The California Model General Notice of COBRA Continuation Coverage Rights is an important document that provides detailed information regarding an individual's rights to continue their health coverage under COBRA (Consolidated Omnibus Budget Reconciliation Act). This notice is specific to individuals residing in California and outlines various essential details and rights related to COBRA continuation coverage. The purpose of the California Model General Notice is to inform employees and their dependents about their rights to continue health coverage in the event of job loss, reduced work hours, or other qualifying events that may result in a loss of coverage. The notice must be provided by employers who are subject to federal COBRA laws and who have employed 20 or more individuals in the previous calendar year. Key topics covered in the California Model General Notice include the definition of a qualifying event, the eligibility criteria for COBRA continuation coverage, the steps that need to be taken to enroll in COBRA, the duration of coverage, and the associated costs. The notice also provides details on the importance of notifying the plan administrator promptly in the case of a qualifying event and the possible consequences of failing to do so within the specified time frame. The California Model General Notice also highlights the rights and responsibilities of both the employer and the qualifying individual. It explains the need for premium payments to ensure continuous coverage and provides information on grace periods for payment, as well as the potential for termination of coverage for non-payment. Different types of California Model General Notice of COBRA Continuation Coverage Rights may exist depending on variations in state-specific regulations, updates, or changes to COBRA provisions. Employers should ensure they have the most up-to-date version that complies with both federal COBRA requirements and any additional state-specific guidelines. In conclusion, the California Model General Notice of COBRA Continuation Coverage Rights serves as a vital tool for educating employees and their dependents about their entitlement to continued health coverage. By comprehensively explaining the eligibility criteria, enrollment procedures, and responsibilities of both employers and individuals, this notice helps ensure that individuals can make informed decisions about their healthcare options when facing qualifying events that may result in a loss of coverage.
California Model General Notice of COBRA Continuation Coverage Rights
Description
How to fill out California Model General Notice Of COBRA Continuation Coverage Rights?
You can spend hrs on-line looking for the legitimate papers format which fits the state and federal requirements you need. US Legal Forms offers a large number of legitimate types which can be evaluated by pros. It is possible to down load or print out the California Model General Notice of COBRA Continuation Coverage Rights from our services.
If you already have a US Legal Forms bank account, you are able to log in and click the Download switch. Following that, you are able to total, revise, print out, or indication the California Model General Notice of COBRA Continuation Coverage Rights. Each legitimate papers format you acquire is the one you have eternally. To acquire yet another backup associated with a purchased type, go to the My Forms tab and click the related switch.
If you are using the US Legal Forms website the first time, keep to the basic guidelines below:
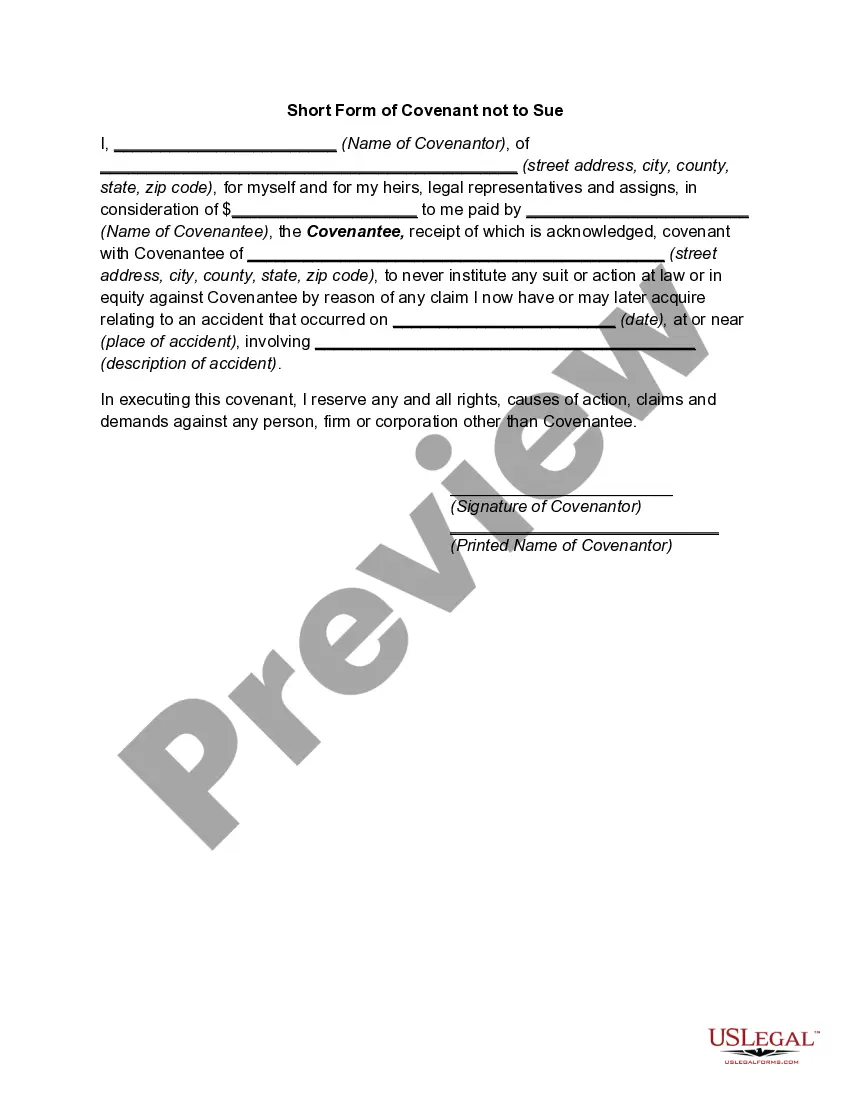
- Initial, ensure that you have chosen the correct papers format for your state/metropolis of your choosing. See the type description to make sure you have selected the proper type. If accessible, make use of the Preview switch to appear with the papers format at the same time.
- If you want to locate yet another edition from the type, make use of the Research field to obtain the format that suits you and requirements.
- Once you have identified the format you want, simply click Purchase now to continue.
- Pick the prices program you want, type your credentials, and sign up for a merchant account on US Legal Forms.
- Comprehensive the transaction. You should use your credit card or PayPal bank account to purchase the legitimate type.
- Pick the file format from the papers and down load it to the device.
- Make alterations to the papers if possible. You can total, revise and indication and print out California Model General Notice of COBRA Continuation Coverage Rights.
Download and print out a large number of papers web templates utilizing the US Legal Forms website, that offers the biggest selection of legitimate types. Use professional and condition-distinct web templates to deal with your company or person requirements.