Title: Understanding Arizona Individual Notice of Preexisting Condition Exclusion: Types and Detailed Description Introduction: In Arizona, health insurance providers are required to provide individuals with a Notice of Preexisting Condition Exclusion before enrolling them in a health insurance plan. This notice helps individuals understand any exclusions related to preexisting medical conditions that may affect their coverage. This article aims to provide a comprehensive overview of the Arizona Individual Notice of Preexisting Condition Exclusion, including its types, implications, and the steps one can take to navigate this process effectively. Keywords: Arizona, individual, notice, preexisting condition exclusion, health insurance, coverage, types, implications, navigate, process. Types of Arizona Individual Notice of Preexisting Condition Exclusion: 1. Standard Exclusion: This type of exclusion typically covers any health condition or illness that an individual had before obtaining the insurance coverage. The insurer may impose a waiting period during which these preexisting conditions might not be covered or may apply higher premiums. 2. Extended Exclusion: Unlike standard exclusions, extended exclusions often involve longer waiting periods before the preexisting conditions are covered by the insurance plan. Insurance providers extend the waiting periods if an individual has recently received treatment for a particular condition. 3. Modified Exclusion: Under a modified exclusion, some preexisting conditions may be covered after a reduced waiting period or with specific limitations. The insurer may define these limitations based on the condition's severity, treatment history, or other relevant factors. Detailed Description and Implications: When individuals receive a Notice of Preexisting Condition Exclusion, it is crucial to review the information thoroughly to understand the implications and limitations associated with their health insurance coverage. Here are some key aspects to consider: 1. Clear Statement of Preexisting Conditions: The notice should explicitly list the preexisting conditions that will be excluded or subject to waiting periods. This clarity helps individuals gauge the potential impact on their coverage. 2. Waiting Periods: The notice should provide detailed information on waiting periods, if applicable. Waiting periods typically range from six months to a year, during which treatments related to the excluded conditions will not be covered or only partially covered. 3. Premium Adjustments: In certain cases, individuals with preexisting conditions may face higher premiums due to the insurer perceiving them as higher-risk individuals. The notice should clearly outline any premium adjustments based on the individual's health condition. 4. Appeals and Special Enrollment Periods: Individuals who believe they have been unfairly categorized or wish to challenge the exclusion can explore the avenues for appealing the decision. Also, certain circumstances, such as losing other coverage or life events, may trigger a special enrollment period which allows individuals to obtain coverage without facing preexisting condition exclusions. Navigating the Process Effectively: To navigate the Arizona Individual Notice of Preexisting Condition Exclusion effectively, individuals are advised to take the following steps: 1. Seek Clarification: If any aspect of the notice is unclear or confusing, reach out to the insurance provider for further clarification. Understanding the terms and conditions is vital to make informed decisions. 2. Compare Insurance Plans: Before finalizing a health insurance plan, compare different options available in the market. This comparison can help identify plans with reasonable waiting periods, comprehensive coverage, and competitive premiums. 3. Explore Assistance Programs: Arizona offers various assistance programs for individuals facing difficulties due to preexisting conditions. Investigate if you might be eligible for programs such as Arizona Health Care Cost Containment System (AHC CCS) or other assistance programs, which can provide additional support. Conclusion: The Arizona Individual Notice of Preexisting Condition Exclusion plays a vital role in helping individuals understand the impact of their preexisting conditions on their health insurance coverage. By thoroughly reviewing the notice, individuals can make informed decisions, explore available options, and effectively navigate the process, ultimately securing suitable health insurance coverage. (Note: This content is for informational purposes only and should not be considered legal or professional advice. Individuals should consult with qualified professionals or the Arizona Department of Insurance for specific guidance regarding their situation.)
