The Alabama General Notice of Preexisting Condition Exclusion is a legal document that outlines the guidelines and regulations regarding the exclusion of preexisting health conditions from insurance coverage. This notice serves to inform individuals and explain the limitations and restrictions that may apply to their insurance policy based on their preexisting conditions. Preexisting conditions are defined as any health conditions or illnesses that an individual has prior to obtaining insurance coverage. These conditions can vary widely, ranging from chronic diseases like diabetes or heart conditions, to past injuries or surgeries. Insurance companies may exclude coverage for these conditions, meaning that any related medical expenses or treatments will not be covered under the policy. The Alabama General Notice of Preexisting Condition Exclusion provides essential information to policyholders, ensuring they understand the terms and conditions of their insurance policy. This notice must be provided by insurance providers to applicants during the enrollment process, or to policyholders upon request. The notice may differ based on the type of insurance plan or policy. For instance, employer-sponsored group health plans may have their own specific notice regarding preexisting condition exclusions. Similarly, individual health insurance plans or government-funded programs like Medicaid or Medicare may have separate notices outlining their preexisting condition exclusion policies. To comply with the law, the Alabama General Notice of Preexisting Condition Exclusion must contain relevant keywords and details such as "preexisting condition," "exclusion," "insurance coverage," "limitations," "restrictions," "chronic diseases," "health conditions," "medical expenses," "enrollment process," "employer-sponsored group health plans," "individual health insurance plans," "government-funded programs," and "Medicaid." In conclusion, the Alabama General Notice of Preexisting Condition Exclusion is a crucial document that informs policyholders about the preexisting condition exclusion policy of their insurance plan. Understanding this notice is essential for individuals to make informed decisions about their insurance coverage and to be aware of any limitations or restrictions that may apply to their preexisting conditions.
Alabama General Notice of Preexisting Condition Exclusion
Description
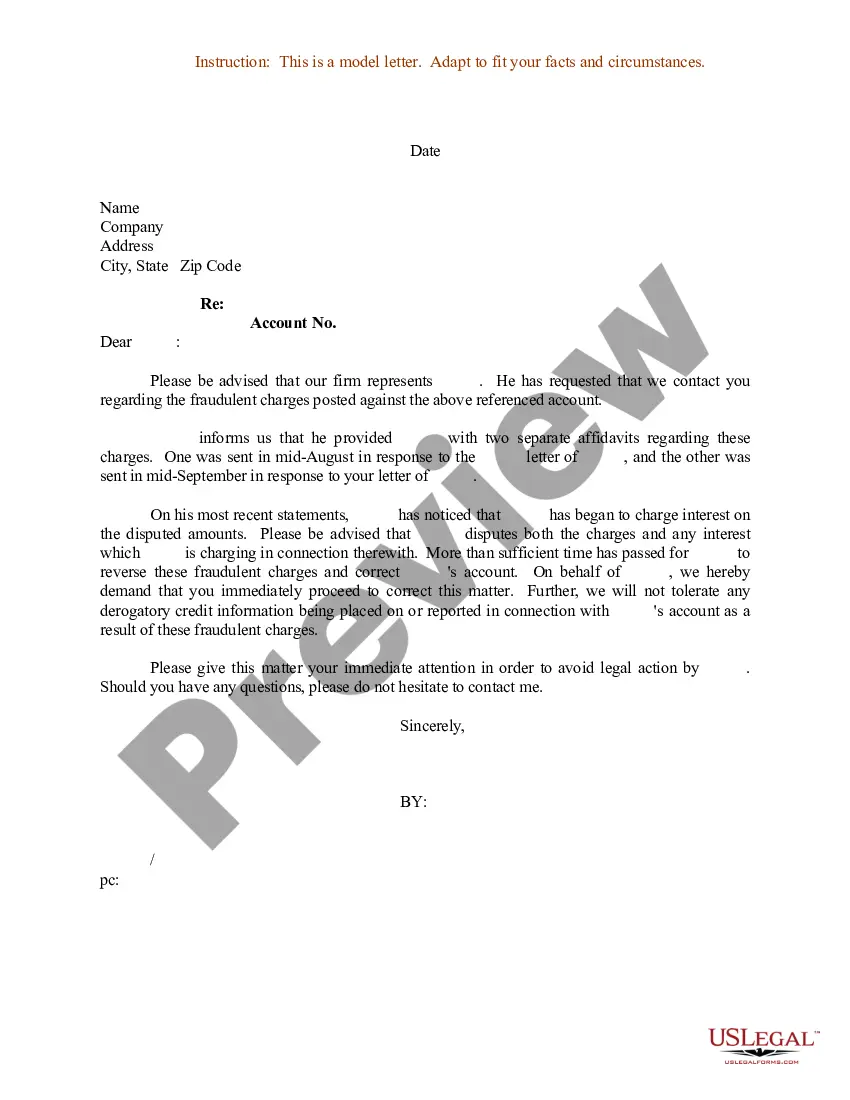
How to fill out Alabama General Notice Of Preexisting Condition Exclusion?
If you need to total, acquire, or print out legitimate papers web templates, use US Legal Forms, the biggest variety of legitimate types, which can be found on-line. Utilize the site`s simple and easy practical look for to find the documents you will need. Different web templates for company and specific uses are sorted by types and states, or search phrases. Use US Legal Forms to find the Alabama General Notice of Preexisting Condition Exclusion in just a number of mouse clicks.
When you are previously a US Legal Forms client, log in for your profile and then click the Obtain switch to find the Alabama General Notice of Preexisting Condition Exclusion. You can also accessibility types you in the past downloaded from the My Forms tab of your profile.
If you work with US Legal Forms for the first time, follow the instructions under:
- Step 1. Ensure you have chosen the form for your right metropolis/land.
- Step 2. Make use of the Review choice to examine the form`s content material. Don`t overlook to read through the outline.
- Step 3. When you are not satisfied with the type, utilize the Lookup area on top of the monitor to find other versions in the legitimate type web template.
- Step 4. After you have identified the form you will need, click on the Acquire now switch. Select the prices prepare you like and put your accreditations to sign up on an profile.
- Step 5. Procedure the transaction. You can use your bank card or PayPal profile to complete the transaction.
- Step 6. Find the structure in the legitimate type and acquire it in your gadget.
- Step 7. Total, edit and print out or indicator the Alabama General Notice of Preexisting Condition Exclusion.
Every single legitimate papers web template you purchase is your own eternally. You possess acces to each type you downloaded inside your acccount. Select the My Forms area and select a type to print out or acquire yet again.
Remain competitive and acquire, and print out the Alabama General Notice of Preexisting Condition Exclusion with US Legal Forms. There are millions of specialist and status-specific types you can use to your company or specific requires.