The Colorado Notice of Special Enrollment Rules refers to regulations that govern the conditions and procedures for individuals to enroll in or make changes to their health insurance coverage outside the typical open enrollment period. These rules guarantee certain opportunities for individuals to obtain or modify their health insurance plans in specific situations, ensuring access to necessary healthcare services. Implementing these rules guarantees fair and consistent processes for Coloradans to acquire or modify their coverage when they experience qualifying events or exceptional circumstances. There are several types of Colorado Notice of Special Enrollment Rules, each catering to different situations that may necessitate enrollment outside the regular enrollment period. These include: 1. Qualifying Life Events (Ales): Ales are life-changing events that allow individuals to enroll in or make changes to their health insurance plans. Examples of Ales include getting married, having a baby, adopting a child, losing other health coverage, or moving to Colorado. Individuals experiencing Ales can take advantage of the special enrollment period provided under these rules to ensure adequate coverage. 2. Medicaid and Children's Health Insurance Program (CHIP): The Colorado Notice of Special Enrollment Rules also addresses eligibility for Medicaid and CHIP, allowing individuals who qualify for these programs to enroll or modify their coverage outside the regular enrollment period. This ensures that those who meet the necessary criteria can access the benefits and services provided by these programs. 3. Native Americans: Special enrollment rules are in place for Native Americans, recognizing their unique circumstances and federal obligations. These rules provide additional flexibility and opportunities for Native Americans to enroll in or change their health insurance coverage. 4. Loss of Minimum Essential Coverage: Individuals who lose their minimum essential coverage due to reasons like the expiration of COBRA coverage, loss of eligibility for Medicaid or CHIP, or the termination of a student health plan are eligible for special enrollment. The Colorado Notice of Special Enrollment Rules addresses these circumstances to prevent individuals from being left without coverage. 