Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports are services that provide an independent assessment of health insurance claims disputes. This helps to ensure that health insurance companies comply with insurance law and regulations, and that policyholders receive fair and equitable decisions when faced with a claim denial. The Delaware Department of Insurance oversees the Delaware External Review, Arbitration & Independent Review of Health Insurance Claims Reports process. The Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports process can be broken down into three different types of reviews: Internal Review, Arbitration and Independent Review. Internal Review: Internal Review is a review of a denied health insurance claim by the health insurance company. The health insurance company may review the claim and overturn the decision to deny based on new evidence or information. Arbitration: Arbitration is an alternative dispute resolution process that is used to resolve health insurance claims disputes. An independent arbitrator will review the dispute and make a decision. Independent Review: Independent Review is a review of a denied health insurance claim by an independent third party. This third party is usually a panel of experts that review the claim and make a decision. These three services provide an independent review of health insurance claims disputes, helping to ensure that policyholders receive fair and equitable decisions.
Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports
Description
How to fill out Delaware Internal Review, Arbitration & Independent Review Of Health Insurance Claims Reports?
Engaging with official documentation necessitates focus, precision, and utilizing well-prepared templates. US Legal Forms has been assisting individuals nationwide in achieving this for 25 years, so when you select your Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports template from our platform, you can trust it complies with federal and state guidelines.
Utilizing our platform is straightforward and efficient. To access the necessary documentation, all you require is an account with a valid subscription. Here’s a quick guide for you to obtain your Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports in just a few minutes.
All documents are designed for multiple uses, like the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports you see on this page. If you require them in the future, you can complete them without additional payment - just access the My documents section in your profile and finalize your document whenever needed. Try US Legal Forms and complete your business and personal paperwork rapidly and in full legal compliance!
- Ensure you carefully examine the form content and its alignment with general and legal standards by previewing it or reviewing its description.
- Look for an alternative official template if the one you opened does not fit your circumstances or state regulations (the option for that is located at the top page corner).
- Log in to your account and save the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports in your desired format. If it’s your first time using our service, click Buy now to continue.
- Create an account, select your subscription plan, and make a payment using your credit card or PayPal account.
- Choose the format in which you wish to save your document and click Download. You can print the blank version or upload it to a professional PDF editor to submit it electronically.
Form popularity
FAQ
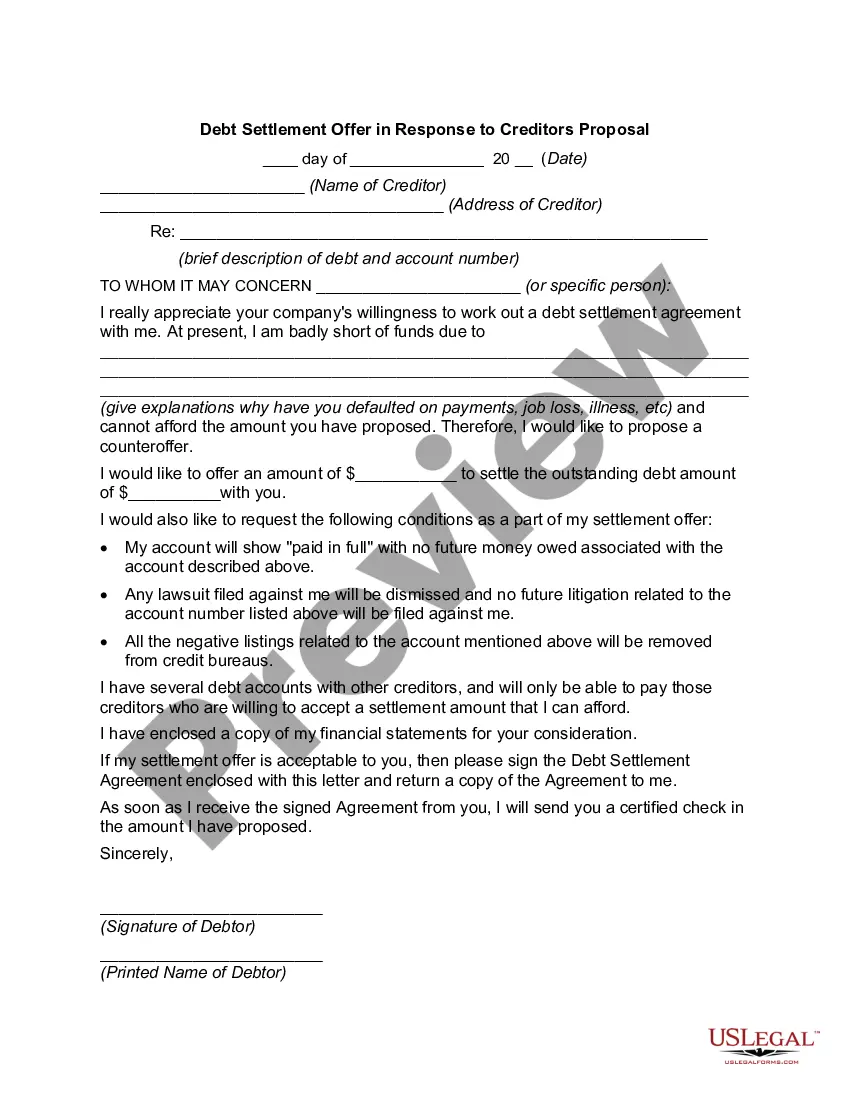
To write a grievance appeal letter to an insurance company, start by addressing it to the appropriate department and including all necessary personal details. Clearly articulate your points regarding why the grievance should be reconsidered, and attach any pertinent documents that support your claim. Referencing Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports can demonstrate your knowledge and encourage a prompt reconsideration of your appeal.
