Arizona Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
If you wish to obtain, download, or print valid document templates, utilize US Legal Forms, the foremost collection of legal forms that can be accessed online.
Make use of the site's straightforward and convenient search feature to locate the documents you require. Several templates for business and personal uses are organized by categories and states, or keywords.
Use US Legal Forms to access the Arizona Introductory COBRA Letter in just a few clicks.
Every legal document template you obtain is yours indefinitely. You have access to every form you acquired through your account. Check the My documents section and select a form to print or download again.
Acquire, download, and print the Arizona Introductory COBRA Letter with US Legal Forms. There are numerous professional and state-specific forms available for your business or personal needs.
- If you are already a US Legal Forms user, Log In to your account and click the Obtain button to find the Arizona Introductory COBRA Letter.
- You can also view forms you previously obtained in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct city/state.
- Step 2. Utilize the Preview option to review the content of the form. Don’t forget to check the description.
- Step 3. If you are not satisfied with the form, use the Search box at the top of the screen to find other versions of the legal form template.
- Step 4. Once you have found the form you need, select the Get now button. Choose the pricing plan you prefer and enter your details to create an account.
- Step 5. Process the transaction. You can use your credit card or PayPal account to complete the purchase.
- Step 6. Choose the format of your legal form and download it onto your device.
- Step 7. Complete, modify, and print or sign the Arizona Introductory COBRA Letter.
Form popularity
FAQ
COBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
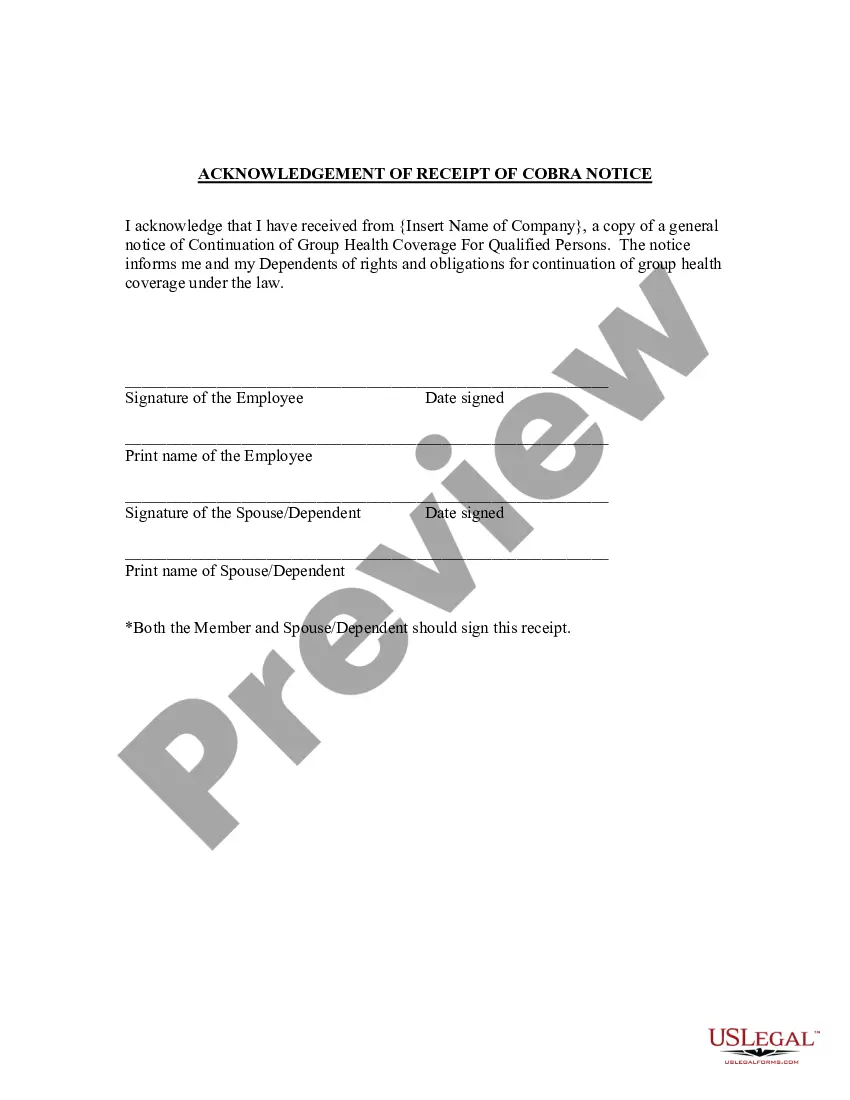
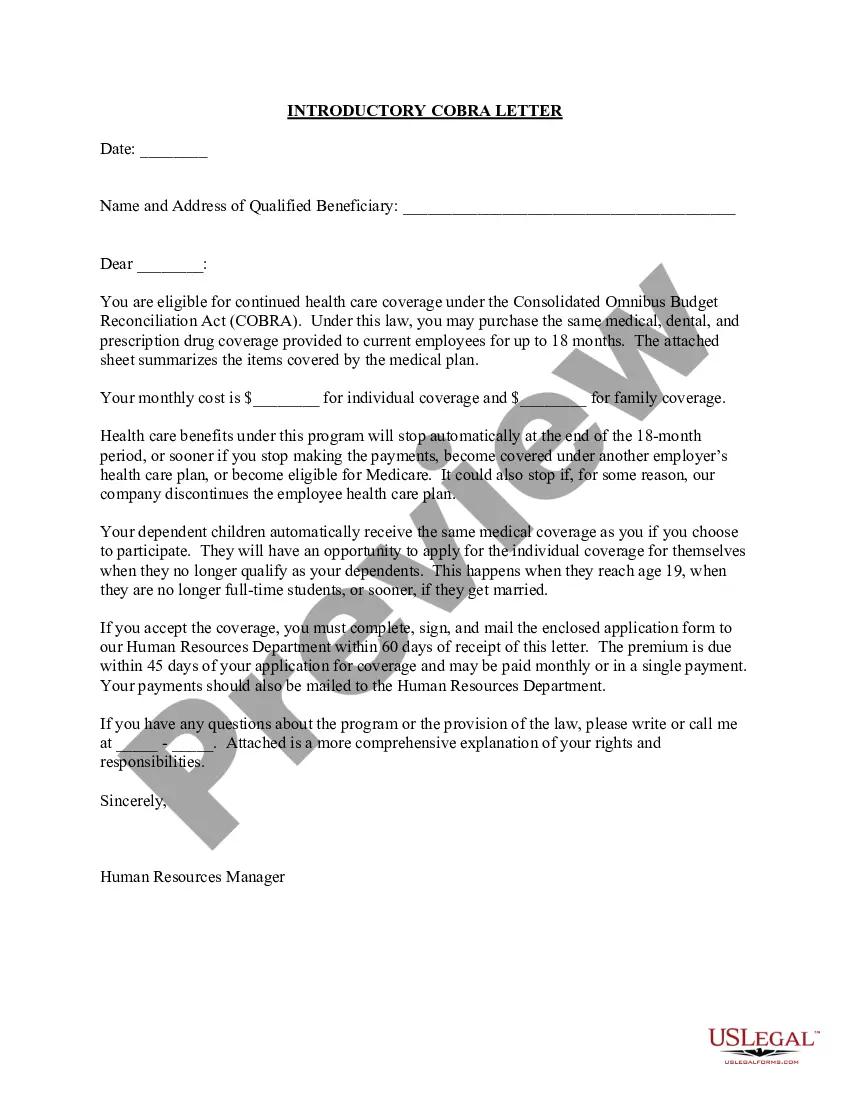
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.