Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508
Description
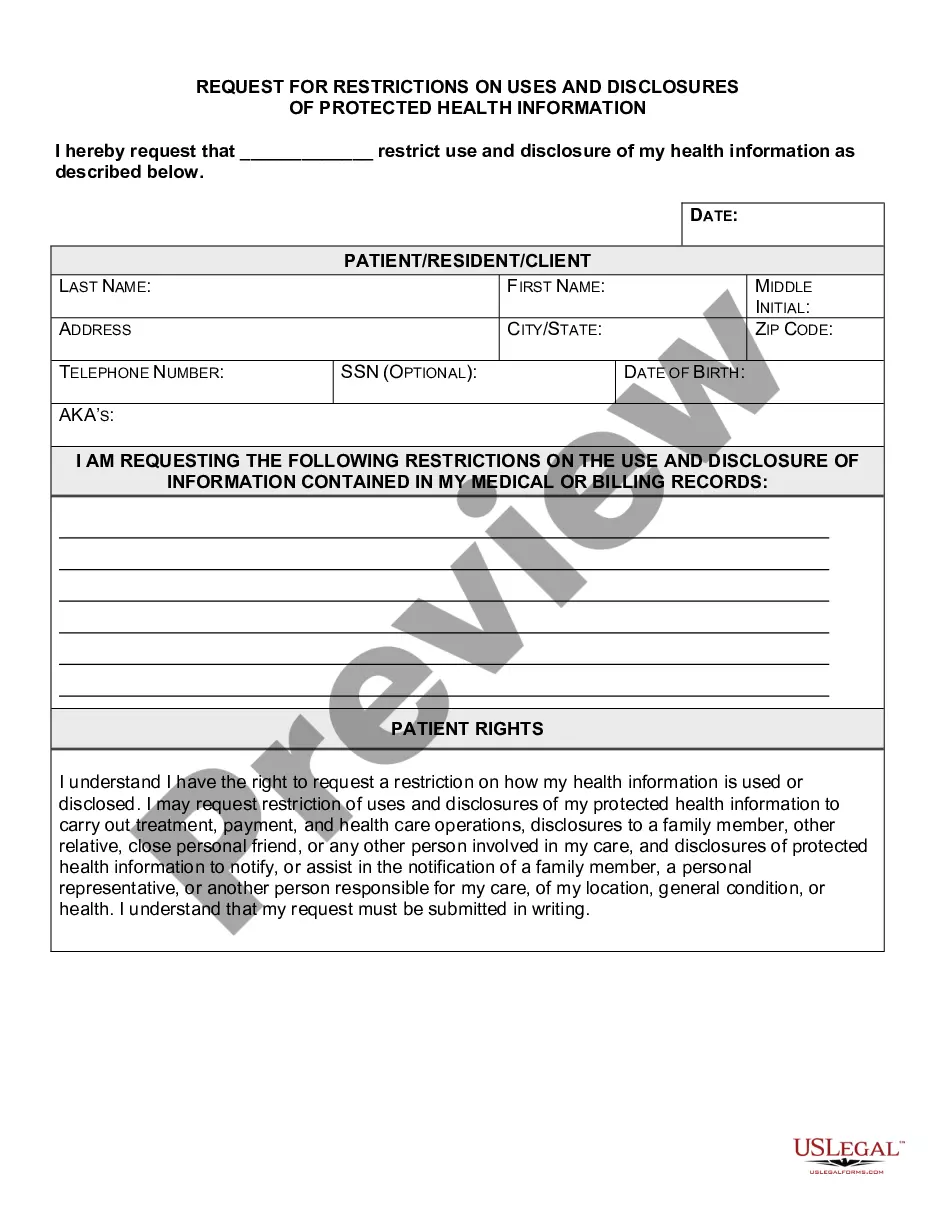
How to fill out Authorization For Use And Disclosure Of Protected Health Information Under HIPAA RULE 164.508?
Selecting the optimal lawful document template can be challenging.
Of course, there are numerous templates accessible online, but how do you find the legal version you require.
Utilize the US Legal Forms website. This service provides a vast array of templates, including the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, suitable for both business and personal purposes.
First, ensure you have selected the correct form for your location. You can view the form using the Review button and read the form description to confirm it is suitable for your needs.
- All of the forms are reviewed by professionals and comply with federal and state regulations.
- If you already have an account, sign in and click the Obtain button to access the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508.
- Use your account to browse the legal forms you have previously ordered.
- Visit the My documents section of your account to download another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple instructions you can follow.
