The District of Columbia Election Form for Continuation of Benefits — COBRA is a crucial document that provides employees with the necessary information and options regarding their continuation of benefits under the Consolidated Omnibus Budget Reconciliation Act (COBRA). COBRA ensures that individuals, who would otherwise lose their health insurance coverage due to qualifying events such as job loss, reduction in work hours, or certain life events, have the opportunity to continue receiving healthcare benefits. This election form serves as a means for eligible individuals in the District of Columbia to exercise their right to elect continued coverage within the designated time frame. It allows employees to make informed decisions about their healthcare options and ensures that they receive essential medical services during times of transition or uncertain circumstances. The District of Columbia Election Form for Continuation of Benefits — COBRA typically includes the following relevant keywords: 1. District of Columbia: Referring to the specific jurisdiction within which the COBRA election form is applicable, indicating that it is specific to residents of the District of Columbia. 2. Election Form: The document itself, which requires employees to select their desired options for continuation of healthcare coverage under COBRA. 3. Continuation of Benefits: Emphasizing the purpose of the form, which is to enable individuals the opportunity to maintain their health insurance benefits despite qualifying events. 4. COBRA: An abbreviation for the Consolidated Omnibus Budget Reconciliation Act, a federal law that grants individuals the right to continue receiving health insurance coverage for a defined period after job loss or other qualifying events. It's important to note that there may not be different types of District of Columbia Election Form for Continuation of Benefits — COBRA per se, as the content and structure of the form are typically standardized by federal regulations. However, various templates and versions of the election form may exist, with slight variations in formatting or additional instructions depending on the issuing entity.
District of Columbia Election Form for Continuation of Benefits - COBRA
Description
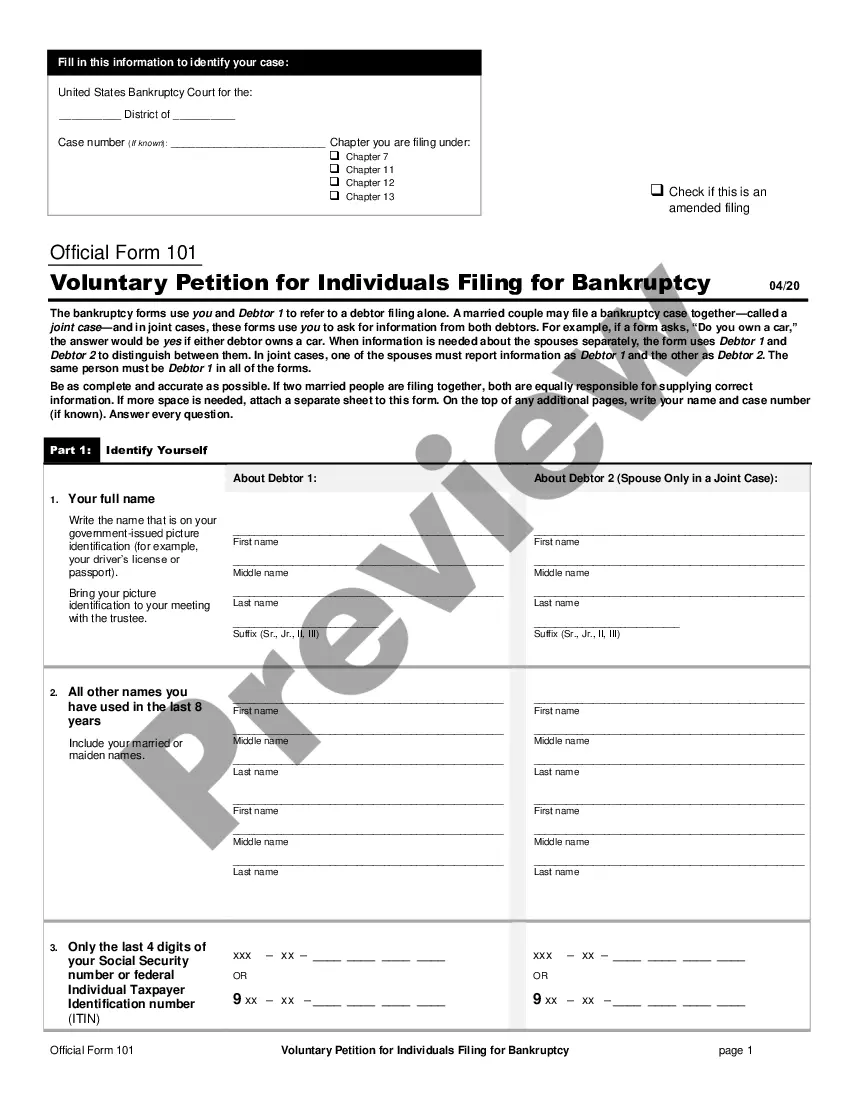
How to fill out District Of Columbia Election Form For Continuation Of Benefits - COBRA?
