Connecticut Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
Are you within a place the place you require files for sometimes company or specific reasons just about every working day? There are plenty of lawful file templates available on the net, but discovering kinds you can trust is not straightforward. US Legal Forms delivers 1000s of form templates, just like the Connecticut Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, which can be written to satisfy state and federal demands.
Should you be previously informed about US Legal Forms website and get a free account, simply log in. Following that, you may download the Connecticut Notice from Employer to Employee Regarding Early Termination of Continuation Coverage format.
If you do not have an accounts and would like to begin to use US Legal Forms, abide by these steps:
- Discover the form you want and make sure it is for the appropriate town/county.
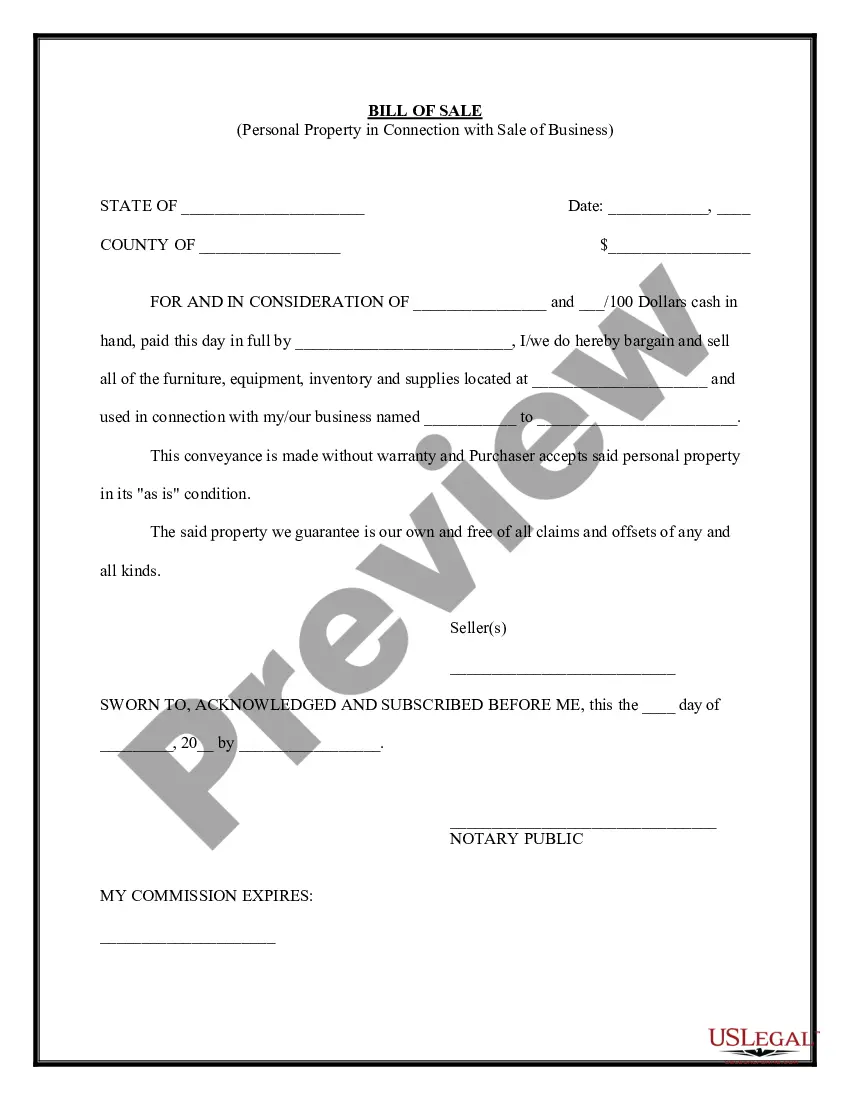
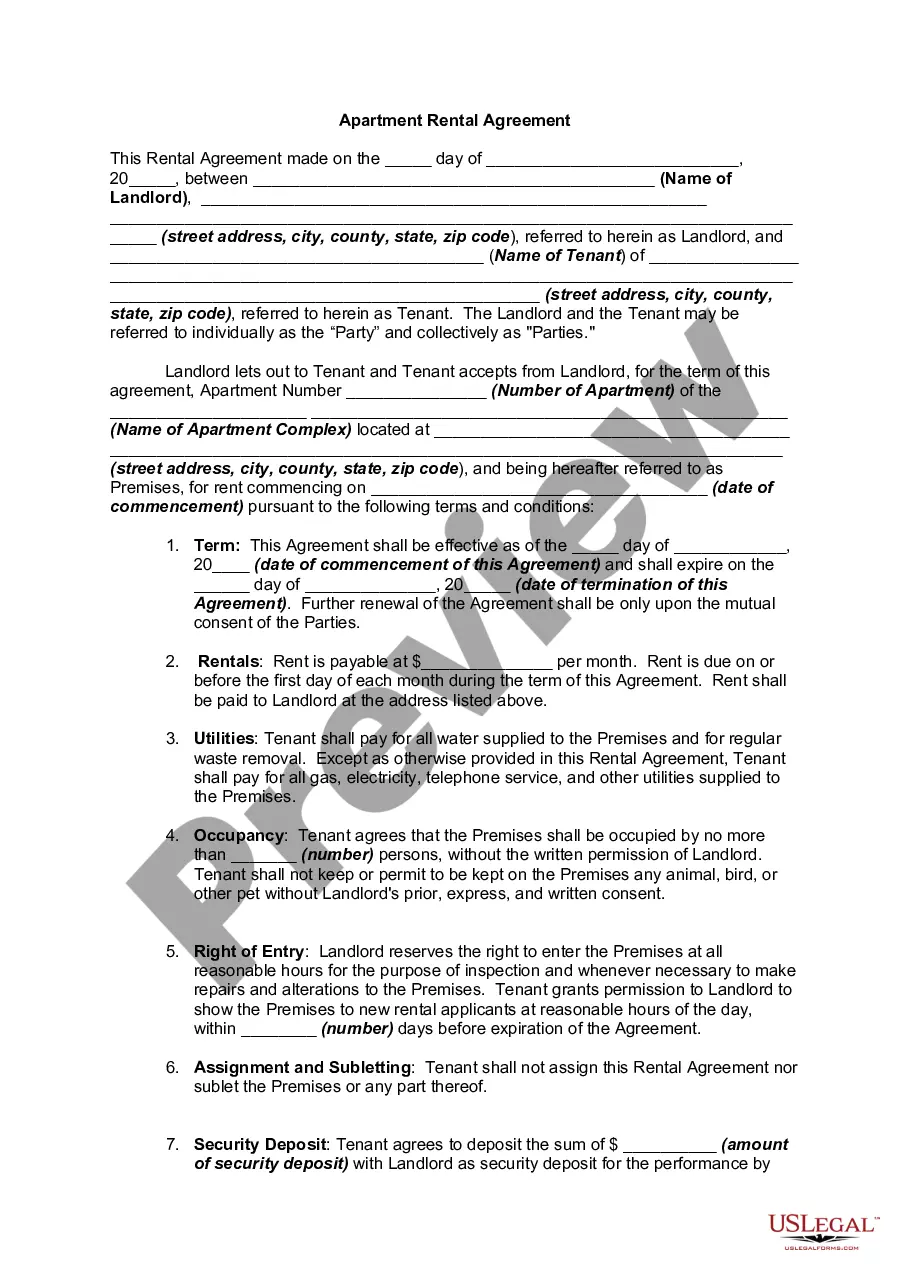
- Take advantage of the Preview switch to check the form.
- Look at the information to actually have selected the right form.
- If the form is not what you are trying to find, make use of the Search discipline to discover the form that meets your requirements and demands.
- Whenever you discover the appropriate form, just click Get now.
- Opt for the pricing strategy you need, fill in the required info to create your money, and buy your order with your PayPal or bank card.
- Choose a handy paper formatting and download your copy.
Discover every one of the file templates you have purchased in the My Forms menu. You can aquire a extra copy of Connecticut Notice from Employer to Employee Regarding Early Termination of Continuation Coverage at any time, if necessary. Just click on the essential form to download or print out the file format.
Use US Legal Forms, by far the most extensive variety of lawful varieties, to conserve some time and steer clear of faults. The assistance delivers professionally produced lawful file templates which can be used for a selection of reasons. Make a free account on US Legal Forms and begin making your life a little easier.
Form popularity
FAQ
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
D&R coverage ends when one of the following occurs: Your employment terminates. You transfer to an employer who does not participate in the D&R Plan. You change jobs with a Participating Employer and start working in an employee group that does not participate in the D&R Plan.
The employer need not give notice if misconduct is the cause for termination. However, the employee, in such circumstances, should have an opportunity to reasonably explain the charge against them prior to termination.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Copayment - A form of medical cost sharing in a health insurance plan that requires an insured person to pay a fixed dollar amount when a medical service is received. The insurer is responsible for the rest of the reimbursement. before a copayment applies.
In this concept, termed means "terminated." This type of termination is also called involuntary termination because the employee has been dismissed against his will.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
After the termination, an employer have to clear all dues of a respective employee. One has to get the notice pay when the termination notice has not been issued. Salary for the working days, compensation of retrenchment and leave encashment.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.