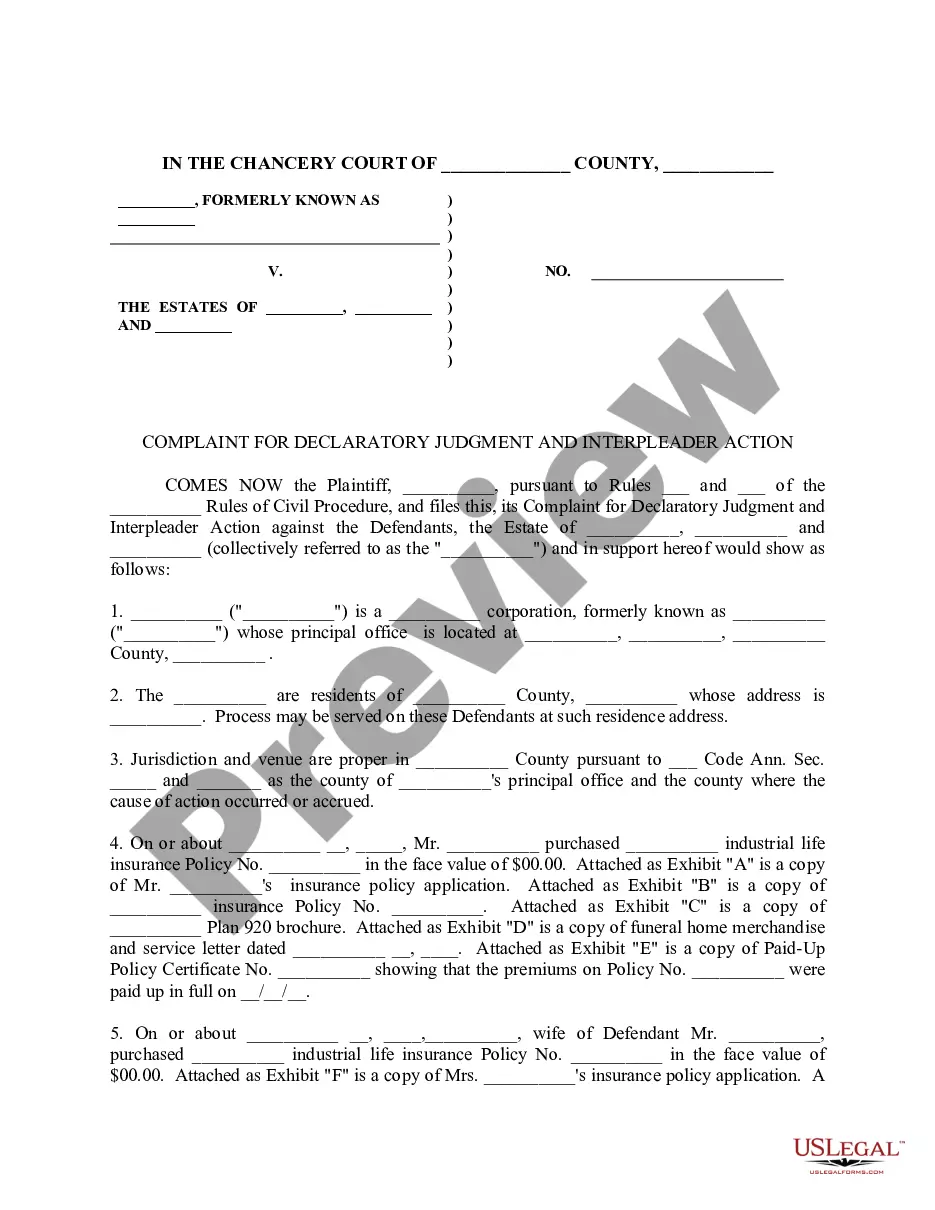
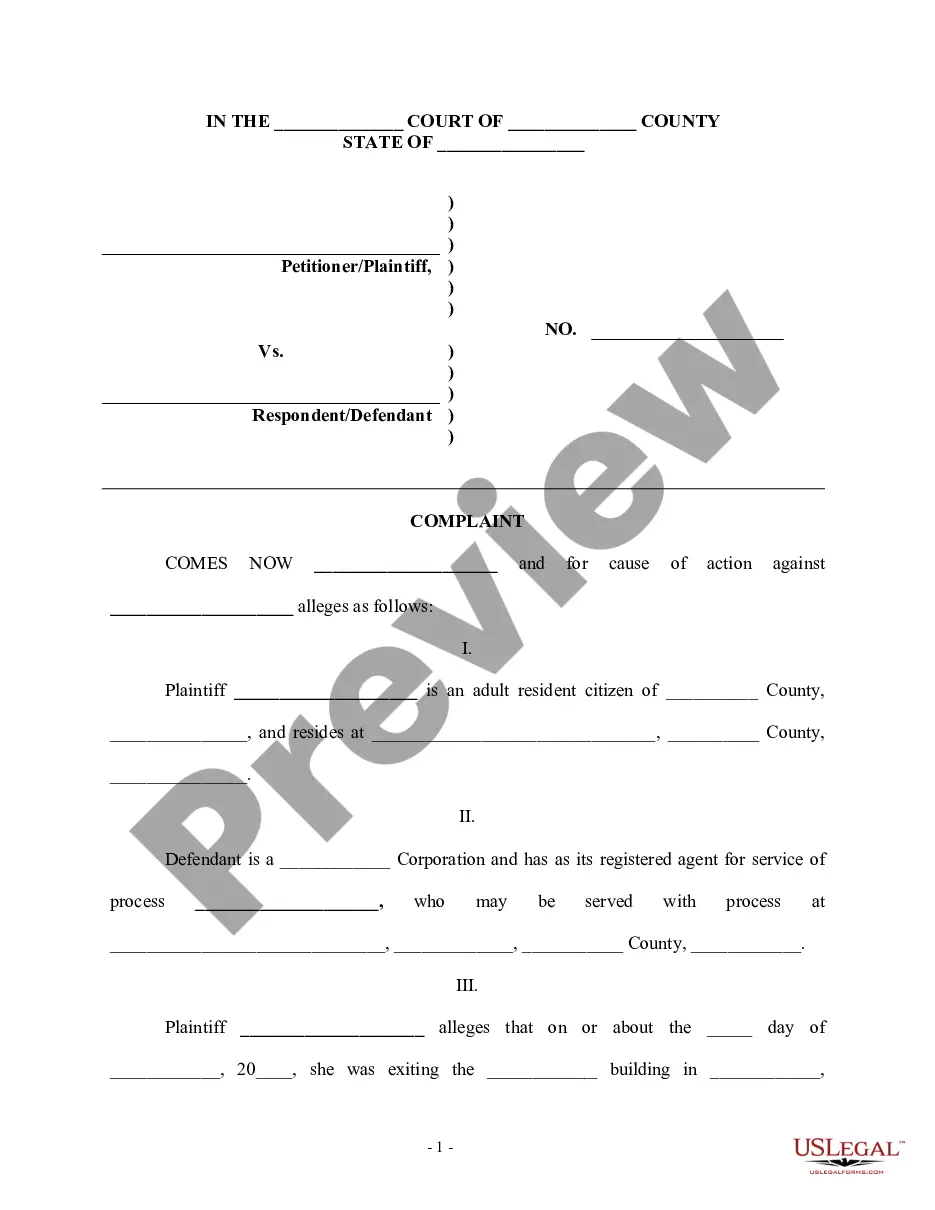
This form is a Complaint For Declaratory Judgment To Determine ERISA Coverage. Adapt to your specific circumstances. Don't reinvent the wheel, save time and money.
Delaware Complaint For Declaratory Judgment To Determine ERISA Coverage
Description
How to fill out Complaint For Declaratory Judgment To Determine ERISA Coverage?
You may spend countless hours online searching for the legal document template that fulfills the state and federal criteria you require. US Legal Forms provides a vast array of legal forms that can be reviewed by experts.
You have the option to download or print the Delaware Complaint For Declaratory Judgment To Determine ERISA Coverage from the service. If you possess a US Legal Forms account, you can Log In and click on the Acquire button. Subsequently, you can fill out, modify, print, or sign the Delaware Complaint For Declaratory Judgment To Determine ERISA Coverage.
Every legal document template you obtain is yours indefinitely. To retrieve an additional copy of the downloaded form, navigate to the My documents section and click on the respective button.
Select the format of the document and download it to your device. Make alterations to the document if necessary. You can fill out, revise, sign, and print the Delaware Complaint For Declaratory Judgment To Determine ERISA Coverage. Acquire and print numerous document templates using the US Legal Forms website, which offers the most extensive collection of legal forms. Utilize professional and state-specific templates to address your business or personal needs.
- If you're accessing the US Legal Forms website for the first time, follow the straightforward instructions below.
- Firstly, ensure that you have selected the appropriate document template for your location/region of interest. Review the form outline to confirm that you have chosen the correct one.
- If available, use the Review button to browse through the document template as well.
- To find another version of the form, use the Lookup field to locate the template that aligns with your needs and specifications.
- Once you have identified the template you desire, click on Acquire now to continue.
- Select the pricing plan you prefer, provide your information, and register for an account on US Legal Forms.
- Complete the transaction. You can use your credit card or PayPal account to pay for the legal document.
