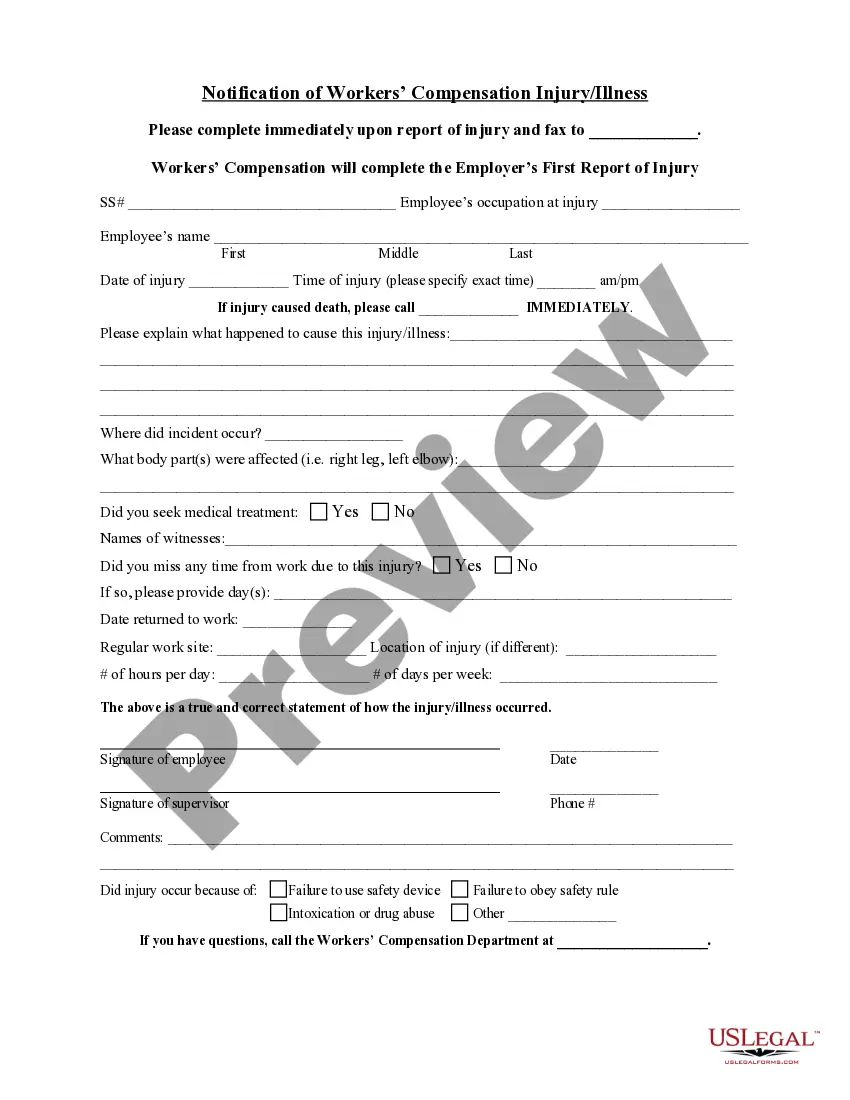
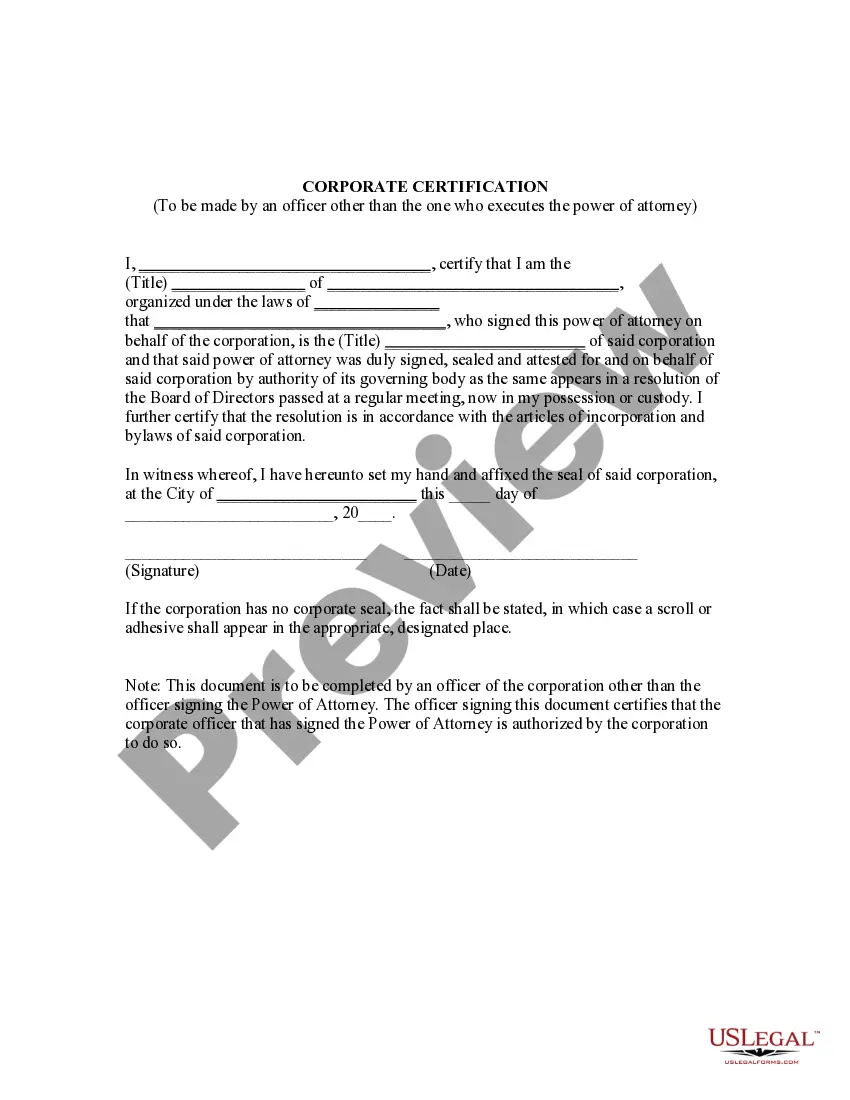
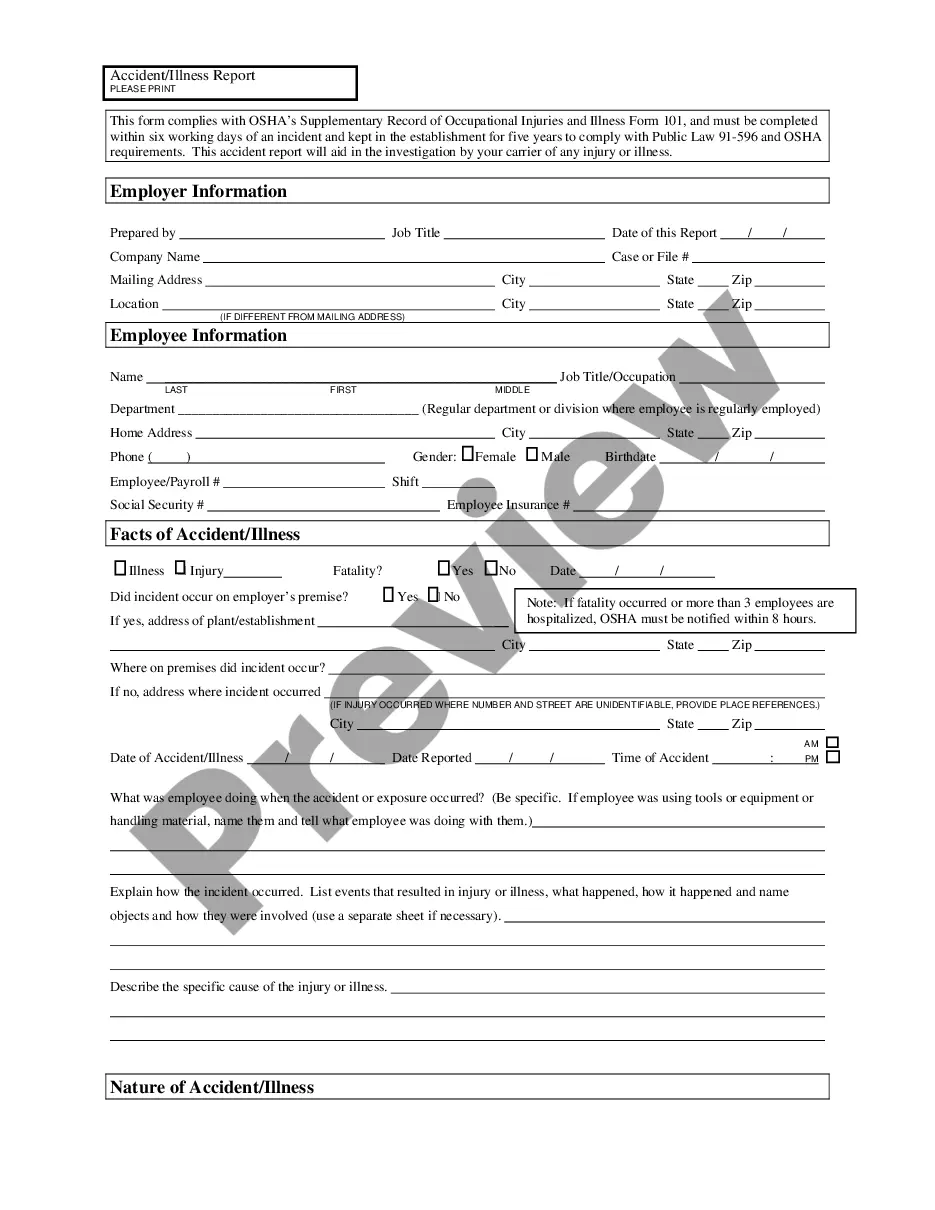
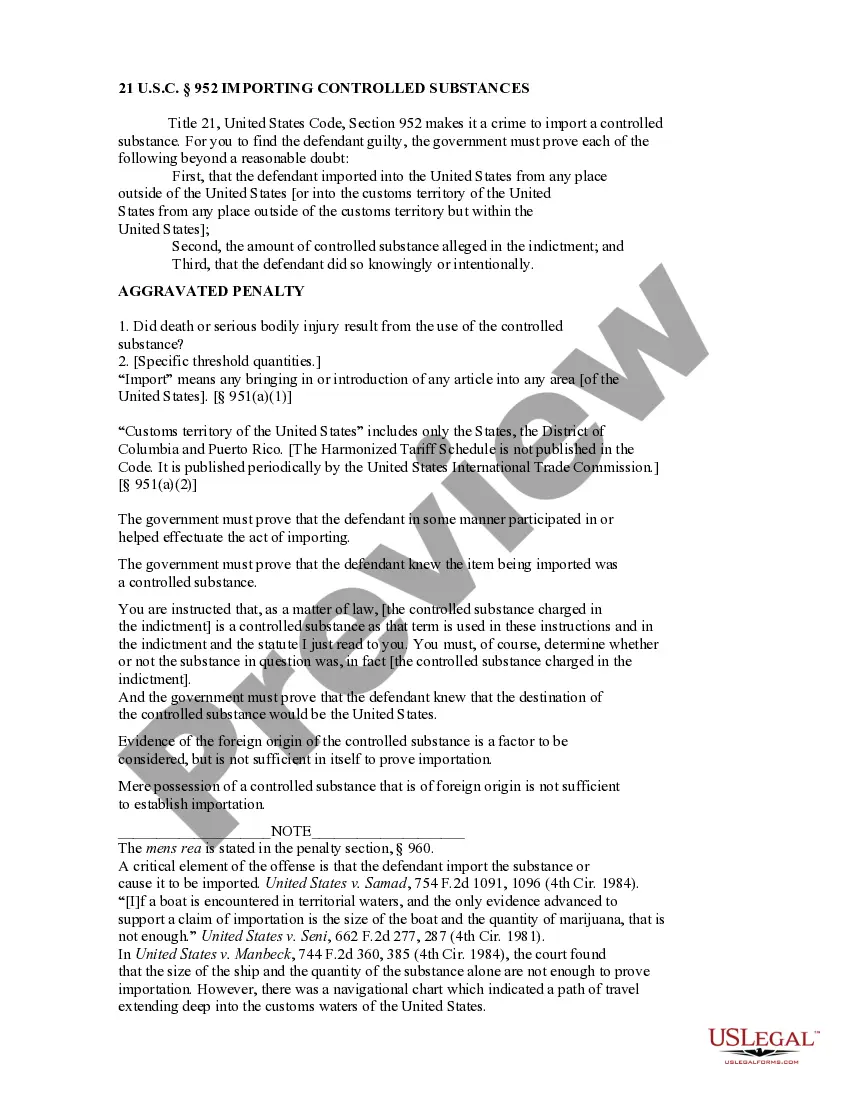
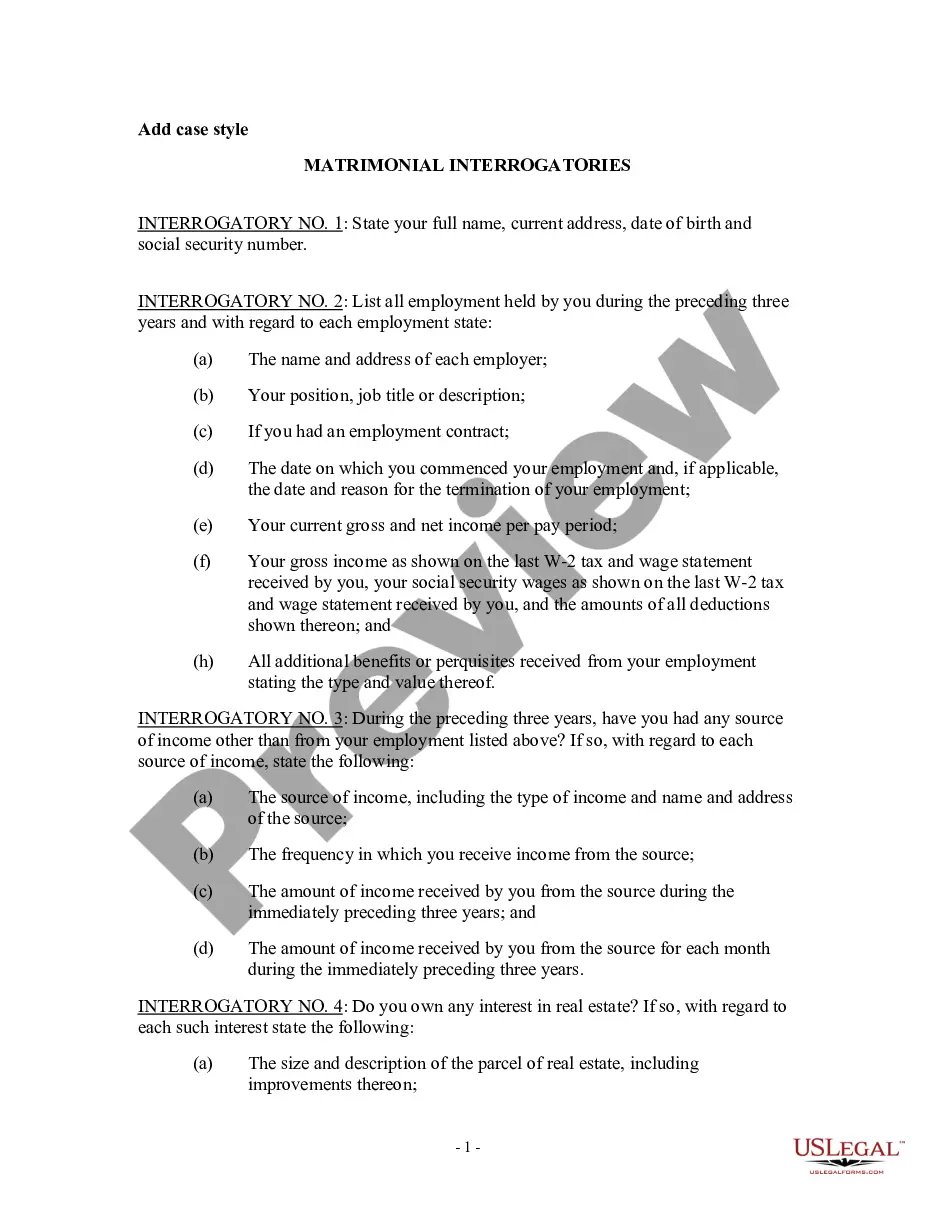
Alabama Recertification Required is a process by which medical providers in the state of Alabama must acquire certification from the Alabama Medicaid Agency in order to receive reimbursement for services provided to Medicaid recipients. Recertification is required for inpatient hospitalizations, outpatient hospitalizations, skilled nursing facility stays, and some high-cost medical procedures. There are three types of recertification required in Alabama: Prior Authorization, Concurrent Review, and