If you have to complete, obtain, or produce authorized document web templates, use US Legal Forms, the biggest selection of authorized types, that can be found on-line. Use the site`s simple and convenient search to obtain the documents you want. Different web templates for organization and individual uses are sorted by groups and suggests, or keywords. Use US Legal Forms to obtain the District of Columbia Election Form for Continuation of Benefits - COBRA within a handful of mouse clicks.
Should you be presently a US Legal Forms consumer, log in to your account and click on the Down load option to have the District of Columbia Election Form for Continuation of Benefits - COBRA. You can also accessibility types you earlier acquired from the My Forms tab of the account.
Should you use US Legal Forms initially, follow the instructions below:
- Step 1. Be sure you have chosen the shape for that right metropolis/country.
- Step 2. Utilize the Preview method to examine the form`s content material. Never neglect to read through the description.
- Step 3. Should you be not happy with all the develop, take advantage of the Search discipline near the top of the display to get other models of your authorized develop design.
- Step 4. After you have identified the shape you want, select the Purchase now option. Opt for the pricing prepare you prefer and add your accreditations to sign up on an account.
- Step 5. Procedure the deal. You can use your Мisa or Ьastercard or PayPal account to finish the deal.
- Step 6. Find the file format of your authorized develop and obtain it on the product.
- Step 7. Full, edit and produce or indication the District of Columbia Election Form for Continuation of Benefits - COBRA.
Every authorized document design you get is the one you have forever. You may have acces to each develop you acquired in your acccount. Go through the My Forms area and pick a develop to produce or obtain once again.
Contend and obtain, and produce the District of Columbia Election Form for Continuation of Benefits - COBRA with US Legal Forms. There are millions of specialist and express-specific types you can utilize for your organization or individual requirements.
Form popularity
FAQ
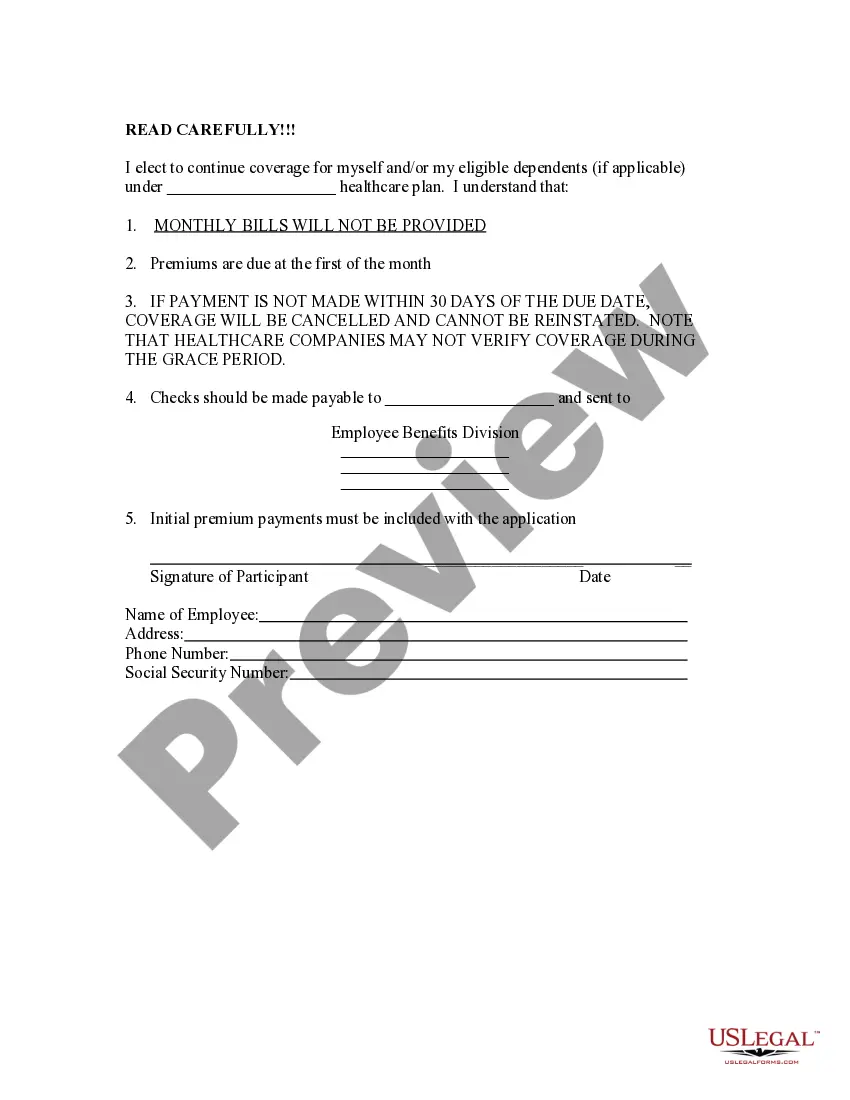
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
How COBRA Works In Delaware. The Federal COBRA Law requires businesses with 20 or more workers to provide the option to elect the same group health coverage to workers and their families if that insurance would end. Exempt from this rule are government employers, churches and tax-exempt organizations.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
The D.C. mini-COBRA law provides for 3 months of continuation coverage, except in the case of terminations for gross misconduct. The employer is required to provide notice to the employee within 15 days after the date that coverage would otherwise terminate.
