Connecticut Notice of Special Enrollment Rules is a comprehensive set of regulations established by the state of Connecticut to provide individuals with certain opportunities to enroll in health insurance plans outside the standard open enrollment period. These special enrollment rules are designed to ensure that residents have access to affordable and adequate healthcare coverage throughout the year. Under the Connecticut Notice of Special Enrollment Rules, there are several types of special enrollment periods (SEPs) that cater to specific circumstances or life events. These SEPs allow individuals and families to enroll in or make changes to their existing health insurance plans outside the regular open enrollment period, which typically takes place once a year. One type of SEP covered under the Connecticut Notice of Special Enrollment Rules is the loss of qualifying health coverage. This occurs when individuals and families lose their current health insurance coverage due to reasons such as the termination of employment, expiration of a Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage, or eligibility loss for Medicaid or the Children's Health Insurance Program (CHIP). In such cases, individuals have a limited time frame to enroll in a new health insurance plan or make changes to their existing coverage. Another type of SEP is triggered by changes in household size or composition. This includes situations such as getting married or divorced, having a child, adopting a child, or becoming a dependent or losing dependent status. These life events allow individuals to take advantage of the special enrollment period and modify their health insurance plans accordingly to accommodate their new circumstances. Furthermore, individuals who experience a change in place of residence or move to Connecticut from another state are eligible for a special enrollment period. This includes both permanent moves and those due to seasonal employment or student status changes. The Connecticut Notice of Special Enrollment Rules acknowledges that relocating can disrupt an individual's access to healthcare, and therefore provides an opportunity for them to obtain or switch to a new health insurance plan. Lastly, individuals who gain citizenship or lawful presence in the United States, become members of a federally recognized tribe, or qualify for a Special Enrollment Period based on exceptional circumstances are also eligible to apply under the Connecticut Notice of Special Enrollment Rules. It is crucial for Connecticut residents to be aware of these various SEPs to ensure they can access healthcare coverage when they need it the most. By understanding the Connecticut Notice of Special Enrollment Rules and the different types of special enrollment periods, individuals can make informed decisions about their health insurance options and secure adequate coverage tailored to their specific situations.
Connecticut Notice of Special Enrollment Rules
Description
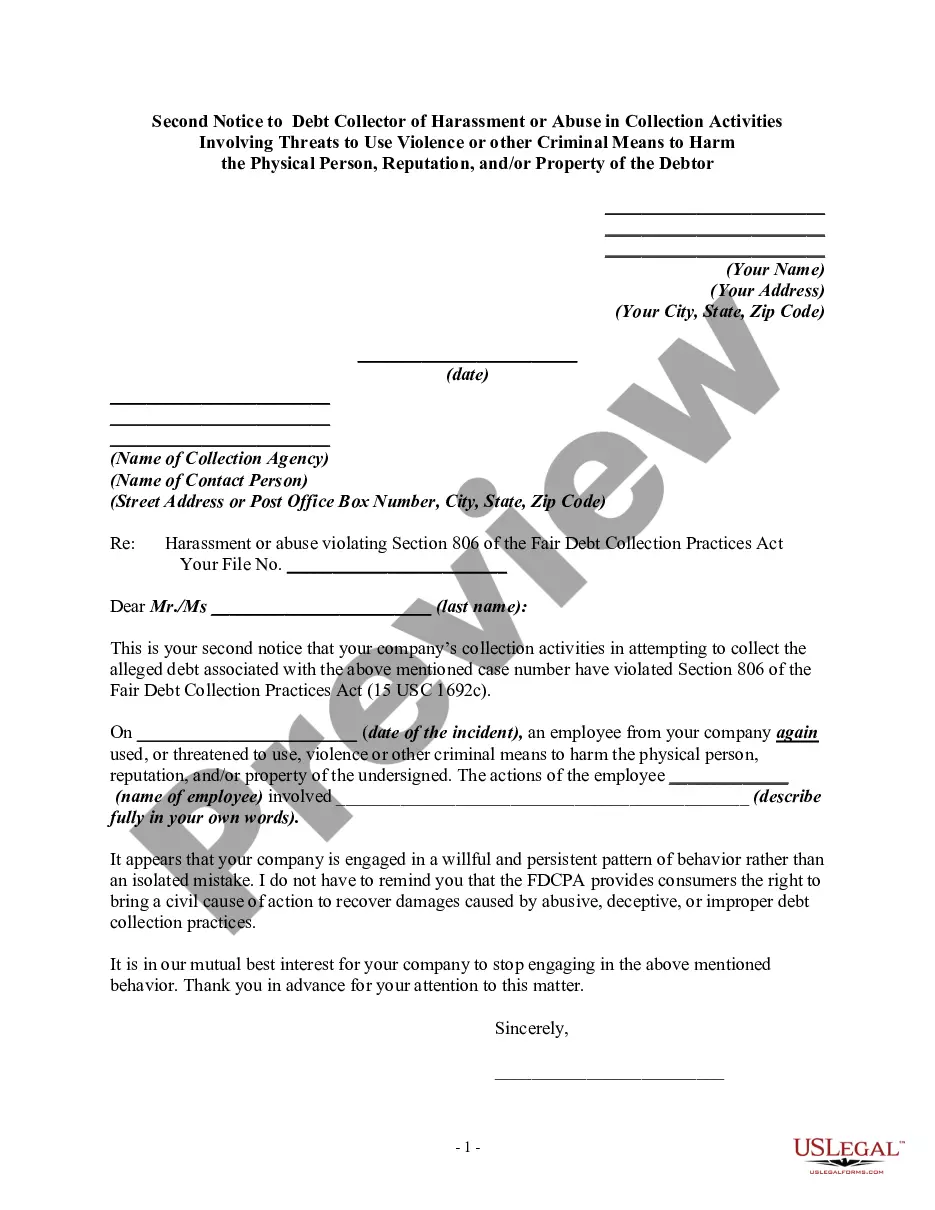
How to fill out Connecticut Notice Of Special Enrollment Rules?
Have you been within a situation in which you need to have documents for both organization or person purposes almost every working day? There are a variety of authorized record layouts available on the net, but getting ones you can depend on is not easy. US Legal Forms provides a large number of kind layouts, like the Connecticut Notice of Special Enrollment Rules, that are created to satisfy state and federal requirements.
When you are currently acquainted with US Legal Forms internet site and possess a free account, merely log in. After that, you can down load the Connecticut Notice of Special Enrollment Rules format.
Unless you come with an profile and want to begin to use US Legal Forms, follow these steps:
- Discover the kind you want and make sure it is to the correct town/region.
- Utilize the Review switch to review the form.
- See the information to actually have selected the right kind.
- In case the kind is not what you`re searching for, utilize the Lookup field to discover the kind that meets your needs and requirements.
- If you find the correct kind, simply click Acquire now.
- Select the pricing strategy you want, complete the desired details to produce your money, and pay money for an order using your PayPal or credit card.
- Pick a hassle-free file format and down load your version.
Find every one of the record layouts you possess bought in the My Forms food list. You can obtain a further version of Connecticut Notice of Special Enrollment Rules whenever, if required. Just click the essential kind to down load or produce the record format.
Use US Legal Forms, probably the most substantial collection of authorized types, to save lots of time as well as prevent blunders. The services provides appropriately created authorized record layouts that you can use for a range of purposes. Generate a free account on US Legal Forms and commence producing your lifestyle a little easier.