5. Exceptional Circumstances: In certain exceptional cases, individuals may face unique circumstances that prevent them from enrolling during the standard enrollment period. The Notice of Special Enrollment Rules provides provisions for individuals affected by exceptional circumstances, ensuring they are not denied access to health insurance coverage due to unforeseen events. In summary, the Colorado Notice of Special Enrollment Rules outlines the various circumstances and events that allow individuals to enroll in or modify their health insurance coverage outside the regular enrollment period. By defining eligibility criteria and establishing procedures, these rules ensure equitable access to healthcare services for Coloradans facing qualifying life events, exceptional circumstances, or those needing assistance with Medicaid and CHIP enrollment.
Colorado Notice of Special Enrollment Rules
Description
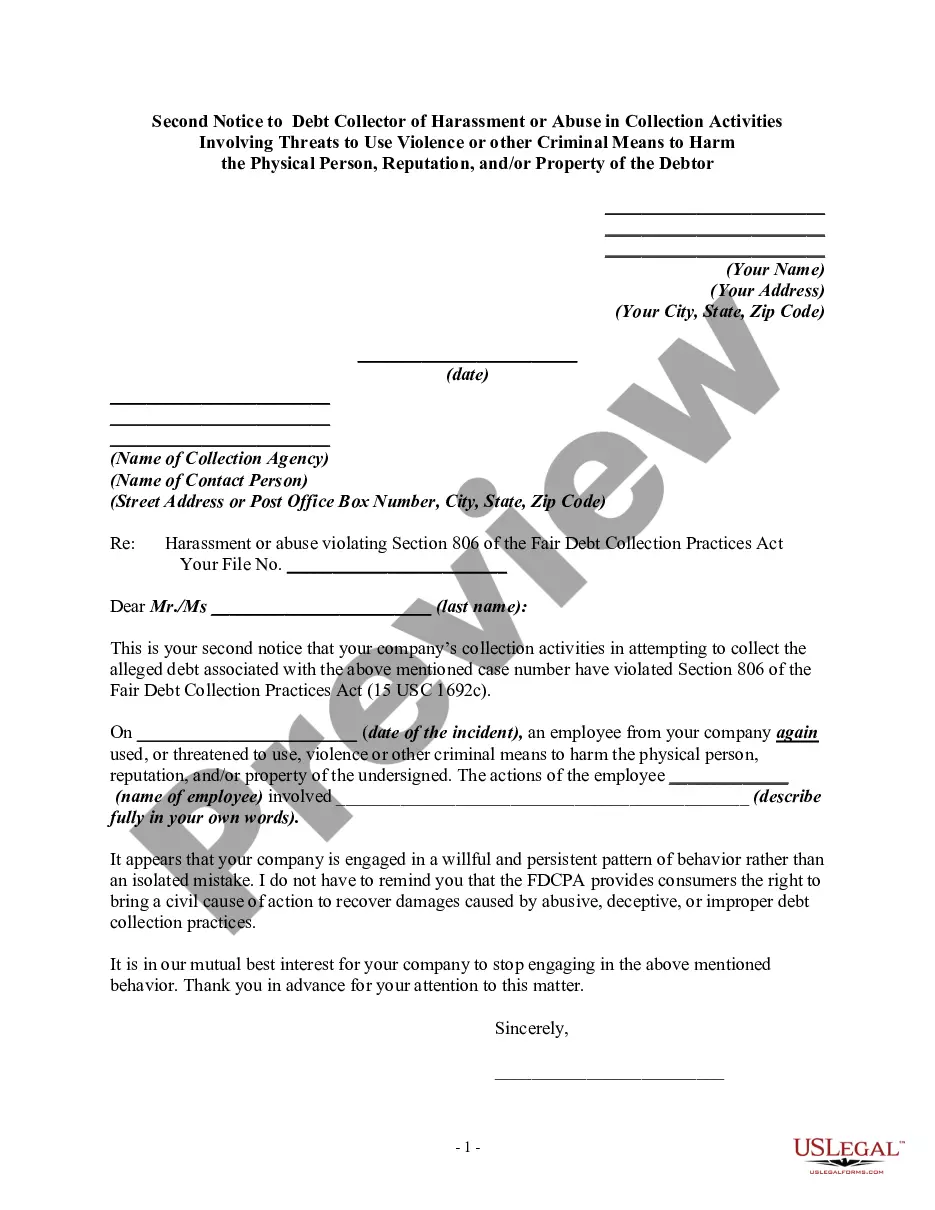
How to fill out Colorado Notice Of Special Enrollment Rules?
Choosing the best authorized papers template can be quite a have a problem. Obviously, there are a variety of layouts available on the Internet, but how will you get the authorized type you require? Take advantage of the US Legal Forms internet site. The service offers a huge number of layouts, like the Colorado Notice of Special Enrollment Rules, that can be used for enterprise and personal requires. All the types are checked by professionals and meet state and federal demands.
If you are currently registered, log in to the profile and click on the Acquire switch to have the Colorado Notice of Special Enrollment Rules. Make use of your profile to appear through the authorized types you might have acquired formerly. Proceed to the My Forms tab of your own profile and have yet another backup of your papers you require.
If you are a whole new consumer of US Legal Forms, listed below are straightforward directions so that you can follow:
- Initially, be sure you have chosen the correct type for your personal city/region. It is possible to look over the shape utilizing the Preview switch and browse the shape explanation to make sure this is basically the best for you.
- In case the type does not meet your preferences, make use of the Seach industry to get the right type.
- When you are positive that the shape is proper, select the Purchase now switch to have the type.
- Pick the costs prepare you need and type in the essential information. Make your profile and pay money for the order with your PayPal profile or Visa or Mastercard.
- Opt for the submit structure and down load the authorized papers template to the device.
- Complete, edit and print and signal the attained Colorado Notice of Special Enrollment Rules.
US Legal Forms may be the most significant catalogue of authorized types that you can find different papers layouts. Take advantage of the service to down load professionally-manufactured paperwork that follow condition demands.