Subject: Arizona Sample Letter for Enclosure of Medical Reports — Comprehensive Template Included Dear [Recipient's Name], I am writing to provide you with the necessary medical reports and documentation pertaining to [patient's name]. These enclosed documents aim to provide a comprehensive overview of their medical history, diagnosis, treatment plan, and other pertinent information required for further assessment or record-keeping purposes. Please find the following enclosed items: 1. Medical History Report: This report contains a detailed summary of the patient's medical background, including prior illnesses, surgeries, allergies, and family medical history. It provides essential context for thoroughly understanding the patient's overall health. 2. Consultation Notes: These notes outline the discussions, observations, and findings from the latest consultations with the primary care physician, specialist, or any other relevant medical professionals. They will help to provide further insights into the patient's specific condition, diagnosis, treatment options, and prescribed medications. 3. Laboratory Test Results: Included are copies of any laboratory test reports conducted, such as blood tests, imaging scans, biopsies, or pathology test results. These reports offer objective data reflecting the patient's physiological or pathological conditions, thus supporting the diagnosis and treatment plans. 4. Surgical Reports (if applicable): When appropriate, copies of surgical reports from any previous procedures performed on the patient will be enclosed. These reports provide critical information concerning the surgical methodology used, anesthetic considerations, the surgeon's notes, and post-operative care instructions. 5. Medication Records: This section encompasses details of current and past medications prescribed to the patient. It includes the dosage, frequency, duration, and purpose of each medication, empowering you to make informed decisions and ensure medical compatibility. 