A District of Columbia Health Record Amendment Denial Letter is an official document issued by healthcare providers or organizations in the District of Columbia to inform patients about the rejection or denial of their request to amend their health records. This letter is an essential part of the health record amendment process, ensuring transparency and providing patients with an explanation as to why their requested changes cannot be made. Keywords: District of Columbia, health record amendment, denial letter, healthcare providers, organizations, patients, rejection, transparency, requested changes, explanation. There might be different types of District of Columbia Health Record Amendment Denial Letters, depending on the specific reason for the denial. Some possible variants include: 1. Incomplete Information Denial Letter: This type of denial letter is issued when the patient fails to provide the necessary or complete information required to support their requested amendment. It explains that additional or missing information is needed to proceed with the amendment process. 2. Medical Inaccuracy Denial Letter: This denial letter is given when the healthcare provider finds that the requested changes to the medical records are inaccurate or not supported by sufficient evidence. It may mention specific discrepancies or inconsistencies found in the patient's records. 3. Time Limitation Denial Letter: If the amendment request falls outside the acceptable timeframe for modifications, this denial letter is issued. It informs patients that their request cannot be fulfilled due to the expiration of the designated time period for making changes to health records. 4. Legal Restriction Denial Letter: When certain legal restrictions prevent the healthcare provider from amending the patient's health records as requested, this denial letter is provided. It may outline the specific legal regulations or requirements that prohibit the desired modifications. 5. Insufficient Justification Denial Letter: This type of denial letter is given when the patient's reasons or justifications for amending their health records are deemed insufficient or unsupported. It explains the need for credible evidence or valid reasons to support any modifications to the records. By categorizing these types of denial letters, healthcare providers ensure clear and specific communication with patients regarding the inability to accommodate their requested amendments to the health records.
