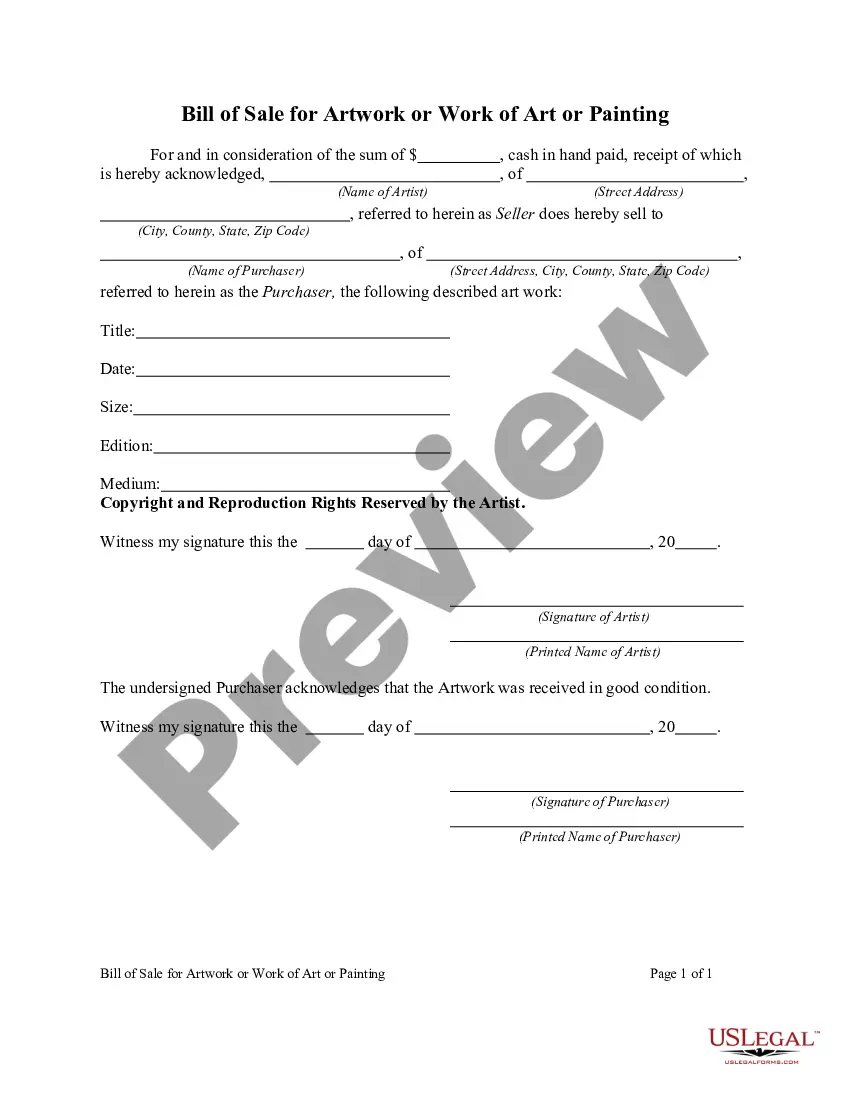
Connecticut Health Record Amendment Denial Letter is a formal document issued by medical entities or healthcare providers in Connecticut to inform patients about the rejection or denial of a requested amendment to their medical records. This letter serves to explain the reasons behind the denial and provides necessary information regarding patients' rights to address the issue further. The denial letter may contain several types, depending on the circumstances and reasons for denial: 1. Medical Inaccuracy: If a requested amendment is deemed inaccurate based on medical evidence or professional judgment, a denial letter emphasizing this reason may be issued. It would explain the specific inaccuracies identified within the requested amendment and provide relevant medical details or explanations supporting the denial. 2. Legal Grounds: In cases where the requested amendment conflicts with legal regulations or obligations, such as privacy laws or retention periods, a denial letter citing the legal grounds may be issued. This letter would outline the specific law or regulation supporting the denial and may provide information on patient rights to seek further clarifications or recourse. 3. Untimely Request: Patients are often required to submit their amendment requests within a certain timeframe. If a request is received after the designated time limit, a denial letter highlighting the untimeliness may be generated. It would include information regarding the timeline requirements, reasons for the strict adherence, and potential alternatives available to patients. 4. Insufficient Justification: Occasionally, patients may fail to provide sufficient justification for their requested amendments, warranting a denial letter. The letter would explain the reasons for considering the provided justification inadequate and may provide guidance on how patients can resubmit their request with more comprehensive supporting evidence. 5. Invalid Authorization: In cases where the amendment request lacks proper authorization or fails to meet the necessary requirements, healthcare facilities may issue a denial letter emphasizing the invalid authorization as the basis for denial. The letter would specify the missing or incorrect information, providing instructions on how patients can rectify the issue and resubmit their amendment request. 6. Duplicate or Redundant Requests: Patients sometimes submit multiple requests for the same amendment, either intentionally or inadvertently. In such cases, a denial letter highlighting the presence of duplicate or redundant requests may be sent, explaining the need for a single, consolidated request and listing the subsequent steps patients can take to ensure their request is validly considered. It is essential to note that these described denial letter types are not exhaustive, and the specific format and content may vary based on individual healthcare providers or medical institutions in Connecticut. The purpose of the denial letter remains consistent: to inform patients about the rejection of their medical record amendment request and provide necessary explanations, guidance, and patient rights information.