Form popularity
FAQ
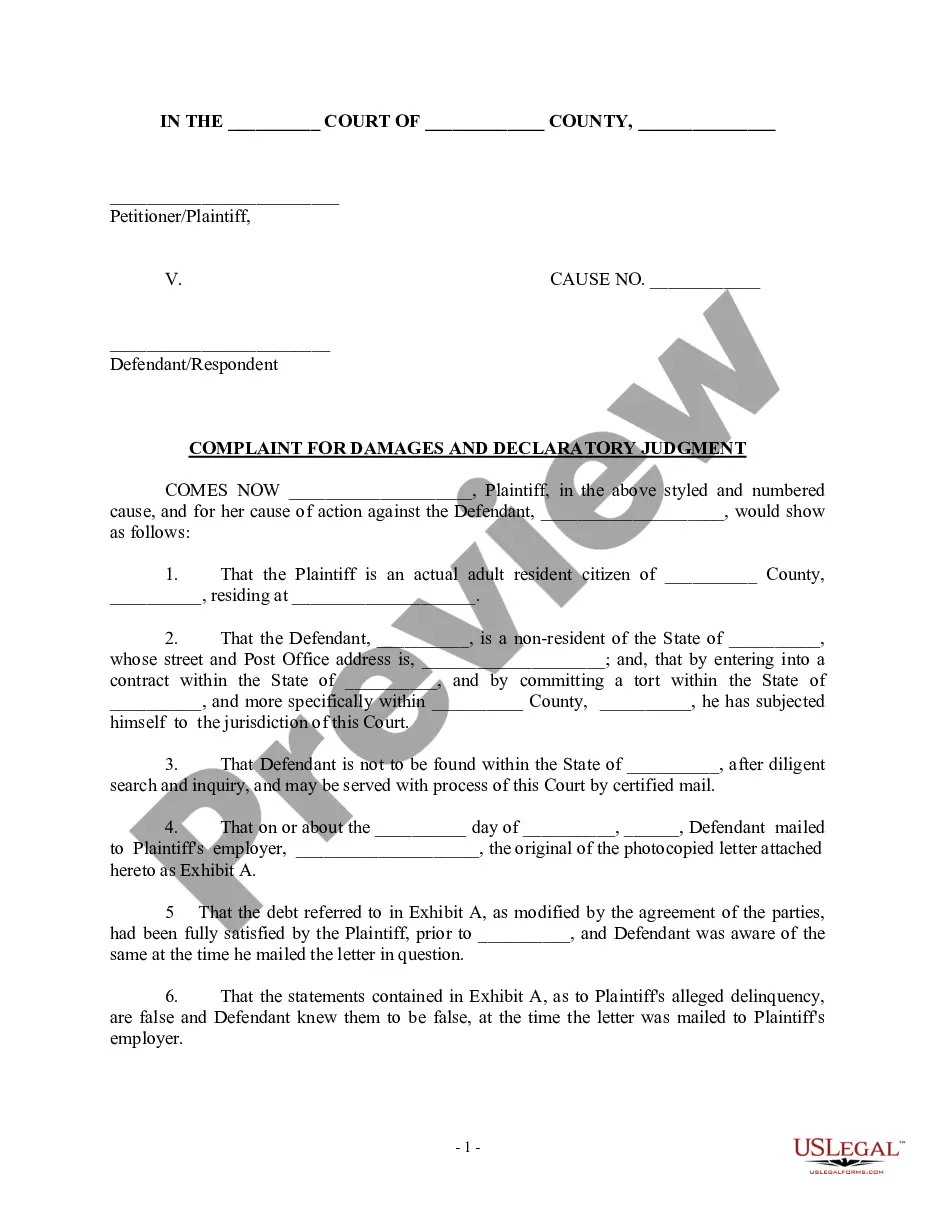
To prove an insurance company acted in bad faith, you must demonstrate that it failed to uphold its obligations under the policy. This typically involves showing that the insurer denied a legitimate claim without a reasonable basis or delayed payment unreasonably. Documenting communications and decisions can strengthen your case. If you are facing issues related to ERISA coverage, a Delaware Complaint For Declaratory Judgment To Determine ERISA Coverage can help clarify your rights and obligations.
A declaratory judgment action may be inappropriate where it is filed to beat the natural plaintiff to the courthouse. This tactic may be intended to deprive the other party of its natural position as plaintiff. Or, it may be intended to deprive the natural plaintiff of its choice of forum.
A declaratory judgment is a binding judgment from a court defining the legal relationship between parties and their rights in a matter before the court. When there is uncertainty as to the legal obligations or rights between two parties, a declaratory judgment offers an immediate means to resolve this uncertainty.
Declaratory relief refers to a court's declaratory judgment stating the rights of parties without ordering any specific action or listing awards for damages.
Declaratory judgment and injunction Order (Injunctive Relief) are different in nature but same in purpose. The effects and outcomes may be varying ing to situation and requirements. The judgment doesn't award the remedies but the injunctive relief awards the remedies on the temporary or permanent base.
The Delaware Supreme Court defined bad faith as ?where the fiduciary intentionally acts with a purpose other than that of advancing the best interests of the corporation, where the fiduciary acts with the intent to violate applicable law, or where the fiduciary intentionally fails to act in the face of a known duty to ...
§ 6501. Power of courts; form and effect of declaration. Except where the Constitution of this State provides otherwise, courts of record within their respective jurisdictions shall have power to declare rights, status and other legal relations whether or not further relief is or could be claimed.