District of Columbia Health Record Amendment Denial Letter
Description
How to fill out District Of Columbia Health Record Amendment Denial Letter?
Are you currently inside a situation the place you require files for sometimes company or individual reasons nearly every time? There are tons of legal file layouts available on the Internet, but getting versions you can rely on is not easy. US Legal Forms provides 1000s of kind layouts, like the District of Columbia Health Record Amendment Denial Letter, which are composed in order to meet federal and state demands.
Should you be already informed about US Legal Forms web site and have an account, basically log in. Afterward, you can acquire the District of Columbia Health Record Amendment Denial Letter web template.
If you do not provide an account and wish to begin using US Legal Forms, abide by these steps:
- Get the kind you require and make sure it is for that right town/state.
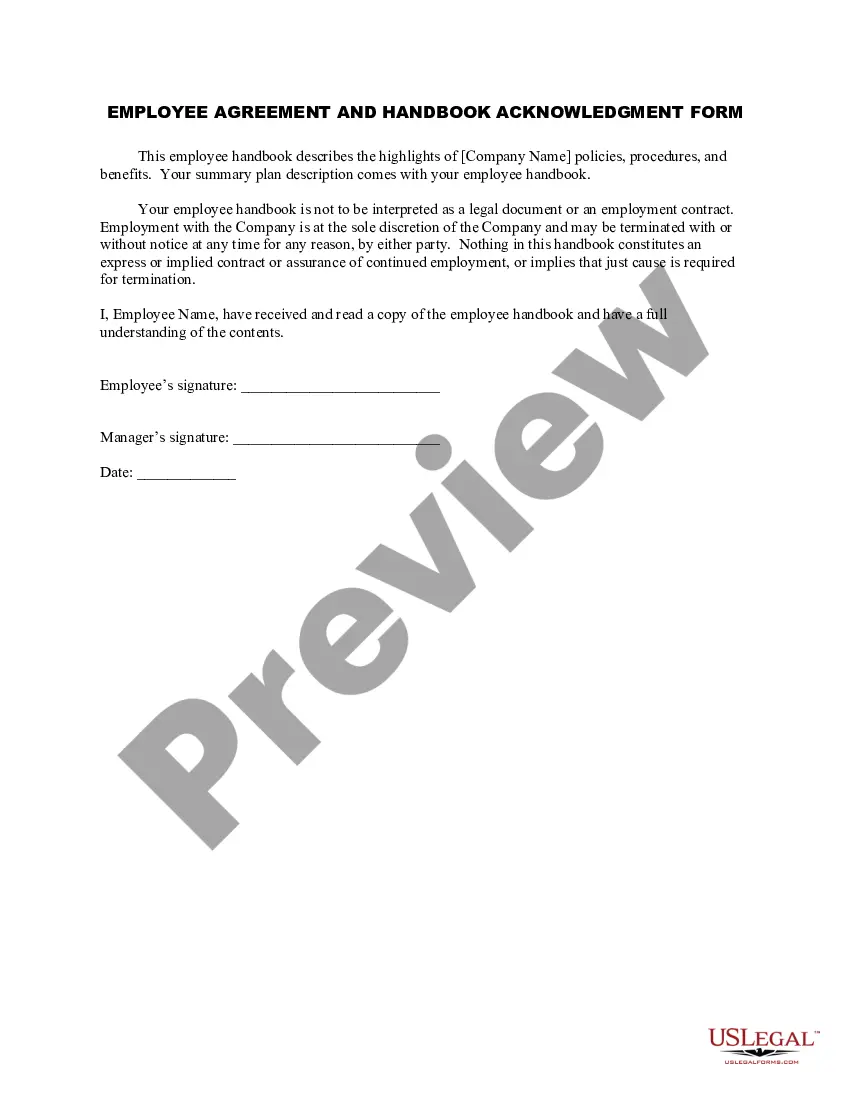
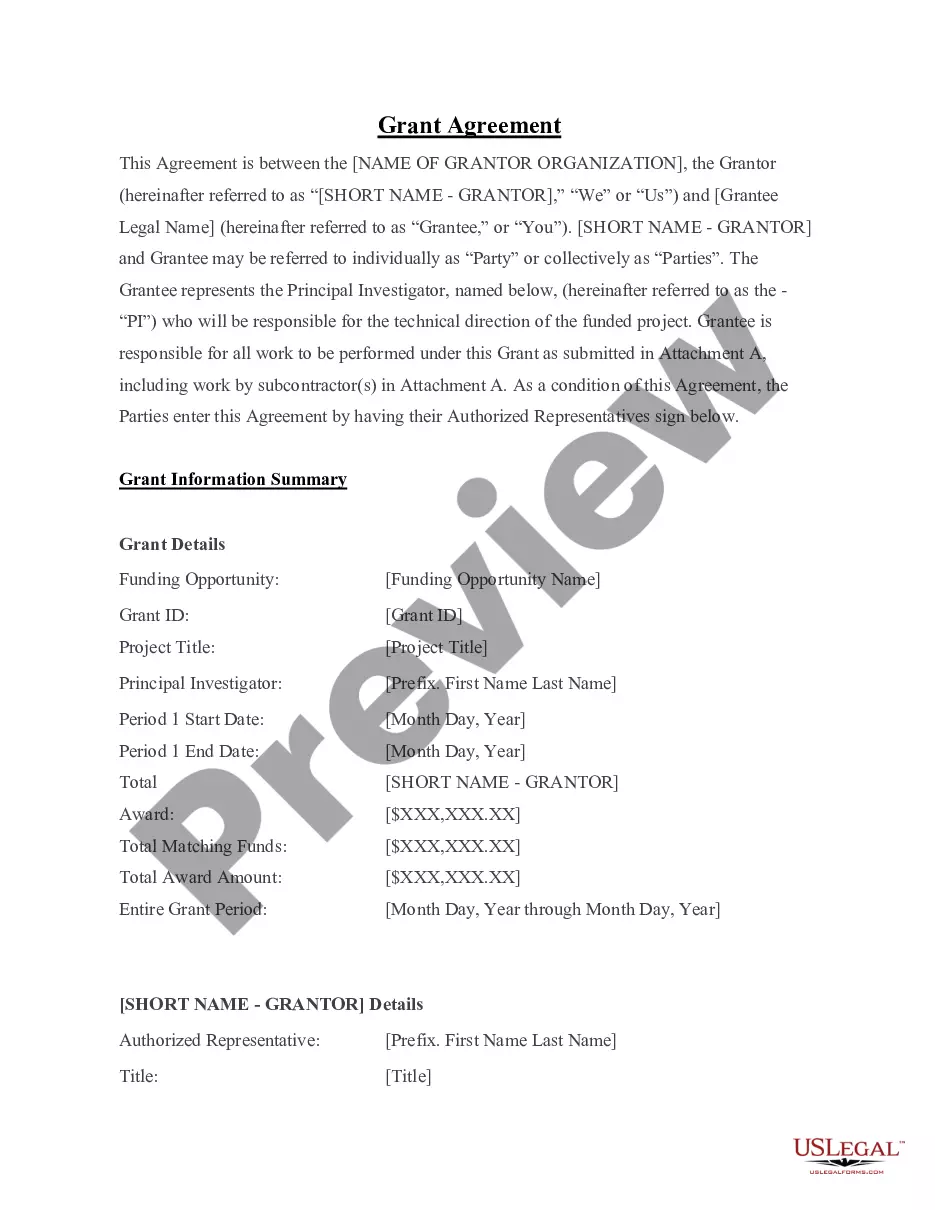
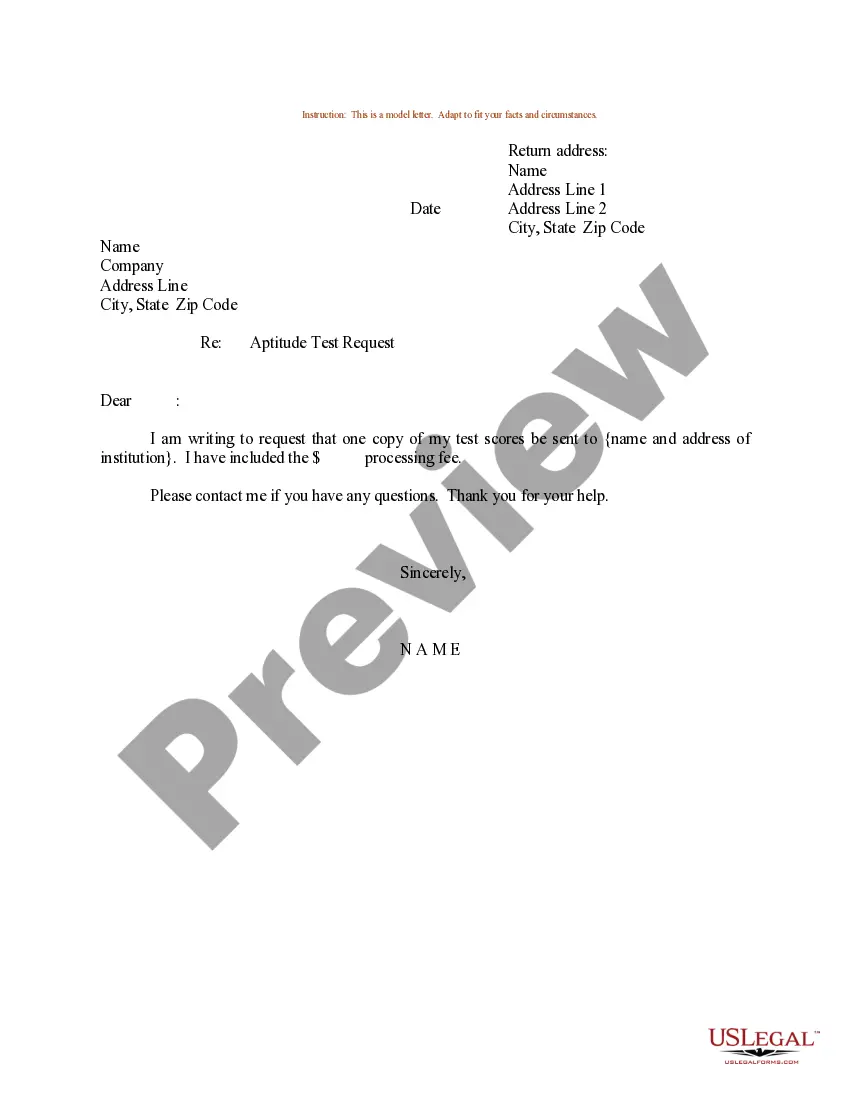