Connecticut Health Record Amendment Denial Letter
Description
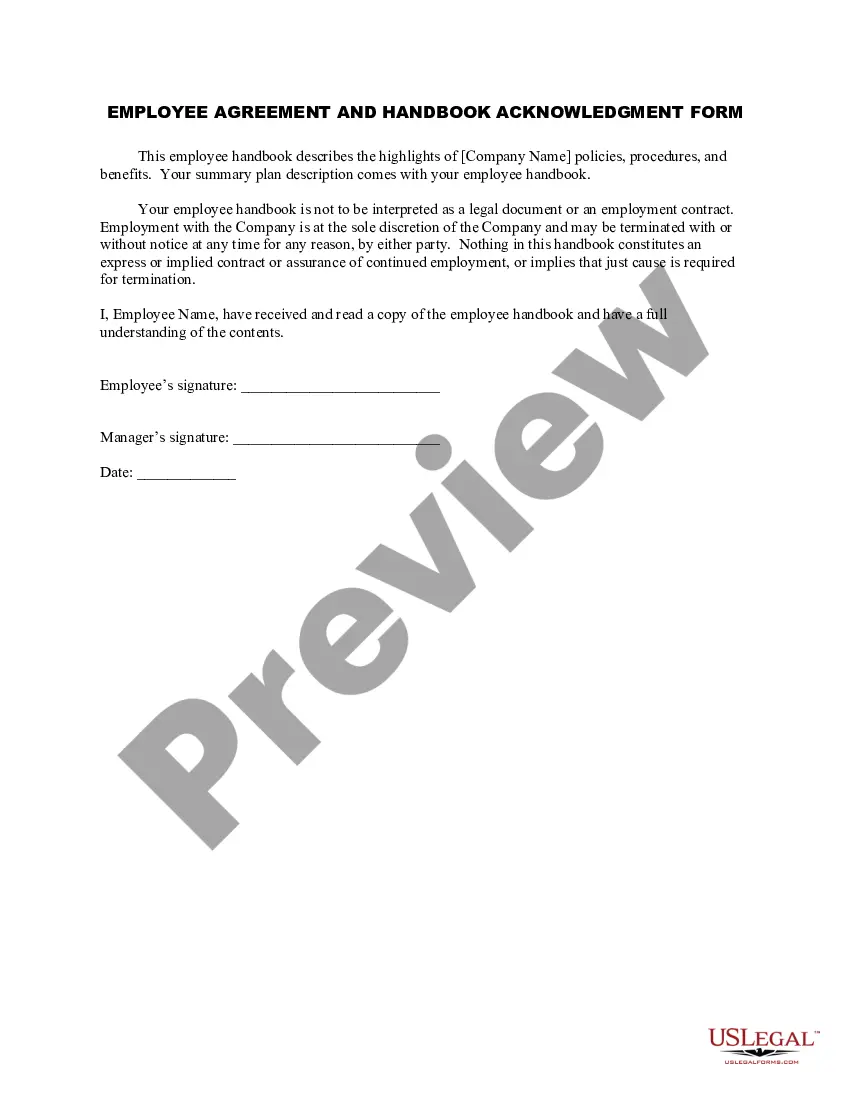
How to fill out Connecticut Health Record Amendment Denial Letter?
US Legal Forms - one of the biggest libraries of lawful types in the States - gives a wide range of lawful document web templates you may acquire or printing. While using website, you may get 1000s of types for business and personal purposes, sorted by categories, states, or keywords.You can find the latest models of types much like the Connecticut Health Record Amendment Denial Letter within minutes.
If you already have a registration, log in and acquire Connecticut Health Record Amendment Denial Letter in the US Legal Forms local library. The Down load switch will show up on every type you look at. You have access to all earlier delivered electronically types within the My Forms tab of your account.
If you would like use US Legal Forms for the first time, allow me to share straightforward directions to get you started out:
- Make sure you have chosen the right type for your town/state. Click on the Preview switch to examine the form`s content material. See the type description to actually have selected the appropriate type.
- In case the type doesn`t satisfy your needs, make use of the Search industry near the top of the display screen to obtain the one who does.
