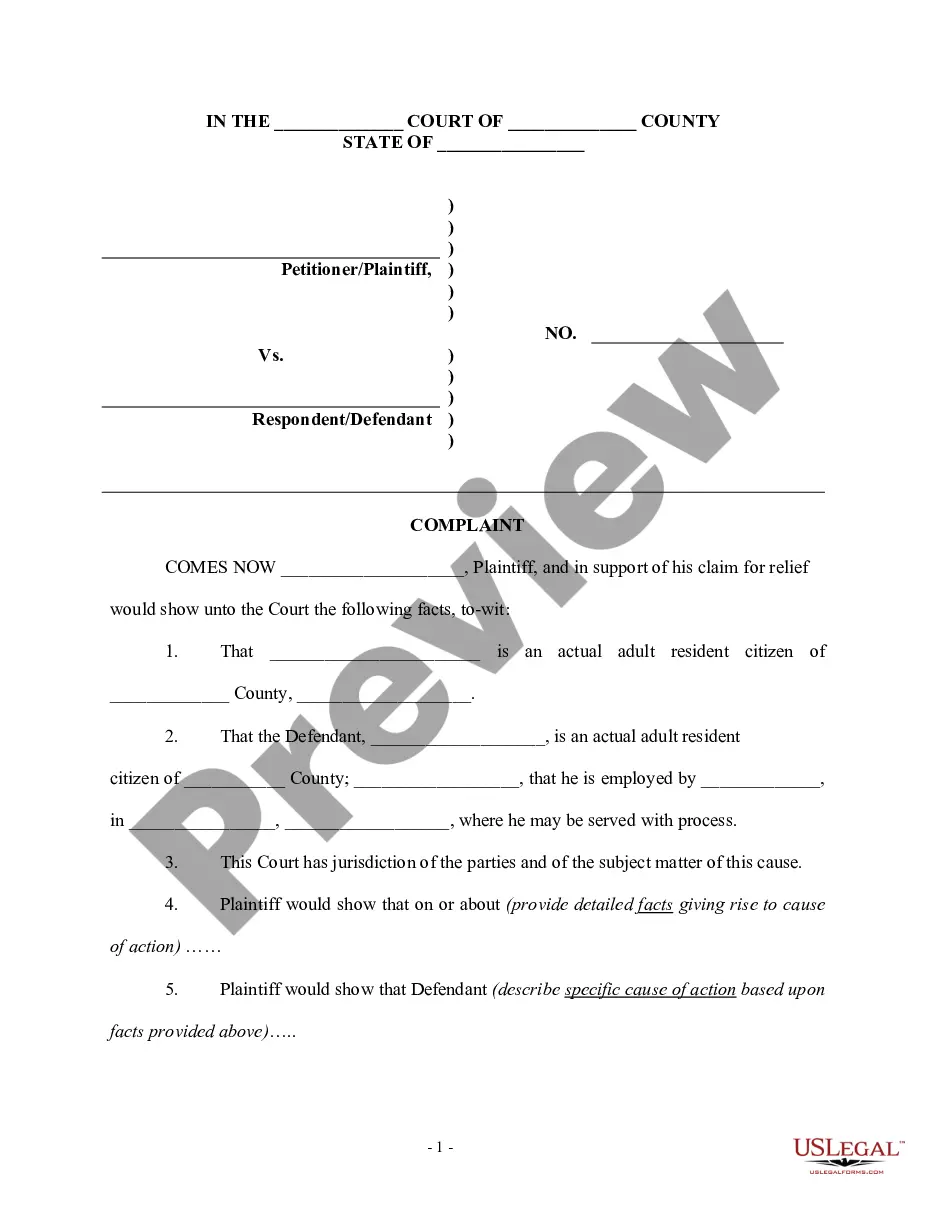
How to fill out Alaska General Notice Of Preexisting Condition Exclusion?
If you want to total, download, or print authorized record layouts, use US Legal Forms, the greatest assortment of authorized forms, which can be found on the web. Use the site`s simple and easy convenient lookup to find the papers you need. Different layouts for organization and person functions are sorted by classes and claims, or search phrases. Use US Legal Forms to find the Alaska General Notice of Preexisting Condition Exclusion within a few mouse clicks.
In case you are already a US Legal Forms customer, log in to your bank account and click on the Acquire key to find the Alaska General Notice of Preexisting Condition Exclusion. You may also accessibility forms you previously delivered electronically from the My Forms tab of your respective bank account.
Should you use US Legal Forms initially, refer to the instructions beneath:
- Step 1. Be sure you have chosen the shape to the proper city/country.
- Step 2. Utilize the Review choice to check out the form`s articles. Do not neglect to read through the explanation.
- Step 3. In case you are not satisfied with all the kind, utilize the Look for industry towards the top of the monitor to discover other versions in the authorized kind format.
- Step 4. Once you have found the shape you need, select the Purchase now key. Opt for the rates strategy you like and include your qualifications to sign up for an bank account.
- Step 5. Process the purchase. You can utilize your bank card or PayPal bank account to perform the purchase.
- Step 6. Choose the structure in the authorized kind and download it on your device.
- Step 7. Total, modify and print or signal the Alaska General Notice of Preexisting Condition Exclusion.
Each and every authorized record format you get is yours for a long time. You possess acces to each kind you delivered electronically inside your acccount. Select the My Forms area and select a kind to print or download once more.
Be competitive and download, and print the Alaska General Notice of Preexisting Condition Exclusion with US Legal Forms. There are many professional and status-particular forms you can use for your personal organization or person demands.