In a grievance appeal letter, include your claim number and prior correspondence related to your grievance. Clearly state why you believe the decision was incorrect, and provide additional evidence or supporting documents that reinforce your case. Mentioning Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports can strengthen your argument by indicating your awareness of the resolution process available.
When writing a grievance letter to an insurance company, begin with your contact information and policy details. Clearly explain the issue you experienced and provide specific examples to illustrate your concerns. It is also helpful to mention Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports, as this demonstrates your understanding of the necessary steps for addressing your grievance.
To write a good appeal letter to an insurance company, start by clearly stating your policy number and the specific claim in question. Be sure to outline the reasons for your appeal, referencing any relevant documentation that supports your case. Additionally, mention Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports to highlight your knowledge of the process and your commitment to a fair resolution.
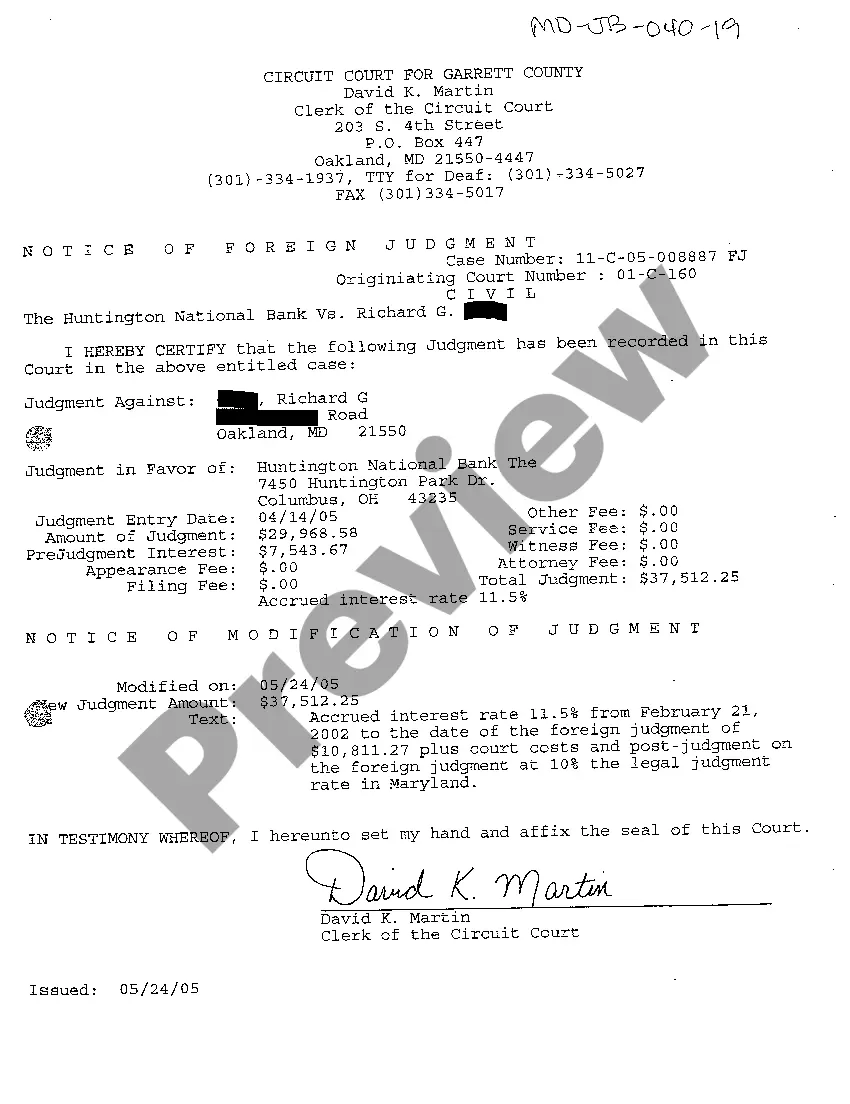
An insurance external review is an independent assessment of a health insurance claim denial after you've completed your internal appeal. It provides a fresh perspective from an unbiased professional who evaluates your case according to specific criteria. This review is part of the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports, ensuring your rights are protected. Utilizing tools from platforms like uslegalforms can simplify this process and enhance your chances of success.
