Arizona Medical Consent for Unconscious Patient
Description
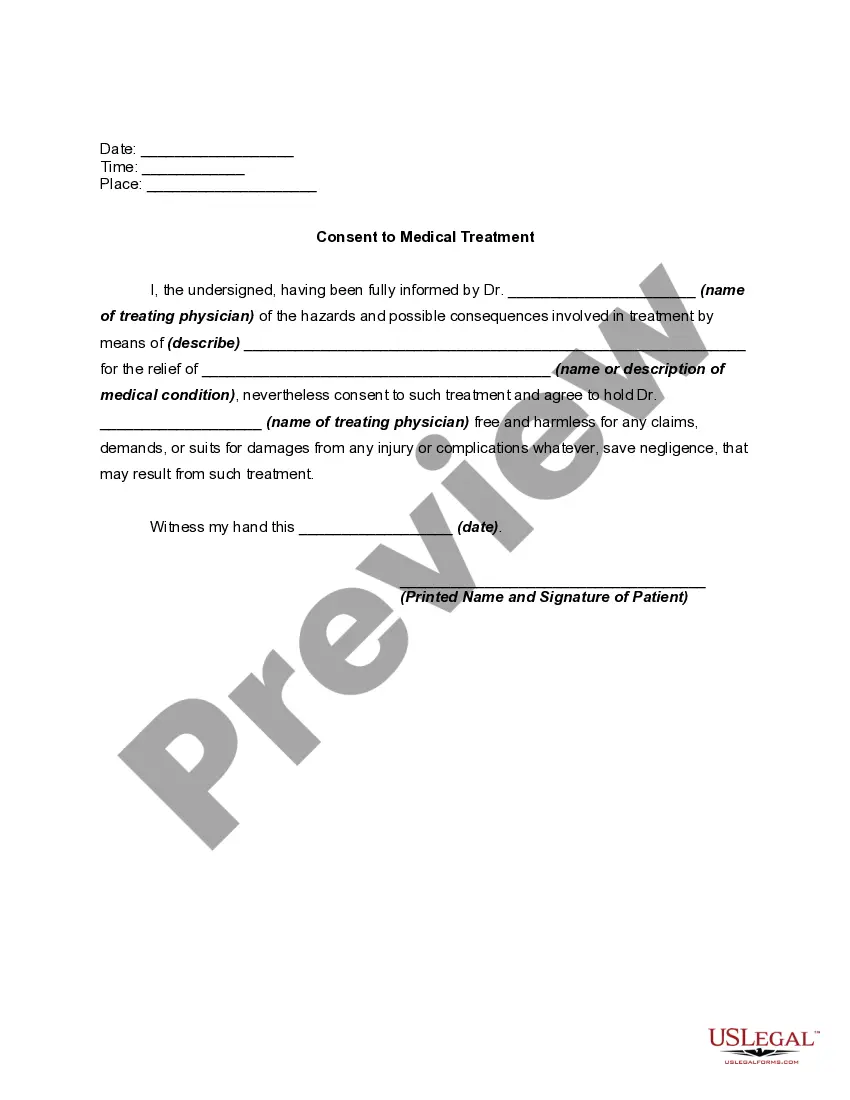
How to fill out Medical Consent For Unconscious Patient?
Selecting the appropriate legal document template can be challenging. There are countless templates available online, but how do you find the legal form you need? Visit the US Legal Forms website. The service offers numerous templates, including the Arizona Medical Consent for Unconscious Patient, suitable for both professional and personal use. All forms are reviewed by experts and comply with federal and state regulations.
If you are already registered, Log In to your account and click the Download button to access the Arizona Medical Consent for Unconscious Patient. Use your account to search through the legal documents you have previously purchased. Navigate to the My documents tab in your account to obtain another copy of the document you need.
If you are a new user of US Legal Forms, follow these simple instructions: First, ensure you have selected the correct form for your city/region. Use the Review button to browse the form and read the details to confirm it meets your needs. If the form does not suit your requirements, utilize the Search area to locate the correct document. Once you are confident that the form is suitable, click on the Get now button to acquire the form.
US Legal Forms is the largest repository of legal documents where you can find a wide range of document templates. Utilize the service to download professionally crafted paperwork that complies with state regulations.
- Choose the payment plan you prefer and provide the necessary information.
- Create your account and complete the transaction using your PayPal account or credit card.
- Select the file format and download the legal document template to your device.
- Complete, modify, print, and sign the received Arizona Medical Consent for Unconscious Patient.
Form popularity
FAQ
In the context of Arizona Medical Consent for Unconscious Patient, there are three main types of patient consent: informed consent, implied consent, and statutory consent. Informed consent requires a patient to fully understand the proposed treatment and its risks before agreeing to it. Implied consent occurs in emergency situations where a patient is unable to communicate but requires immediate medical attention. Statutory consent applies when legal frameworks allow for certain individuals to make medical decisions on behalf of unconscious patients, ensuring that care can proceed when the patient cannot voice their preferences.
Yes, treating a person who is unconscious and unable to consent is permitted under Arizona law. Medical professionals can provide necessary and life-saving treatments based on implied consent, ensuring the patient's wellbeing. Understanding the nuances of Arizona Medical Consent for Unconscious Patient helps clarify the duties of healthcare providers in such circumstances.
Indeed, an unconscious, confused, or seriously ill person cannot grant informed consent. In such cases, healthcare providers must turn to legal representatives or follow state laws governing medical decisions. Understanding the Arizona Medical Consent for Unconscious Patient is essential for healthcare providers to navigate these sensitive situations correctly.
An unconscious person typically gives implied consent for treatment in Arizona. This means that under the assumption that the patient would agree to medical help if they were able, healthcare providers can proceed with necessary interventions. In emergency situations, this legal framework is vital for ensuring prompt care.
Yes, you can treat an unconscious patient with first aid. In emergency scenarios, providing necessary first aid is crucial, particularly for life-threatening conditions. The Arizona Medical Consent for Unconscious Patient recognizes implied consent, allowing bystanders and medical professionals to act in the best interest of the patient when they cannot consent.
Obtaining informed consent for an unconscious patient involves following specific protocols. If the patient is incapacitated and cannot provide consent, healthcare providers may need to contact a family member or legal representative. In urgent situations, Arizona law allows for implied consent, assuming an unconscious patient would agree to necessary treatment to preserve their life.
Informed consent in Arizona requires that patients understand the nature of their treatment, the risks involved, and any potential benefits. Medical professionals must ensure that patients are competent to make decisions regarding their care. When dealing with an Arizona Medical Consent for Unconscious Patient, consent typically comes from a legal representative or through applicable laws regarding emergency situations.
If the victim is conscious, begin by explaining the medical situation and the necessary treatment in simple terms. Provide information about any risks and benefits associated with the treatment to help them understand their options. After ensuring they have all the information, seek their verbal consent. Adhering to Arizona Medical Consent for Unconscious Patient principles not only safeguards the patient but also reduces liability for medical professionals.
When a person is unconscious, the consent applied is typically referred to as implied consent. This legal framework allows medical personnel to provide necessary treatment without explicit authorization from the victim, as the law assumes that the patient would consent to care if able. Familiarity with Arizona Medical Consent for Unconscious Patient guidelines helps ensure that healthcare professionals act within the confines of the law.
To obtain consent from a conscious casualty, engage in a clear and calm discussion about their condition and the proposed treatment. Ensure they understand the benefits and risks involved, allowing them to make an informed decision. This approach not only respects the patient's autonomy but also aligns with Arizona Medical Consent for Unconscious Patient standards.