Arkansas Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
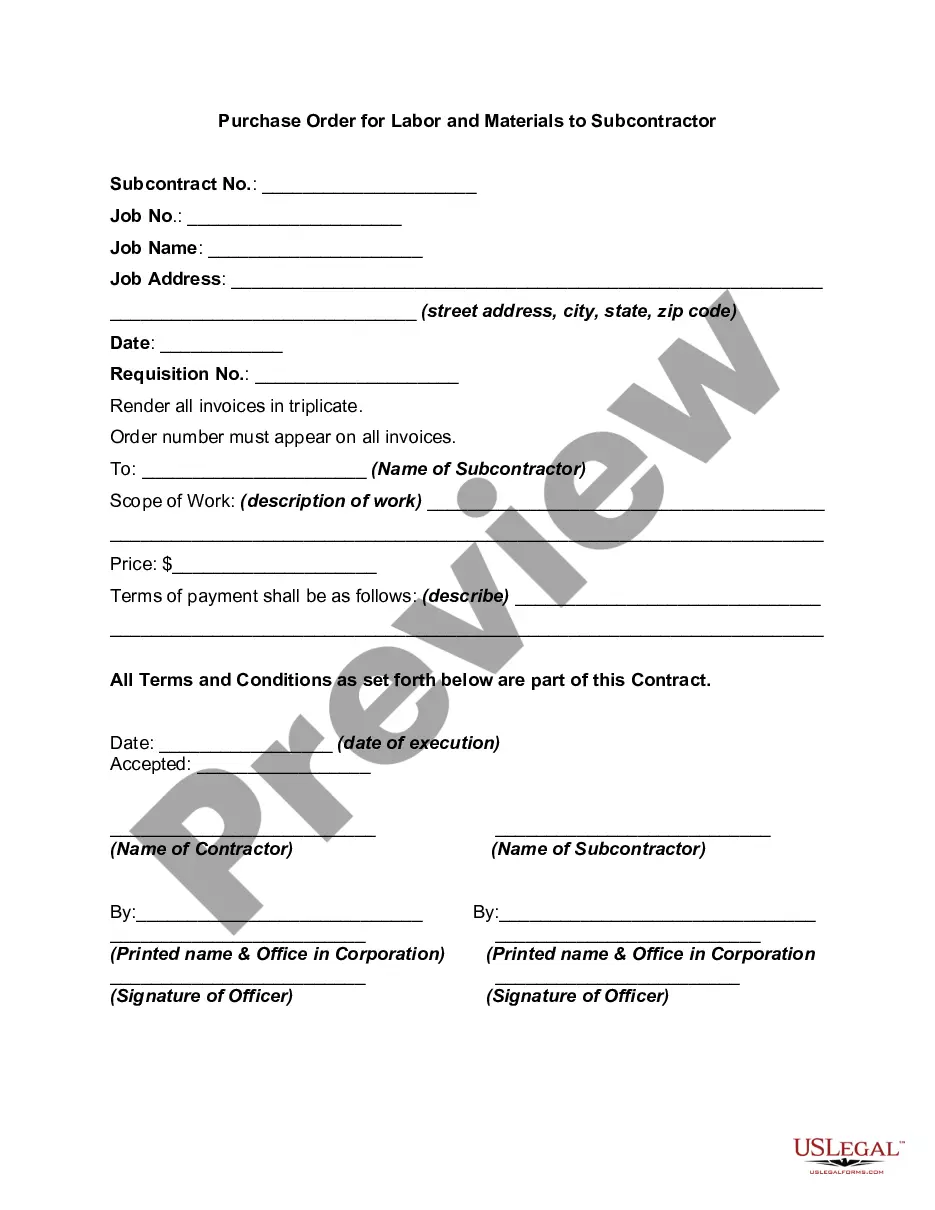
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
Choosing the right authorized record format could be a struggle. Obviously, there are a lot of web templates available on the net, but how can you discover the authorized form you want? Utilize the US Legal Forms site. The service delivers 1000s of web templates, such as the Arkansas Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, which can be used for enterprise and personal needs. Every one of the types are checked out by pros and meet up with state and federal needs.
When you are previously signed up, log in to the accounts and click on the Obtain option to obtain the Arkansas Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Make use of your accounts to check from the authorized types you have bought formerly. Check out the My Forms tab of your own accounts and obtain an additional duplicate of the record you want.
When you are a brand new customer of US Legal Forms, listed below are simple instructions that you should comply with:
- Initially, make sure you have selected the appropriate form to your city/county. You can examine the form making use of the Preview option and browse the form description to make certain it is the best for you.
- When the form is not going to meet up with your expectations, make use of the Seach field to get the appropriate form.
- Once you are certain the form would work, click on the Purchase now option to obtain the form.
- Opt for the pricing prepare you want and type in the needed details. Create your accounts and buy the transaction with your PayPal accounts or bank card.
