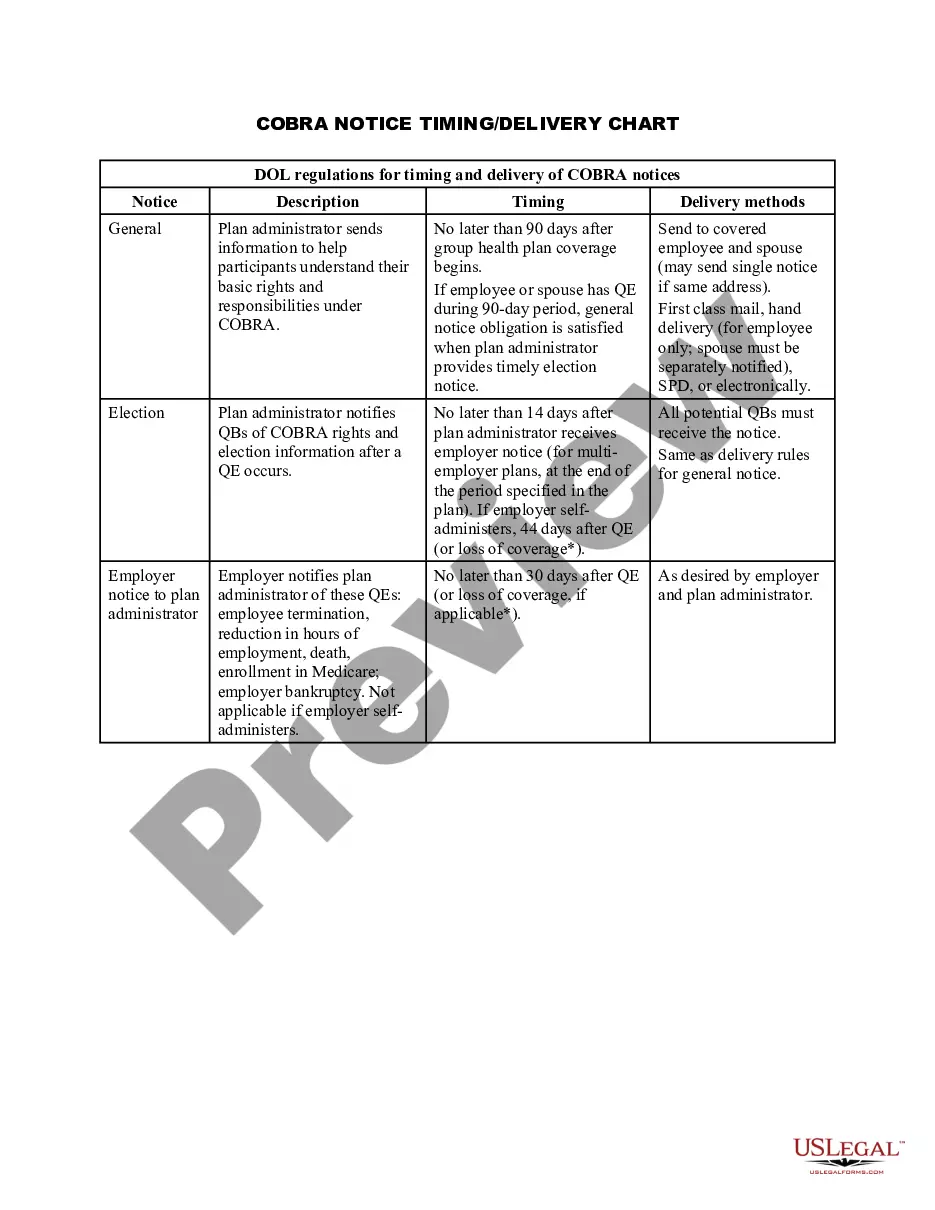
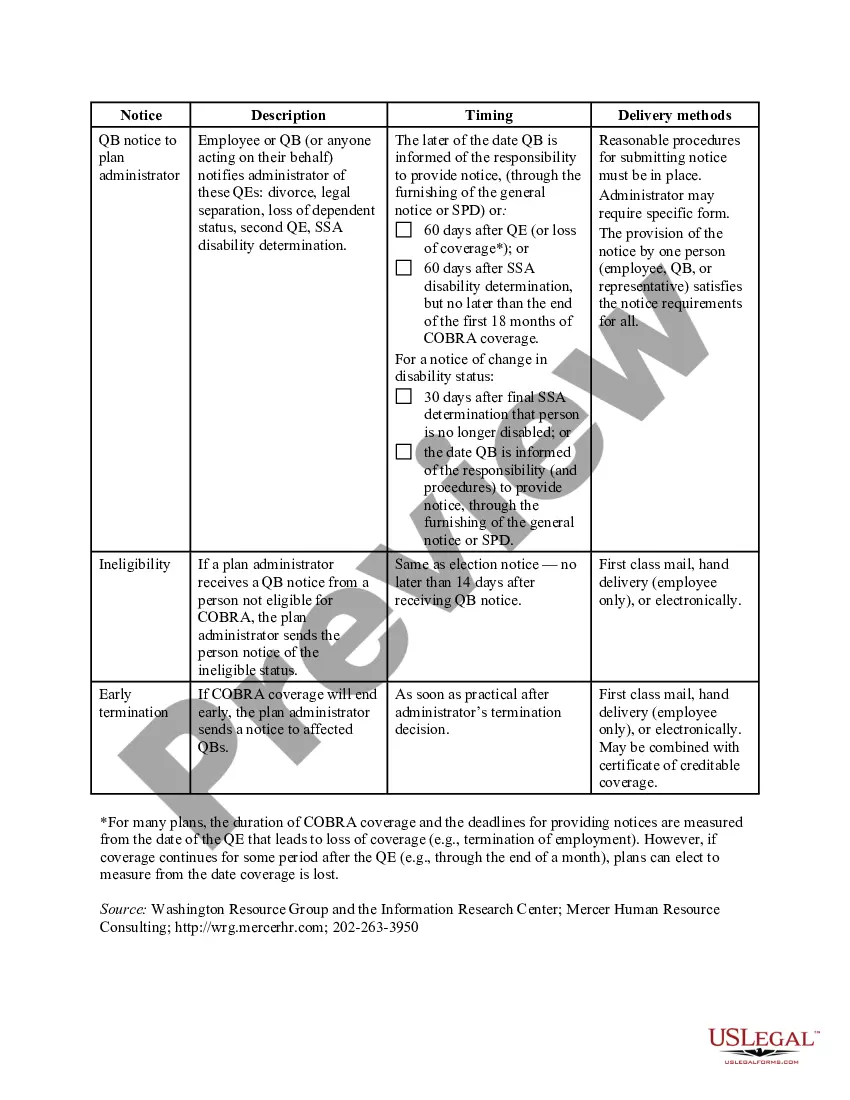
The California COBRA Notice Timing Delivery Chart is an essential resource that outlines the specific timelines and requirements for delivering COBRA notices to eligible employees in the state of California. This comprehensive chart helps employers and benefits administrators stay compliant with California state law and ensures that employees receive the necessary information regarding their continuation of health insurance coverage. The California COBRA Notice Timing Delivery Chart provides detailed information on the various types of COBRA notices and their respective delivery timelines. The chart includes the following types of notices: 1. Initial Notice: This notice must be provided to employees and their covered dependents within 90 days of the start of their health insurance coverage. It informs them of their rights under COBRA and explains the eligibility requirements for continuation coverage. 2. Qualifying Event Notice: When a qualifying event, such as termination of employment or divorce, occurs, this notice must be delivered to the affected individual and any covered dependents within 30 days. It informs them of their right to elect COBRA continuation coverage and explains the procedures and deadlines for doing so. 3. Notice of Unavailability or Cancellation of Continuation Coverage: If an employer or health plan becomes unable to provide COBRA continuation coverage, this notice must be sent to affected individuals within 14 days of the determination. It explains the reason for the unavailability or cancellation and provides alternative options for obtaining health insurance coverage. 4. Notice of Conversion Privileges: In certain circumstances, employees and covered dependents may be eligible to convert their group health plan coverage to an individual policy. This notice must be provided within 14 days of the determination of eligibility and outlines the conversion options available to them. The California COBRA Notice Timing Delivery Chart is an invaluable tool for employers and benefits administrators, allowing them to navigate the complex rules and regulations set forth by California state law. By following the timelines and guidelines outlined in the chart, employers can ensure that eligible employees receive the necessary COBRA notices in a timely manner, promoting transparency and compliance in the continuation of health insurance coverage.
California COBRA Notice Timing Delivery Chart
Description
How to fill out California COBRA Notice Timing Delivery Chart?