6. Radiology Reports: Any radiology reports, such as X-rays, MRI scans, CT scans, or ultrasound imaging results, will be enclosed. These reports offer valuable insights into the patient's anatomical structures, highlighting abnormalities, injuries, or diseases that may require further attention. 7. Progress Notes: In order to provide an ongoing overview of the patient's treatment and progress, we have included relevant progress notes recorded during follow-up visits with the physician or specialist. These notes document changes in symptoms, treatment adjustments, and the effectiveness of prescribed interventions. 8. Referral Letters (if applicable): If the patient has been referred to you by another healthcare professional, we have included copies of the referral letters. These letters typically offer additional contextual information and reasons for seeking specialized care. By providing these comprehensive medical reports, our intention is to aid you in making well-informed decisions about the patient's healthcare needs. Should you require any further clarification or additional information, please do not hesitate to contact our office. Thank you for your attention to this matter. We look forward to collaborating with you in the best interest of our patient, ensuring they receive the highest quality care possible. Sincerely, [Your Name] [Your Title/Position] [Your Contact Information]
Arizona Sample Letter for Enclosure of Medical Reports
Description
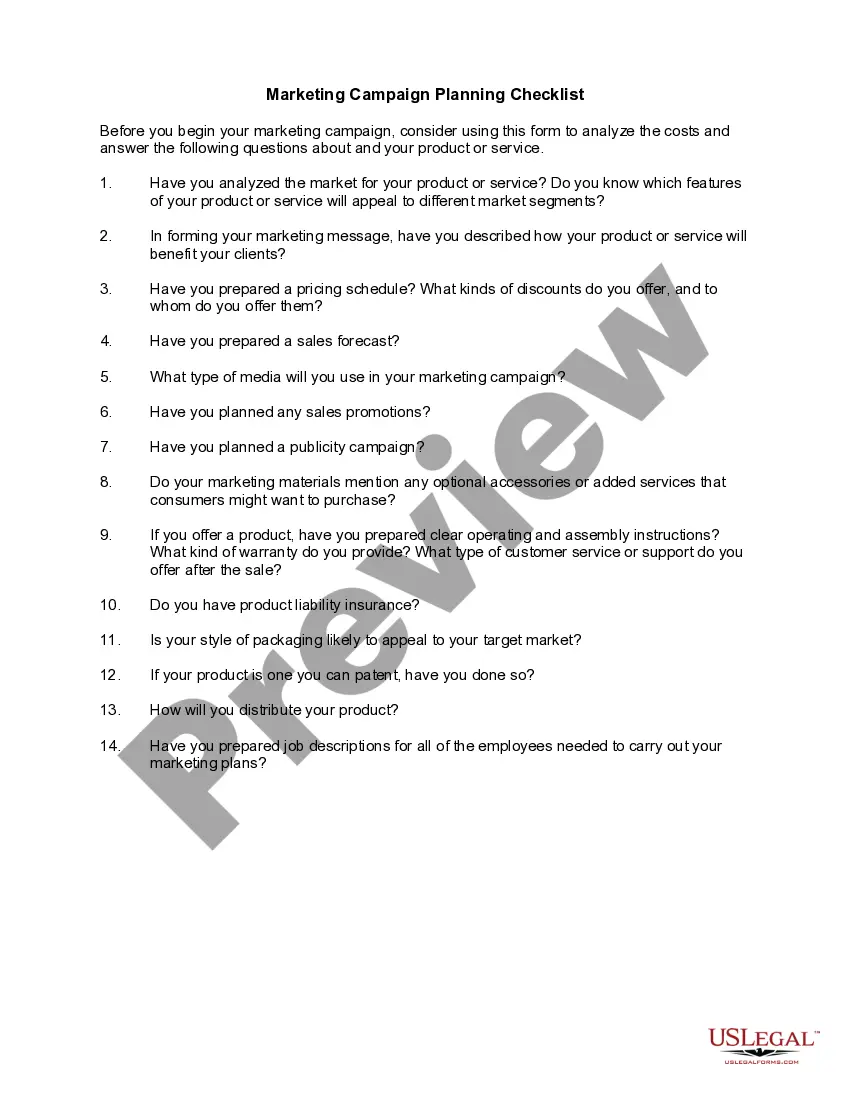
How to fill out Sample Letter For Enclosure Of Medical Reports?
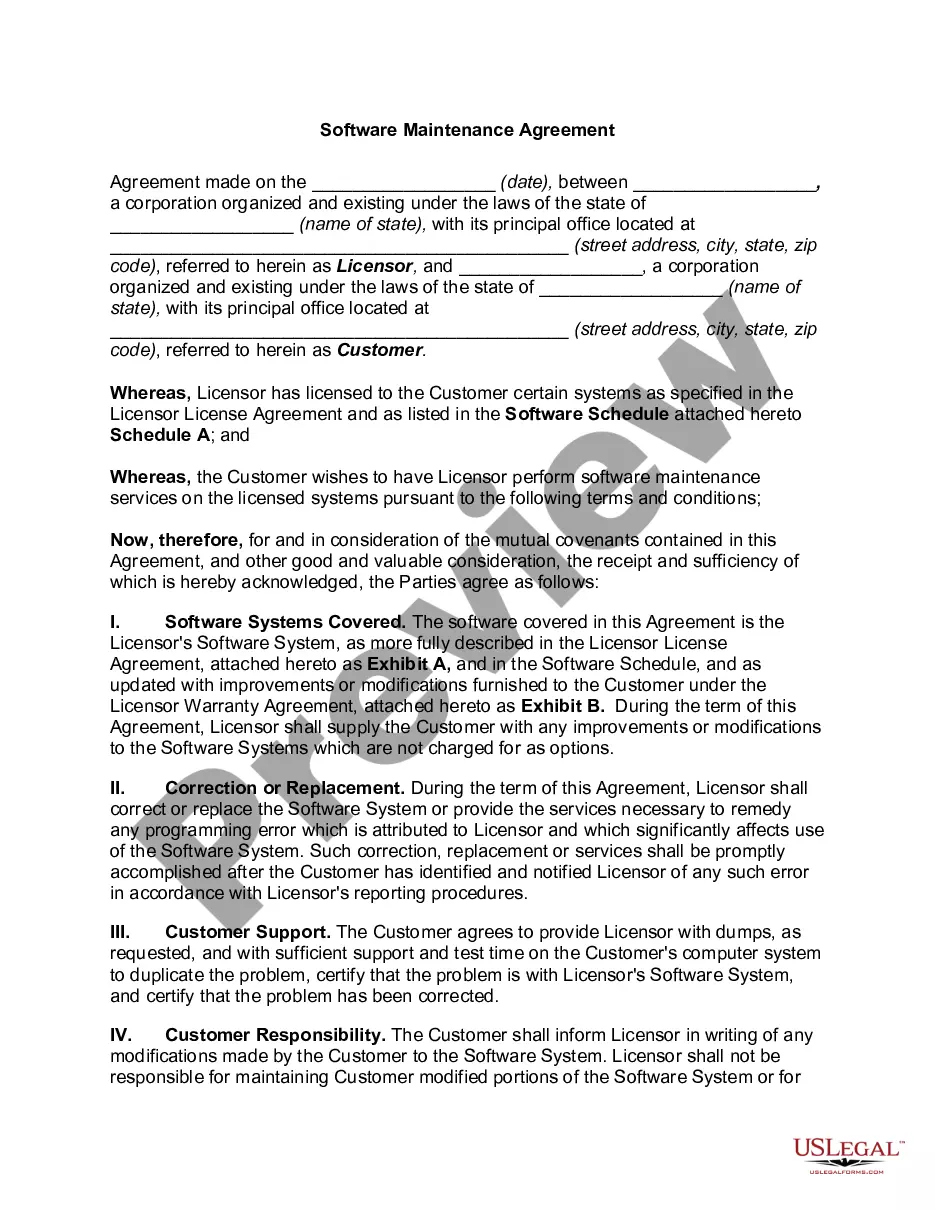
Are you inside a place where you need papers for sometimes organization or specific uses virtually every time? There are a lot of authorized document layouts available on the net, but locating ones you can depend on is not effortless. US Legal Forms offers a huge number of type layouts, much like the Arizona Sample Letter for Enclosure of Medical Reports, that happen to be written to meet federal and state demands.