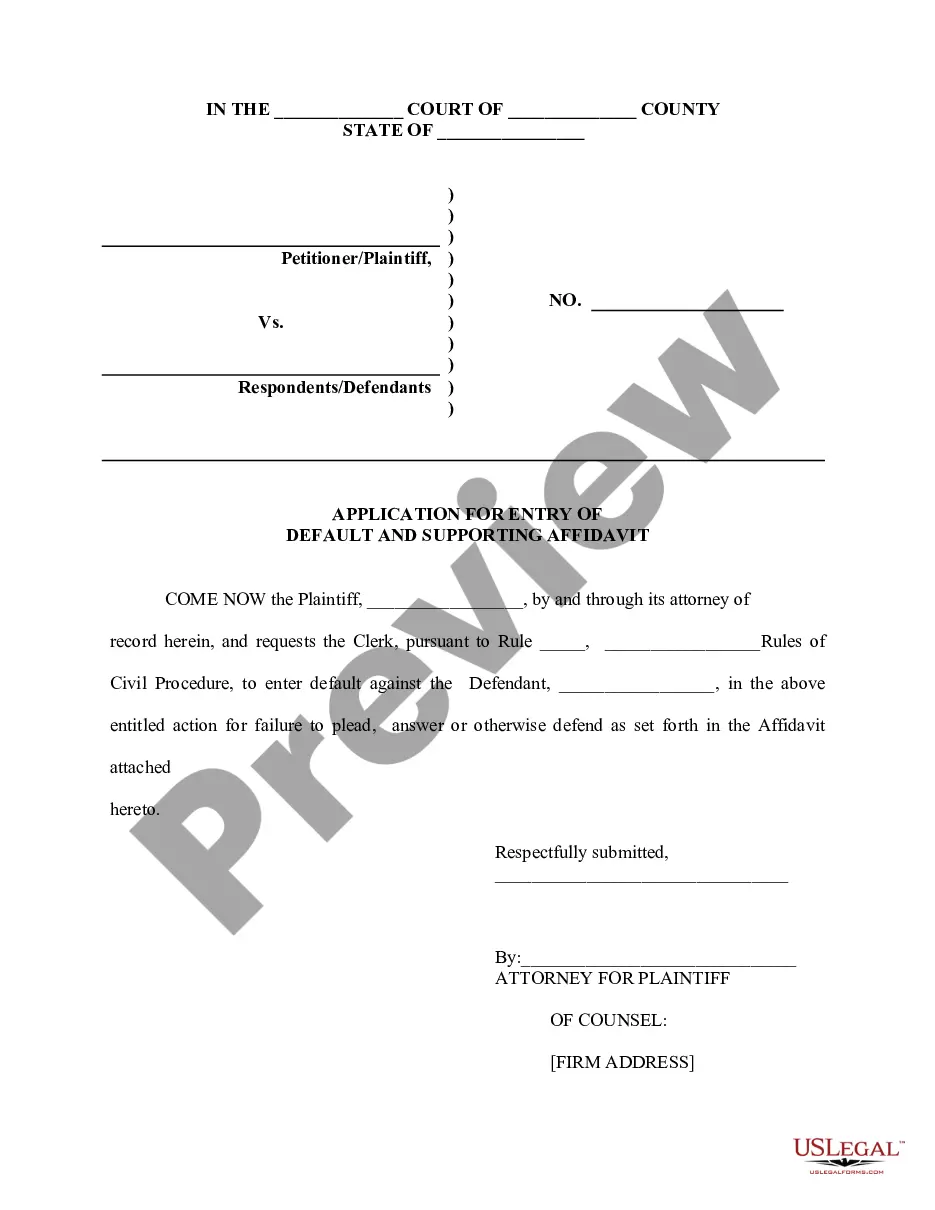
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
How to Administer Cal-COBRANotifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
You can reach Covered California at (800) 300-1506 or online at . You can apply for individual coverage directly through some health plans off the exchange.
Covered Employers Under federal COBRA, employers with 20 or more employees are usually required to offer COBRA coverage. COBRA applies to plans maintained by private-sector employers (including self-insured plans) and those sponsored by most state and local governments.