Form popularity
FAQ
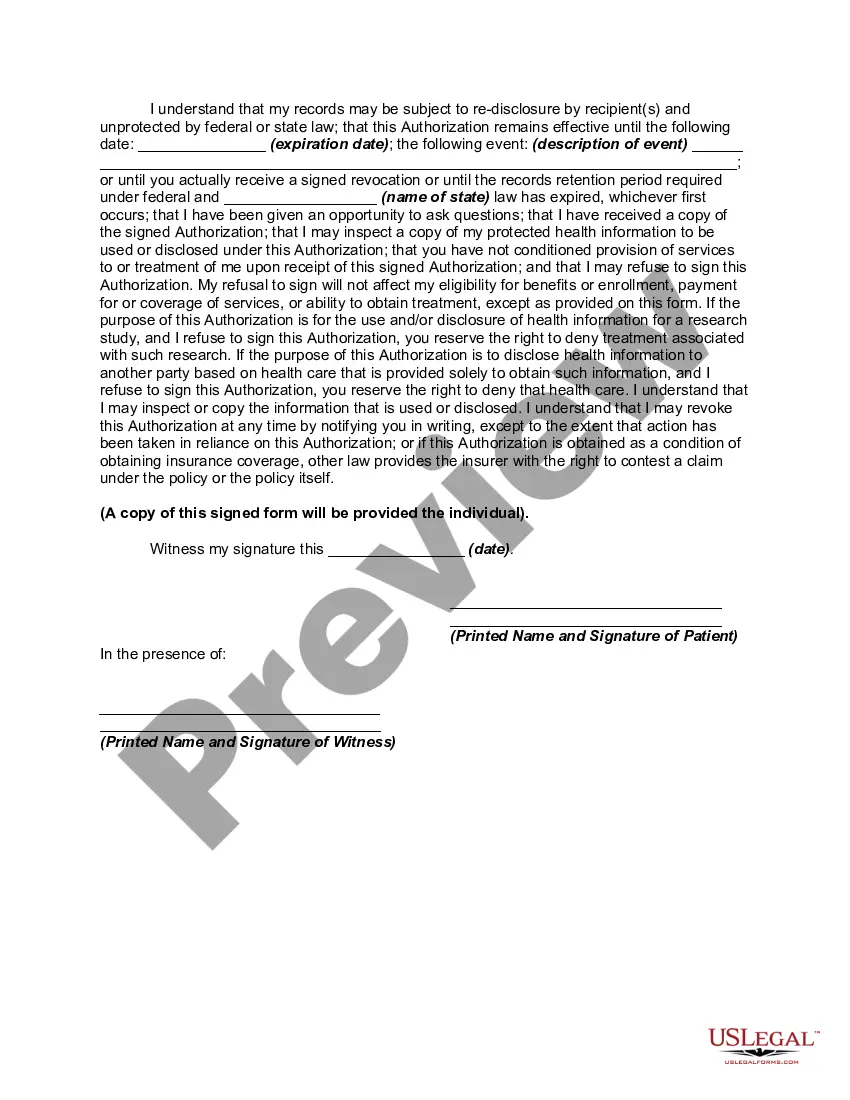
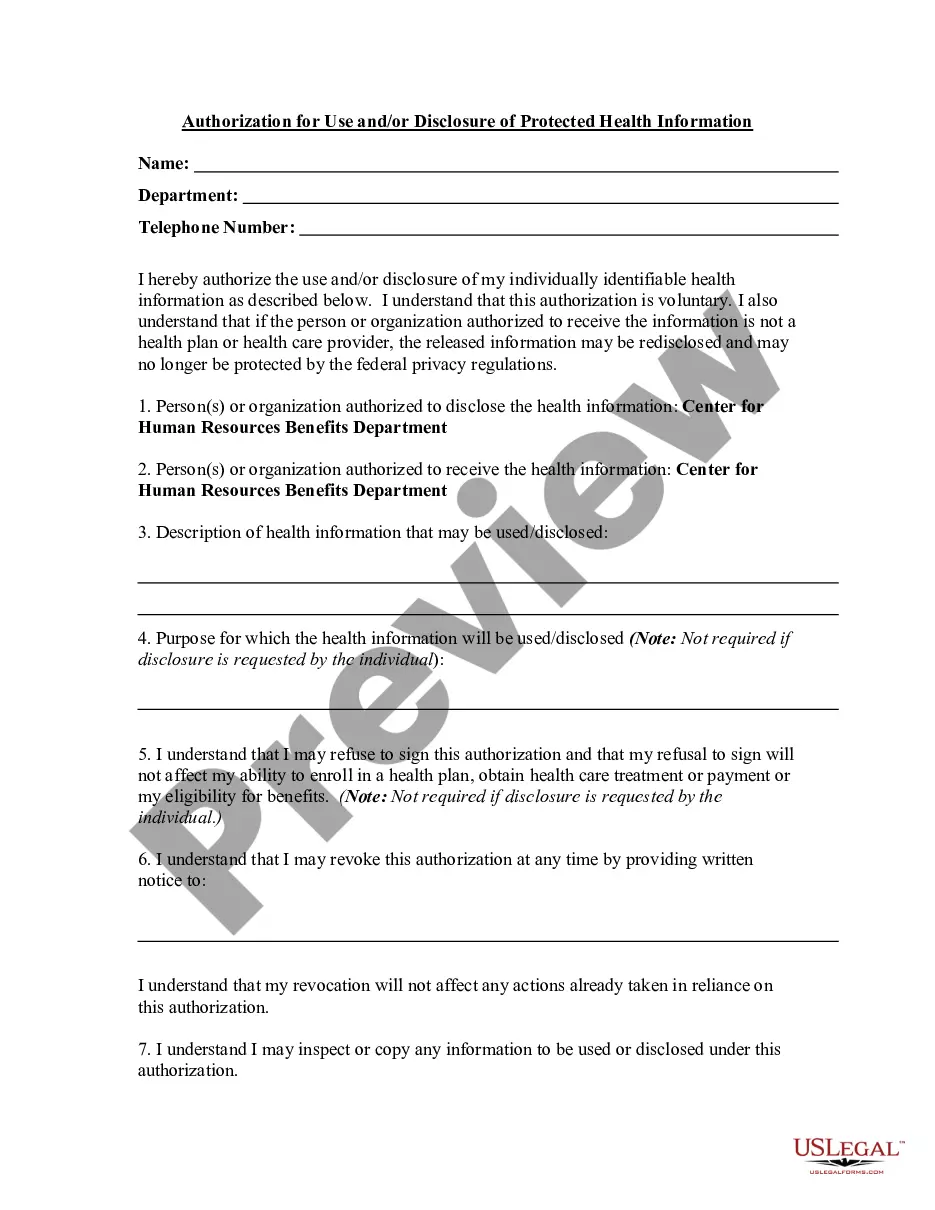
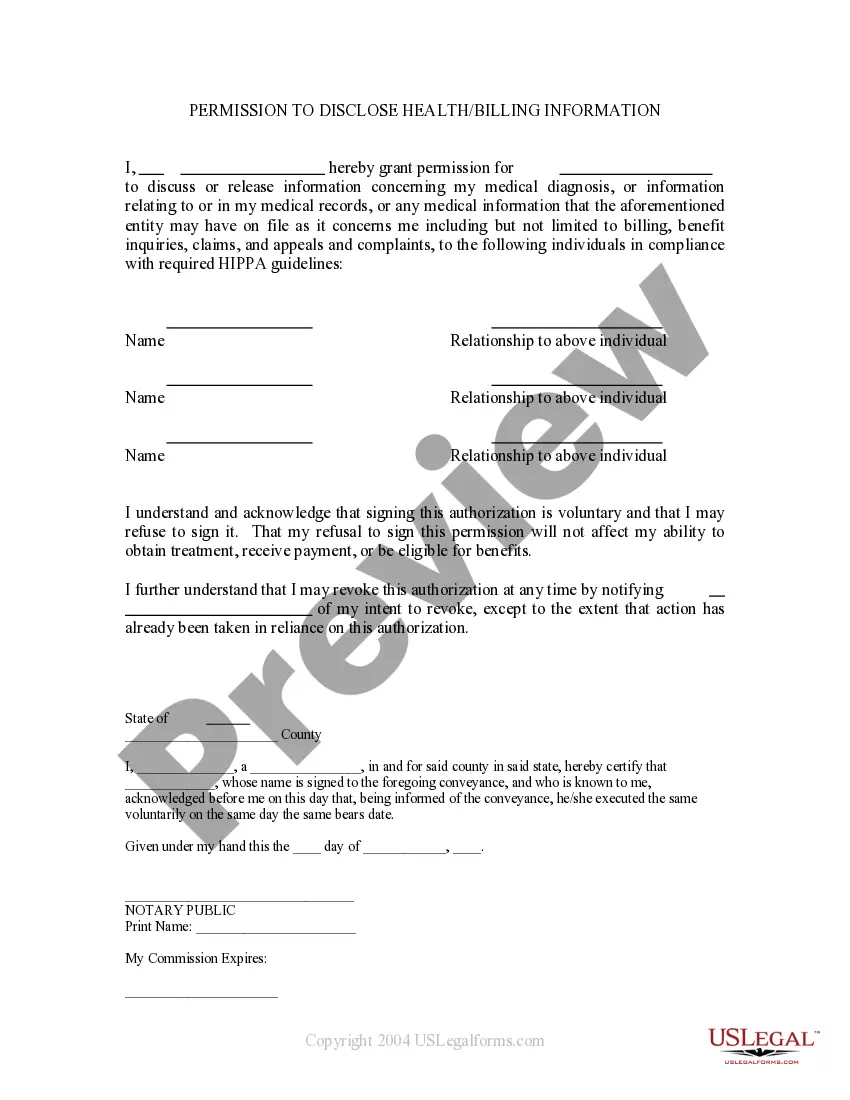
The authorization for disclosure of information form, including the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, is primarily used to obtain a patient's consent before releasing their health information. This form outlines the specific details regarding what information will be shared and with whom. Using this form helps safeguard patient rights and encourages transparency in healthcare practices.
