The California General Notice of Preexisting Condition Exclusion is an important document that outlines the rules and regulations regarding the exclusion of preexisting medical conditions in health insurance coverage. This notice is specifically required by the state of California to be provided to individuals seeking health insurance coverage. A "preexisting condition" refers to any health condition or illness that an individual has prior to obtaining health insurance coverage. California, like many other states, has regulations in place to protect individuals with preexisting conditions from being denied coverage or facing higher premiums. The General Notice of Preexisting Condition Exclusion is designed to inform individuals about their rights and the limitations of coverage related to preexisting conditions. The notice explains that insurance companies in California are allowed to exclude coverage related to preexisting conditions for a certain period of time. However, the specifics of these exclusion periods may vary depending on the type of health insurance plan. It is crucial for individuals to read the notice carefully to fully understand what is covered, what is excluded, and for how long. There are typically three types of California General Notice of Preexisting Condition Exclusion: 1. Individual Health Insurance: This type of exclusion applies to individuals who are purchasing health insurance coverage on their own, outside any group or employer-sponsored plans. The notice will specify the length of the exclusion period, which typically ranges from six months to one year. 2. Group Health Insurance: The notice provides details about preexisting condition exclusions for individuals who obtain health insurance coverage through an employer or group plan. It may outline specific waiting periods and any limitations on coverage for preexisting conditions. 3. Health Maintenance Organization (HMO) Plans: are a type of managed care health insurance plan. The General Notice of Preexisting Condition Exclusion for HMO plans will explain the terms and limitations related to preexisting conditions within the HMO network. It may include information about waiting periods or restrictions on certain treatments or services. It is crucial for individuals to carefully review the California General Notice of Preexisting Condition Exclusion before purchasing or enrolling in a health insurance plan. By understanding the limitations and coverage options related to preexisting conditions, individuals can make more informed decisions about their healthcare needs and ensure they have access to the necessary medical services.
California General Notice of Preexisting Condition Exclusion
Description
How to fill out California General Notice Of Preexisting Condition Exclusion?
It is possible to commit hrs on-line attempting to find the legitimate file template which fits the state and federal requirements you require. US Legal Forms provides 1000s of legitimate forms that are analyzed by experts. It is possible to download or printing the California General Notice of Preexisting Condition Exclusion from our service.
If you already possess a US Legal Forms bank account, it is possible to log in and then click the Obtain key. Following that, it is possible to full, edit, printing, or signal the California General Notice of Preexisting Condition Exclusion. Every single legitimate file template you purchase is the one you have permanently. To get one more backup for any purchased form, visit the My Forms tab and then click the related key.
If you use the US Legal Forms site for the first time, adhere to the straightforward guidelines under:
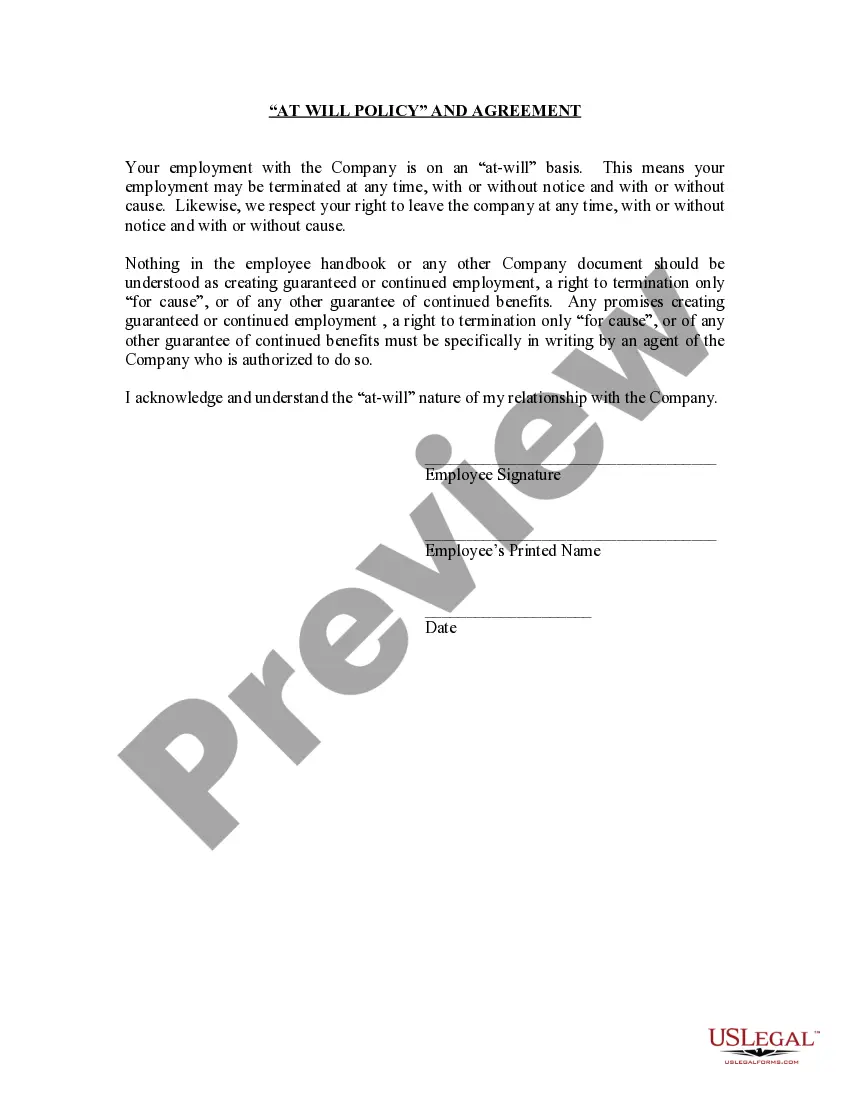
- Initially, make certain you have chosen the proper file template for the area/metropolis that you pick. Read the form outline to make sure you have chosen the appropriate form. If accessible, take advantage of the Review key to look with the file template too.
- In order to locate one more variation of the form, take advantage of the Look for field to get the template that meets your needs and requirements.
- Once you have identified the template you would like, click Acquire now to move forward.
- Choose the prices program you would like, enter your accreditations, and sign up for a free account on US Legal Forms.
- Total the purchase. You can use your charge card or PayPal bank account to fund the legitimate form.
- Choose the formatting of the file and download it to the device.
- Make adjustments to the file if required. It is possible to full, edit and signal and printing California General Notice of Preexisting Condition Exclusion.
Obtain and printing 1000s of file templates using the US Legal Forms Internet site, which provides the largest assortment of legitimate forms. Use specialist and express-specific templates to deal with your business or personal requires.