When you are currently acquainted with US Legal Forms site and get a free account, simply log in. Afterward, you may download the Arizona Sample Letter for Enclosure of Medical Reports format.
Should you not provide an accounts and want to start using US Legal Forms, adopt these measures:
- Find the type you want and make sure it is for your right town/region.
- Take advantage of the Review key to review the shape.
- Look at the description to actually have chosen the proper type.
- In case the type is not what you are trying to find, utilize the Search industry to find the type that meets your needs and demands.
- Once you obtain the right type, just click Buy now.
- Opt for the rates program you need, fill out the required information and facts to generate your account, and pay for the order utilizing your PayPal or bank card.
- Pick a handy document structure and download your backup.
Find every one of the document layouts you have purchased in the My Forms menus. You can aquire a further backup of Arizona Sample Letter for Enclosure of Medical Reports anytime, if necessary. Just go through the necessary type to download or print the document format.
Use US Legal Forms, one of the most considerable variety of authorized kinds, to save some time and prevent mistakes. The support offers expertly created authorized document layouts that can be used for a selection of uses. Make a free account on US Legal Forms and start generating your way of life a little easier.
Form popularity
FAQ
Sample Format Letter of Medical Necessity Dear [Insert Contact Name]: [Insert Patient Name] has been under my care for [Insert Diagnosis] [Insert ICD-10-CM Code] since [Insert Date]. Treatment of [Insert Patient Name] with [medication] is medically appropriate and necessary and should be covered and reimbursed.
Sample Format Letter of Medical Necessity Dear [Insert Contact Name]: [Insert Patient Name] has been under my care for [Insert Diagnosis] [Insert ICD-10-CM Code] since [Insert Date]. Treatment of [Insert Patient Name] with [medication] is medically appropriate and necessary and should be covered and reimbursed.
I am writing on behalf of my patient, [Patient Name], to document the medical necessity to treat their [Diagnosis] with [Product Name]. This letter serves to document my patient's medical history and diagnosis and to summarize my treatment rationale. Please refer to the [List any Enclosures] enclosed with this letter.
I am writing on behalf of my patient, (patient name) to document the medical necessity of (treatment/medication/equipment ? item in question) for the treatment of (specific diagnosis). This letter provides information about the patients medical history and diagnosis and a statement summarizing my treatment rationale.
Guidelines for Writing Diagnostic Reports Appearance of the diagnostic report. ... Recency of the disability documentation and documentation updates. ... Reason for referral and history of the problem. ... Evaluation measures used in the report. ... Relevant developmental, educational and medical histories.
Explain the specific medical problem or functional limitation that results from the patient's diagnosis. You should give specifics about how the service requested will address the functional limitation. If applicable, include a paragraph about the availability of parents to provide the service requested.
I was treated in your office [at your facility] between [fill in dates]. I request copies of the following [or all] health records related to my treatment. [Identify records requested (e.g., medical-history form you filled out; physician and nurses' notes; test results; consultations with specialists; referrals).]
This includes a brief description of the patient's diagnosis, the severity of the patient's condition, prior treatments, the duration of each, responses to those treatments, the rationale for discontinuation, as well as other factors (eg underlying health issues, age) that have affected your treatment selection].