If you wish to full, obtain, or print legitimate document web templates, use US Legal Forms, the biggest variety of legitimate kinds, that can be found on the Internet. Use the site`s simple and easy hassle-free lookup to find the documents you require. A variety of web templates for enterprise and individual functions are sorted by groups and says, or key phrases. Use US Legal Forms to find the California COBRA Notice Timing Delivery Chart within a number of click throughs.
Should you be currently a US Legal Forms client, log in to your profile and click on the Down load button to obtain the California COBRA Notice Timing Delivery Chart. You can even access kinds you formerly acquired inside the My Forms tab of the profile.
If you use US Legal Forms the very first time, follow the instructions under:
- Step 1. Make sure you have chosen the form for that right area/region.
- Step 2. Utilize the Review method to check out the form`s articles. Never forget about to learn the information.
- Step 3. Should you be unhappy using the type, make use of the Lookup discipline at the top of the screen to locate other variations of your legitimate type format.
- Step 4. When you have found the form you require, click the Buy now button. Pick the pricing prepare you favor and put your references to sign up for an profile.
- Step 5. Approach the deal. You may use your credit card or PayPal profile to finish the deal.
- Step 6. Choose the file format of your legitimate type and obtain it on your gadget.
- Step 7. Full, revise and print or indicator the California COBRA Notice Timing Delivery Chart.
Every legitimate document format you acquire is your own property permanently. You have acces to each type you acquired within your acccount. Select the My Forms area and decide on a type to print or obtain again.
Contend and obtain, and print the California COBRA Notice Timing Delivery Chart with US Legal Forms. There are thousands of skilled and state-certain kinds you can use for your enterprise or individual requirements.
Form popularity
FAQ
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event. You are responsible for making sure your COBRA coverage goes into and stays in effect - if you do not ask for COBRA coverage before the deadline, you may lose your right to COBRA coverage.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
Covered Employers Under federal COBRA, employers with 20 or more employees are usually required to offer COBRA coverage. COBRA applies to plans maintained by private-sector employers (including self-insured plans) and those sponsored by most state and local governments.