- Select the submit format and obtain the authorized record format to the gadget.
- Full, revise and produce and indicator the obtained Arkansas Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
US Legal Forms may be the most significant library of authorized types that you can find different record web templates. Utilize the service to obtain expertly-made paperwork that comply with status needs.
Form popularity
FAQ
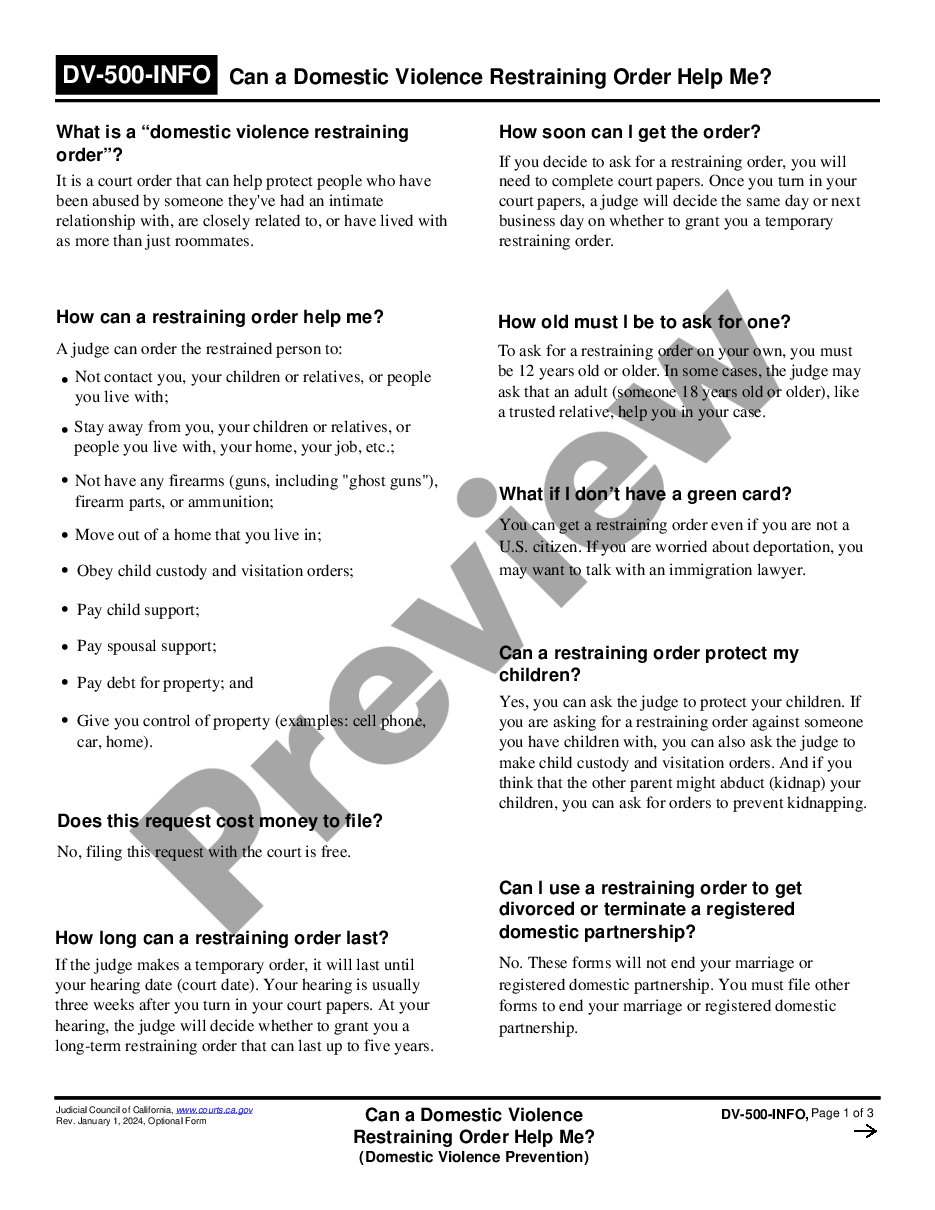
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
The Consolidated Omnibus Budget Reconciliation Act, known as COBRA, is a federal law that allows employees to continue their employer-provided health insurance after they are laid off or fired, or they otherwise become ineligible for benefits (for example, because they quit or their hours are reduced below the
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
Paying for COBRA coverage In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs. When an employee gets extended COBRA coverage due to disability, you can charge 150 percent of the premium for months 18 through 29.
A. Arkansas recognizes the doctrine of employment at will. This means that, as a general rule, either the employer or the employee may end the employment relationship at any time for any reason or for no reason at all.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
You typically have 31 days after termination of employment to apply for this coverage. Unlike the group term life insurance policy, premiums are fixed throughout the life of the policy. Premiums for the converted permanent life policy are higher than premiums for term insurance.