Title: Arizona Sample COBRA Enrollment and/or Waiver Letter: A Comprehensive Guide Introduction: This comprehensive guide aims to provide you with a detailed description of Arizona's COBRA (Consolidated Omnibus Budget Reconciliation Act) enrollment and/or waiver letter, including the various types available. COBRA allows eligible employees and their beneficiaries to maintain their group health coverage for a specified duration after a qualifying event, such as job loss or reduction in work hours. Learn more about these letters, their purpose, and how they can benefit individuals seeking continued health insurance coverage in Arizona. 1. Arizona Sample COBRA Enrollment Letter: The Arizona Sample COBRA Enrollment Letter is a crucial document designed to inform eligible employees about their right to continue their health insurance coverage under COBRA. This letter clearly outlines the employee's coverage options, including the costs associated with continuing the group health plan. It provides detailed guidance on how to enroll within the stipulated timeframe, usually 60 days from the date of the qualifying event. The purpose of this letter is to ensure individuals understand their COBRA rights and can make an informed decision regarding their health insurance coverage. 2. Arizona Sample COBRA Waiver Letter: On the other hand, the Arizona Sample COBRA Waiver Letter is intended for individuals who have been offered COBRA coverage but wish to decline or waive the opportunity to enroll. This letter acknowledges that the employee has been provided the necessary information and explanation of their COBRA rights but chooses not to proceed with continuing their health insurance coverage. It is essential for employers to obtain this waiver letter to ensure compliance with COBRA regulations and to document the employee's decision accurately. 3. Key Components of the Arizona Sample COBRA Letters: — Employee and employer information: The letters include details such as employee name, address, contact information, and employer identification. — Qualifying event information: Both letters state the reason for qualifying under COBRA, whether it be job termination, reduction in work hours, or certain life events. — Coverage details: The letters provide essential information about the specific healthcare plan, coverage duration, and costs associated with continuing the coverage. — Instructions and deadlines: Individuals receive clear instructions regarding the enrollment process, payment methods, and applicable deadlines for submitting the necessary paperwork, such as enrollment forms or waiver letters. — Assistance and contact information: The letters offer support by providing contact details for designated personnel who can address any inquiries or concerns regarding COBRA coverage options. Conclusion: Understanding the Arizona Sample COBRA Enrollment and/or Waiver Letter is vital for both employees and employers as it enables individuals to make informed decisions about their healthcare coverage following a qualifying event. These letters serve as official documentation, informing individuals about their rights and obligations under COBRA. By utilizing these sample letters and carefully following the instructions outlined, individuals can navigate the COBRA enrollment process successfully, ensuring they maintain essential health insurance coverage during challenging times.
Arizona Sample COBRA Enrollment and / or Waiver Letter
Description
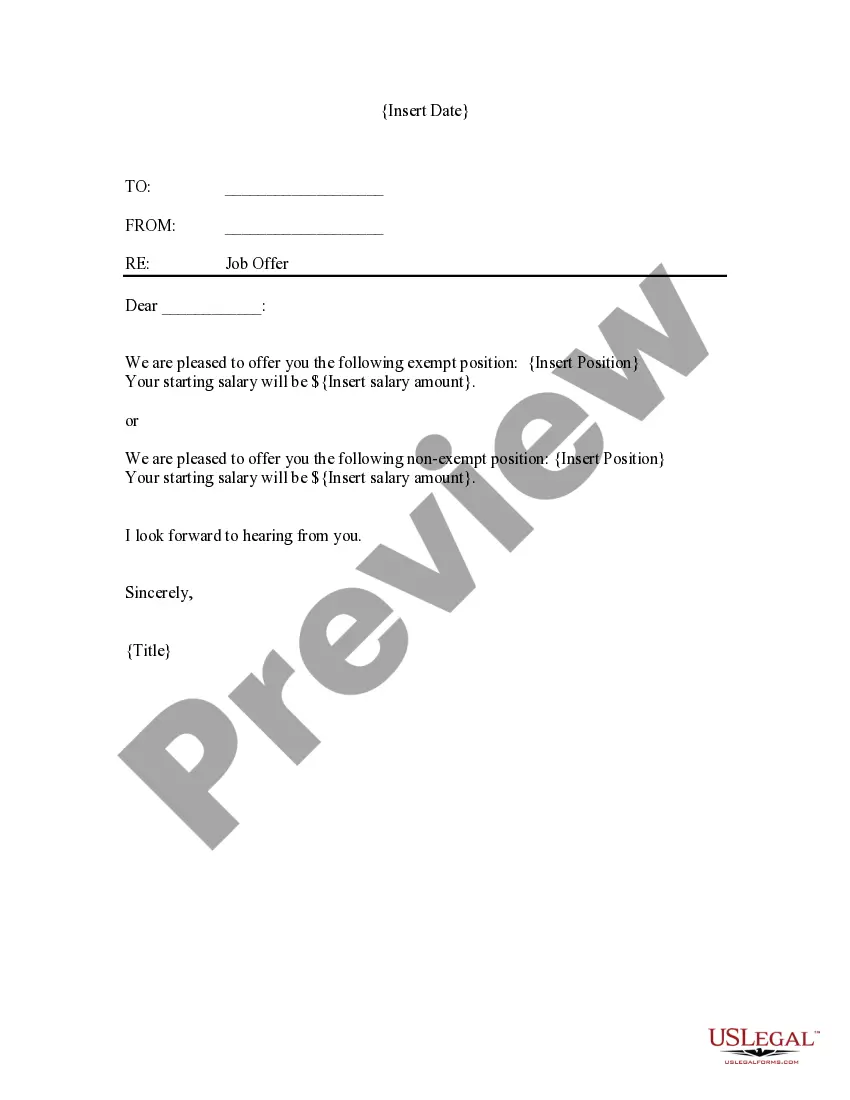
How to fill out Arizona Sample COBRA Enrollment And / Or Waiver Letter?
US Legal Forms - one of the greatest libraries of legitimate varieties in the USA - offers a variety of legitimate document web templates you are able to download or print out. While using site, you can get a large number of varieties for organization and personal functions, sorted by categories, says, or search phrases.You can find the latest models of varieties like the Arizona Sample COBRA Enrollment and / or Waiver Letter within minutes.
If you currently have a membership, log in and download Arizona Sample COBRA Enrollment and / or Waiver Letter from the US Legal Forms catalogue. The Download switch can look on every develop you view. You have accessibility to all in the past downloaded varieties from the My Forms tab of your own accounts.
In order to use US Legal Forms initially, here are easy recommendations to help you get started off:
- Be sure you have chosen the correct develop for your personal city/region. Click the Preview switch to examine the form`s articles. Browse the develop description to actually have selected the proper develop.
- When the develop doesn`t suit your requirements, use the Lookup area near the top of the display screen to obtain the one which does.
- When you are pleased with the form, validate your option by clicking on the Get now switch. Then, opt for the costs prepare you favor and give your credentials to register on an accounts.
- Approach the transaction. Make use of your charge card or PayPal accounts to finish the transaction.
- Select the format and download the form on the system.
- Make modifications. Fill out, revise and print out and signal the downloaded Arizona Sample COBRA Enrollment and / or Waiver Letter.
Each and every format you included in your money does not have an expiry day and is your own forever. So, if you wish to download or print out yet another version, just go to the My Forms portion and click in the develop you want.
Gain access to the Arizona Sample COBRA Enrollment and / or Waiver Letter with US Legal Forms, one of the most comprehensive catalogue of legitimate document web templates. Use a large number of skilled and state-distinct web templates that meet up with your company or personal demands and requirements.