- In case you are happy with the form, confirm your decision by simply clicking the Buy now switch. Then, choose the pricing plan you like and give your credentials to register for an account.
- Process the transaction. Use your Visa or Mastercard or PayPal account to finish the transaction.
- Pick the format and acquire the form on your own product.
- Make changes. Fill up, revise and printing and indication the delivered electronically Connecticut Health Record Amendment Denial Letter.
Every single design you added to your bank account does not have an expiration time and it is yours permanently. So, if you would like acquire or printing an additional duplicate, just go to the My Forms section and then click on the type you require.
Get access to the Connecticut Health Record Amendment Denial Letter with US Legal Forms, the most extensive local library of lawful document web templates. Use 1000s of expert and express-particular web templates that satisfy your organization or personal requires and needs.
Form popularity
FAQ
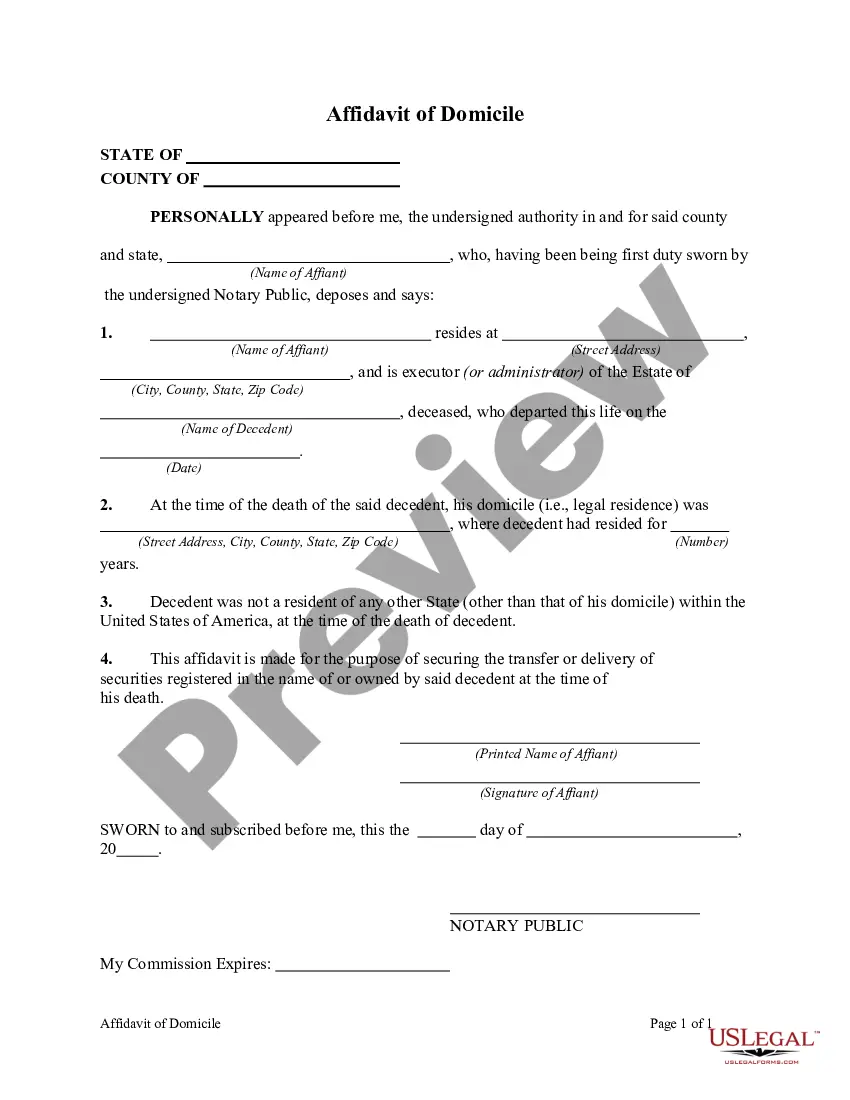
Consequently, patients frequently ask about whether they have the right to remove a diagnosis from their medical records. But, can they do this? The answer to this question is NO.
When the physician discovers an error, such as a progress note that has been inserted into the wrong record or is missing, it must be added as an addendum or corrected in the specific manner. When making a correction on a computerized document, maintain the original entry in the electronic file.
If you think the information in your medical or billing record is incorrect, you can request a change, or amendment, to your record. The health care provider or health plan must respond to your request. If it created the information, it must amend inaccurate or incomplete information.
General concerns about psychological or emotional harm are not sufficient to deny an individual access (e.g., concerns that the individual will not be able to understand the information or may be upset by it). In addition, the requested access must be reasonably likely to cause harm or endanger physical life or safety.