Arizona Individual Notice of Preexisting Condition Exclusion
Description
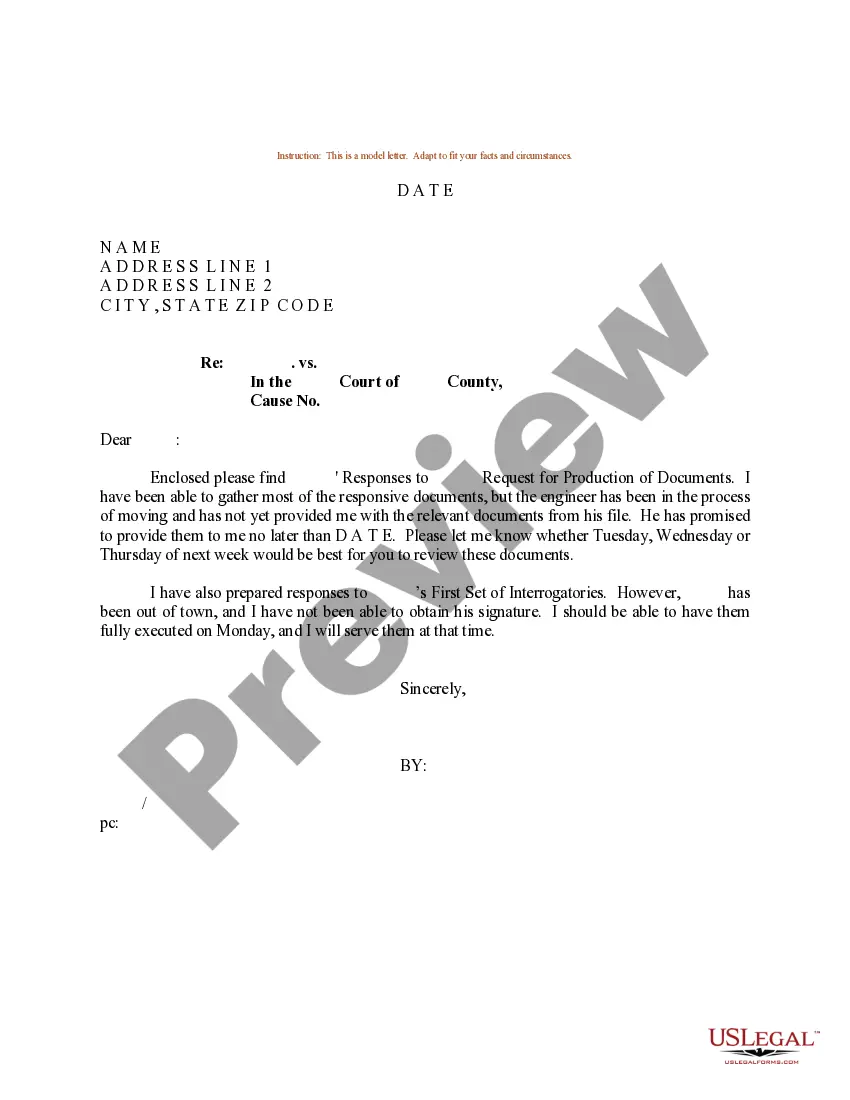
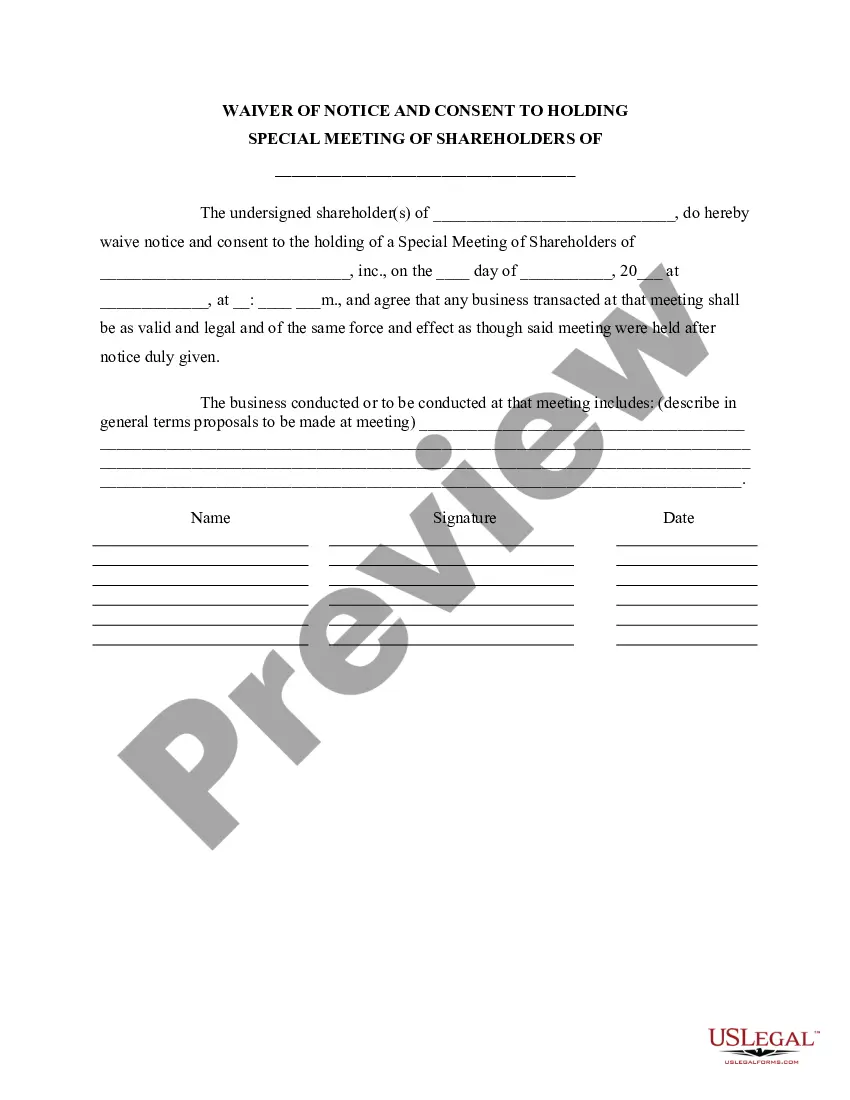
How to fill out Arizona Individual Notice Of Preexisting Condition Exclusion?
You can invest time online searching for the legitimate file design that fits the state and federal specifications you need. US Legal Forms gives a huge number of legitimate varieties which are analyzed by pros. It is possible to obtain or printing the Arizona Individual Notice of Preexisting Condition Exclusion from my support.
If you already possess a US Legal Forms profile, you can log in and click on the Acquire button. Following that, you can comprehensive, revise, printing, or sign the Arizona Individual Notice of Preexisting Condition Exclusion. Each and every legitimate file design you buy is yours eternally. To have yet another copy associated with a purchased develop, proceed to the My Forms tab and click on the related button.
If you use the US Legal Forms site initially, follow the simple instructions beneath:
- Very first, make certain you have selected the proper file design for that state/metropolis that you pick. See the develop information to make sure you have selected the correct develop. If offered, take advantage of the Review button to look with the file design as well.
- If you want to find yet another model in the develop, take advantage of the Look for area to discover the design that meets your needs and specifications.
- Once you have discovered the design you would like, click Get now to continue.
- Choose the pricing prepare you would like, type your references, and sign up for an account on US Legal Forms.
- Full the financial transaction. You can use your bank card or PayPal profile to fund the legitimate develop.
- Choose the format in the file and obtain it for your gadget.
- Make changes for your file if necessary. You can comprehensive, revise and sign and printing Arizona Individual Notice of Preexisting Condition Exclusion.
Acquire and printing a huge number of file layouts using the US Legal Forms Internet site, that provides the most important assortment of legitimate varieties. Use professional and status-distinct layouts to tackle your business or personal needs.
Form popularity
FAQ
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
There might be a scenario's where system determines records for more than one condition type in the pricing procedure. In order to avoid this we can set up conditions or a group of conditions to be mutually exclusive. This is called condition exclusion.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Examples of pre-existing conditions include cancer, asthma, diabetes, and even pregnancy. Under the Affordable Care Act (Obamacare), health insurance companies cannot refuse to cover you because of any pre-existing conditions nor can they charge you more money for coverage or subject you to a waiting period.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.