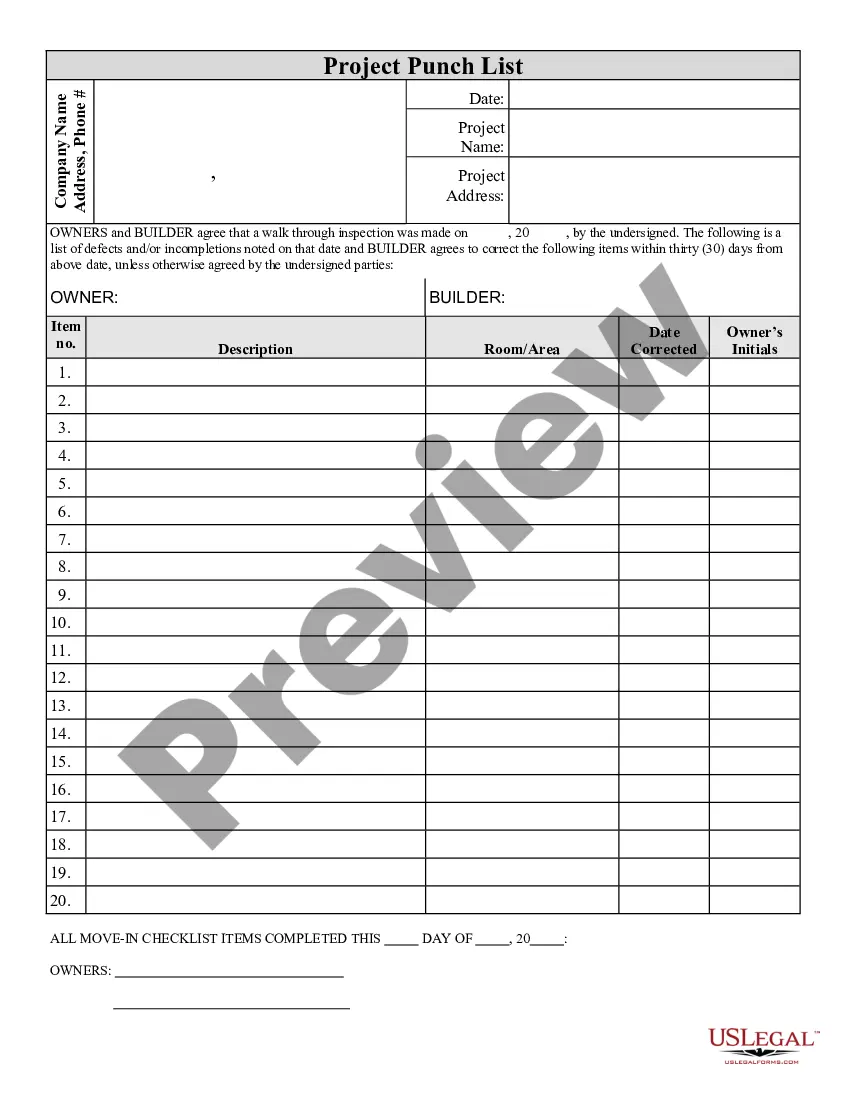
- Make use of the Review button to analyze the form.
- Browse the explanation to ensure that you have chosen the correct kind.
- If the kind is not what you are searching for, make use of the Lookup discipline to discover the kind that meets your needs and demands.
- When you discover the right kind, click on Purchase now.
- Opt for the pricing program you need, fill out the specified details to produce your money, and pay money for the order using your PayPal or charge card.
- Pick a convenient data file format and acquire your version.
Discover every one of the file layouts you may have purchased in the My Forms food selection. You can aquire a additional version of District of Columbia Health Record Amendment Denial Letter at any time, if needed. Just select the necessary kind to acquire or print the file web template.
Use US Legal Forms, one of the most substantial selection of legal types, to conserve some time and stay away from errors. The assistance provides skillfully produced legal file layouts that can be used for an array of reasons. Generate an account on US Legal Forms and commence producing your lifestyle a little easier.