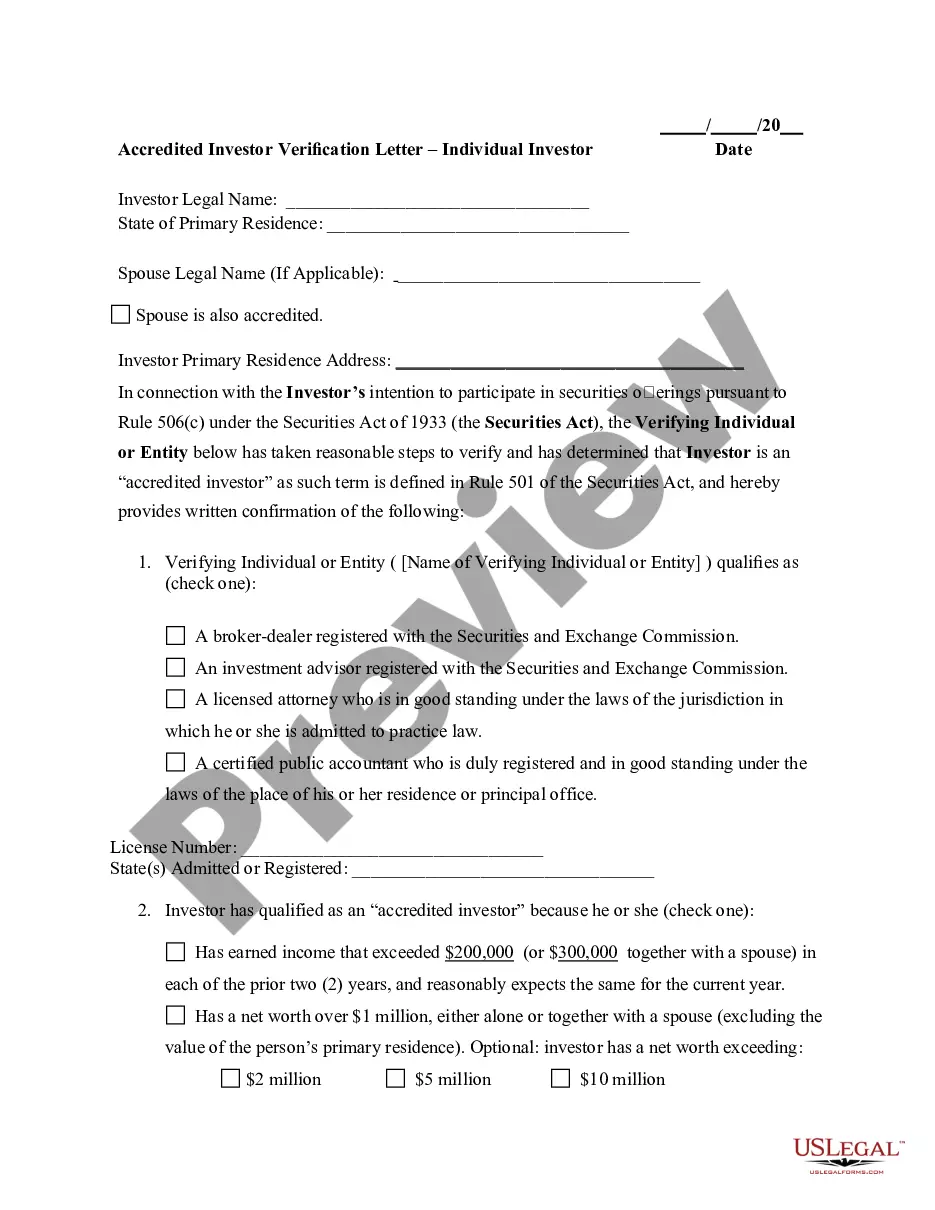
A patient has the right to request an amendment to his or her health record per 45 CFR §164.526 of the HIPAA Privacy Rule, and it is the policy of this organization to respond to any amendment requests in accordance with this rule.
A Medical Record Amendment is: A change, edit or update of medical record information requested by the patient when they feel the information documented is incorrect.
No. A patient's record should be complete and accurate to ensure they receive appropriate care. Patients can question the content of their records, but not on the basis that it is upsetting or that they disagree with it.
Proper Error Correction ProcedureDraw line through entry (thin pen line). Make sure that the inaccurate information is still legible.Initial and date the entry.State the reason for the error (i.e. in the margin or above the note if room).Document the correct information.
Under HIPAA, patients have a right to request amendments to their medical records, but it is up to the provider to decide whether or not to do it. However, regardless of what the provider decides, they must respond to the patient's amendment request.
Reasons for Denial.The provider who received the amendment request had not created the original record. The record was created at another office. There is an exception if the creator is no longer available and the mistake in the record is apparent.