An internal appeal is a process that allows you to challenge a health insurance claim denial. In this process, your insurance company reviews the claim again based on the additional information you provide. This procedure is a vital step in the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports. Engaging in an internal appeal can lead to favorable outcomes, saving you time and resources.
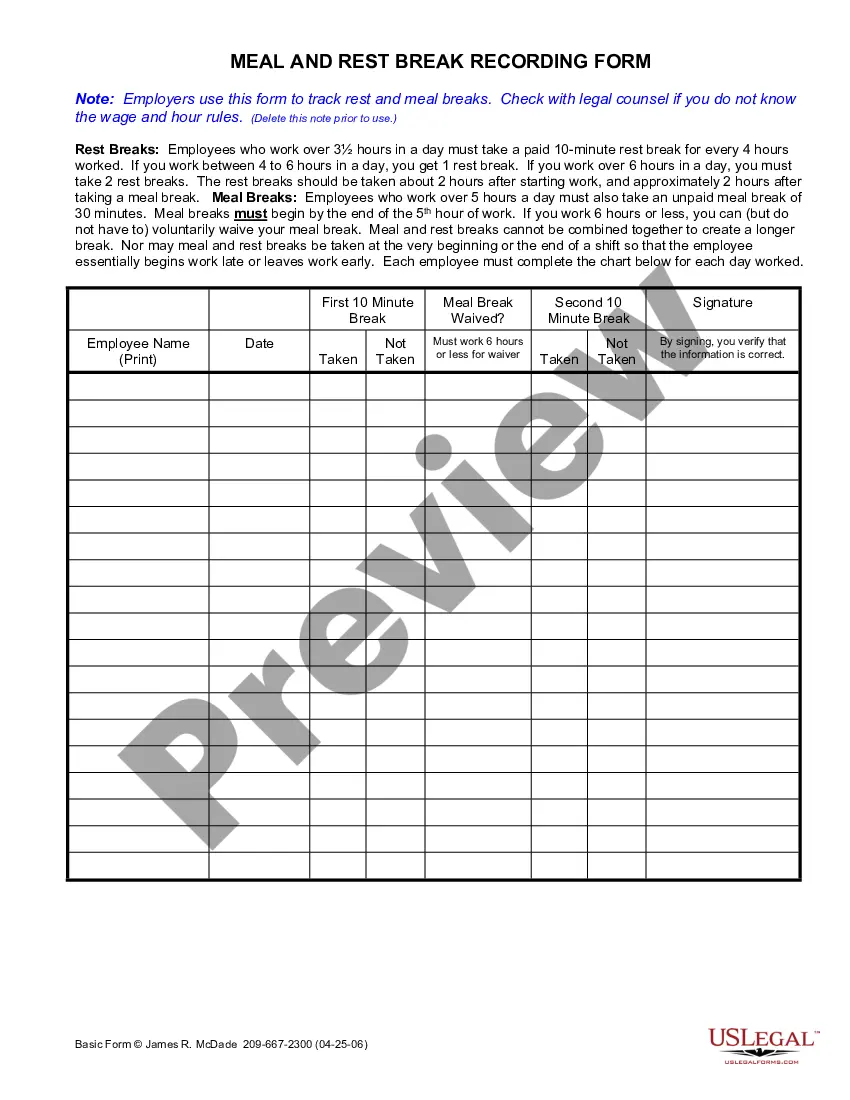
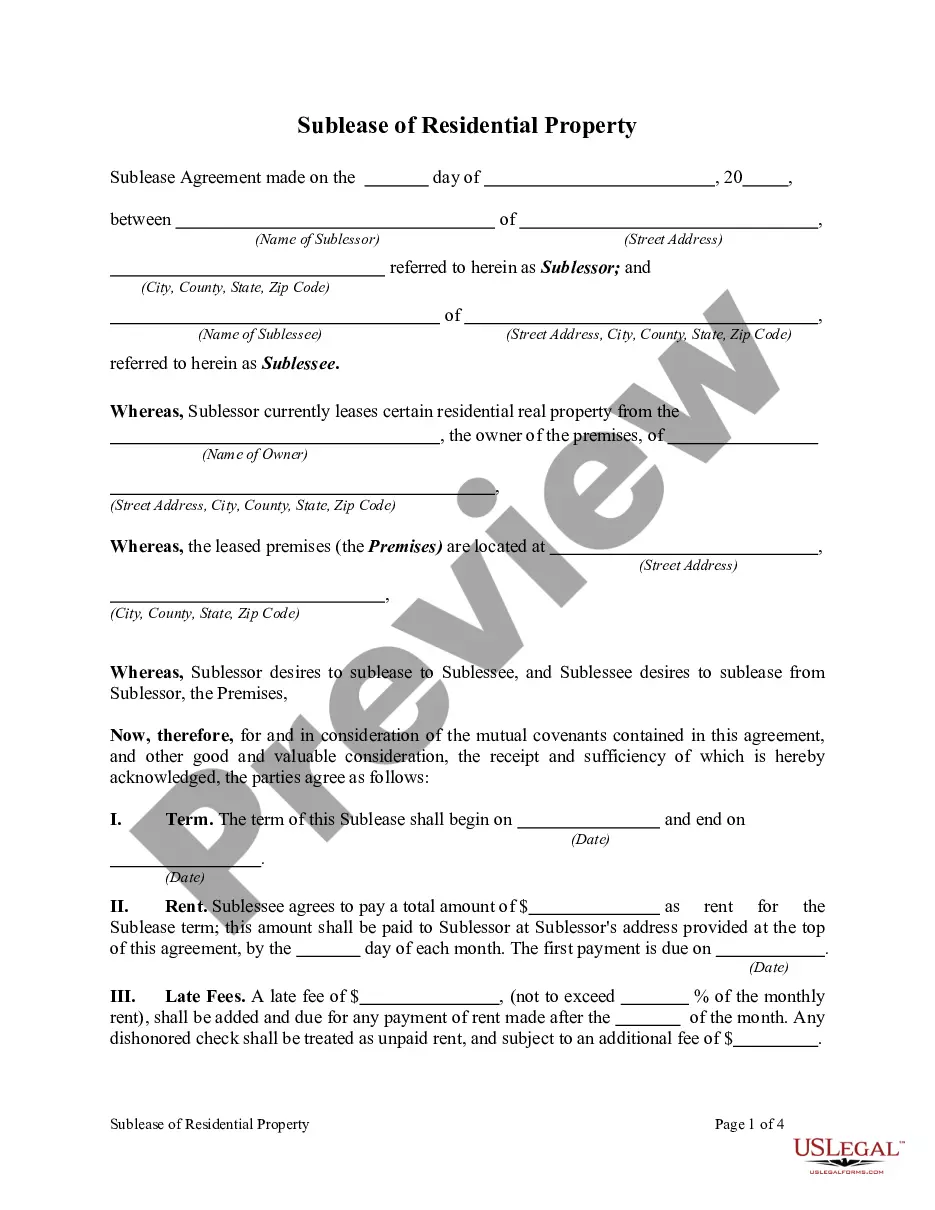
To fill out a health insurance claim form effectively, start by carefully reading the instructions provided by your insurance company. Input your information clearly, including your policy number and details of the medical services. Be thorough to prevent any rejection of claims based on incomplete information. Leveraging guidance from the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports will empower you throughout this essential task.
Filling out a health insurance claim form requires careful attention to detail. Begin by entering your personal information, followed by the specifics of your health care provider and the services received. Make sure to include relevant diagnosis codes and itemized billing if required. Utilizing insights from the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports can help you complete this process accurately and efficiently.
Submitting a claim in care health insurance involves gathering all necessary documentation, including the claim form and receipts for medical expenses. Ensure you fill out the form accurately to avoid delays. Once you have completed the paperwork, submit it to your insurance provider through their preferred method, which might include online submission or mail. Staying updated on the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports can enhance your understanding of your obligations and rights.
To file a claim with your health insurance company, you need to complete the claim form provided by your insurer. This form requires details about the medical services received and the costs incurred. After filling out the form, submit it along with any required documents, such as receipts or invoices. Utilizing resources like the Delaware Internal Review, Arbitration & Independent Review of Health Insurance Claims Reports can keep you informed about your rights throughout this process.