Retrospective Review. Prior Authorization is a pre-certification process that requires medical providers to obtain approval from the Alabama Medicaid Agency before providing a service. Concurrent Review is a process where the Alabama Medicaid Agency reviews a service provided to a Medicaid recipient to determine if it was medically necessary and if it was billed correctly. Retrospective Review is a process where the Alabama Medicaid Agency reviews services provided to a Medicaid recipient after the service has been provided to ensure it was medically necessary and billed correctly.
Alabama Pre-Certification Required
Instant download
Public form
Description
Pre-Certification Required
How to fill out Alabama Pre-Certification Required?
How much time and resources do you frequently allocate to drafting formal documentation.
There’s a superior method to obtain such forms than employing legal experts or utilizing hours searching online for a suitable template.
An additional advantage of our library is that you can retrieve previously purchased documents that you securely store in your profile in the My documents tab.
Save time and energy preparing legal documents with US Legal Forms, one of the most reliable online services. Register with us today!
- Assess the form content to confirm it aligns with your state regulations. To achieve this, review the form description or utilize the Preview option.
- If your legal template falls short of your needs, find an alternative by using the search tab located at the top of the page.
- If you are already registered with us, Log In and retrieve the Alabama Pre-Certification Required. Otherwise, proceed to the subsequent steps.
- Click Buy now when you identify the appropriate blank. Choose the subscription plan that fits you best to access our library’s full capabilities.
- Create an account and pay for your subscription. Payment can be made using your credit card or via PayPal - our service is entirely trustworthy for that.
- Download your Alabama Pre-Certification Required onto your device and complete it on a printed hard copy or electronically.