Yes, the definition encompasses an authorization like the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, which supports the combined use of patient-specific health data with other documents. This ensures that the sharing of health information is conducted within a legal framework, securing patient confidentiality. Having such an authorization can simplify complex healthcare interactions.
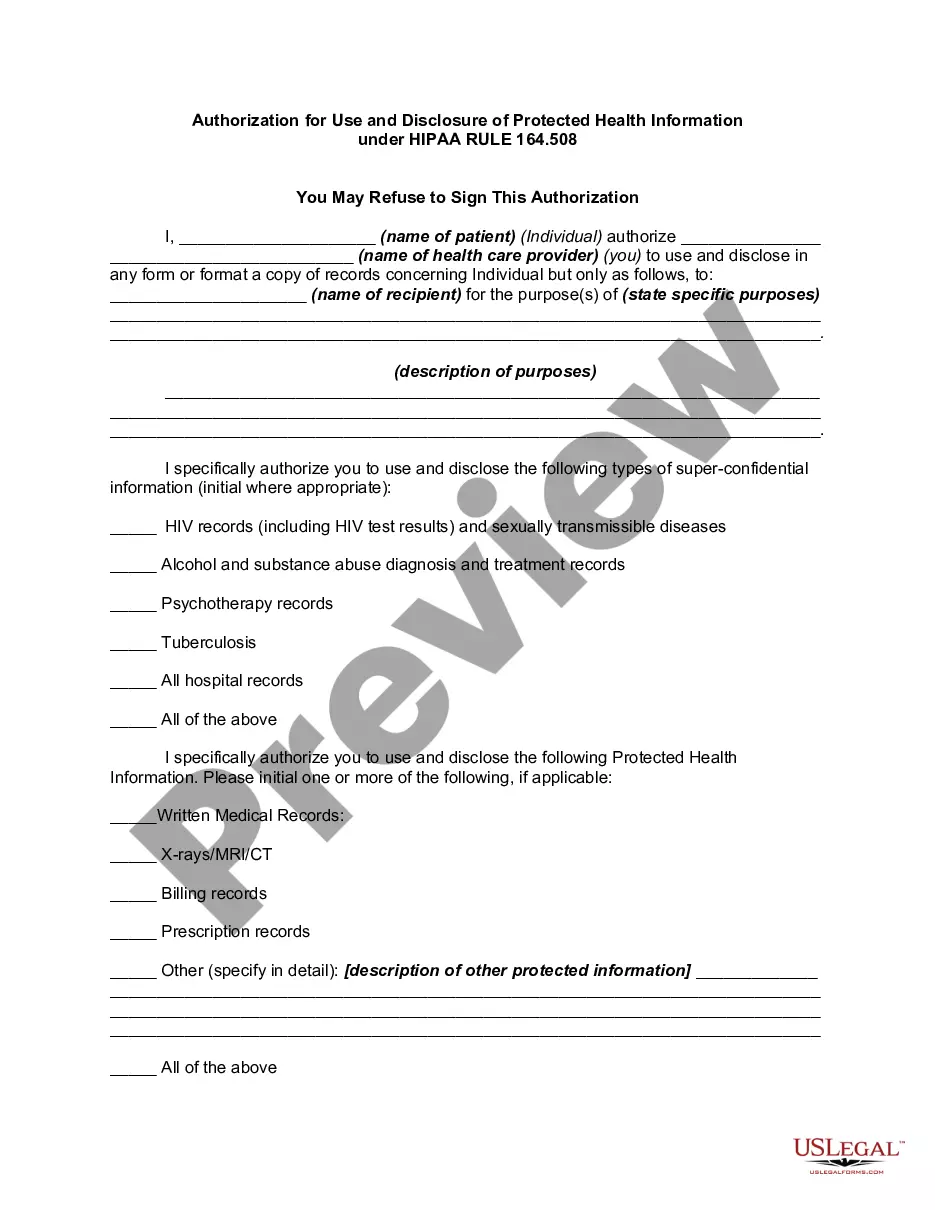
HIPAA requires a signed authorization for use or disclosure of protected health information (PHI) that includes sensitive data, like mental health records, substance abuse treatment information, and genetic information. The Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 must be used for these types of PHI to ensure legal compliance. Understanding which information necessitates an authorization supports better management of health records.
A patient authorization for disclosure of health information, such as the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, is a formal consent that allows healthcare providers to release a patient's health records. This document grants permission for the use of personal health information for specified purposes. It empowers patients by giving them control over who accesses their medical information.
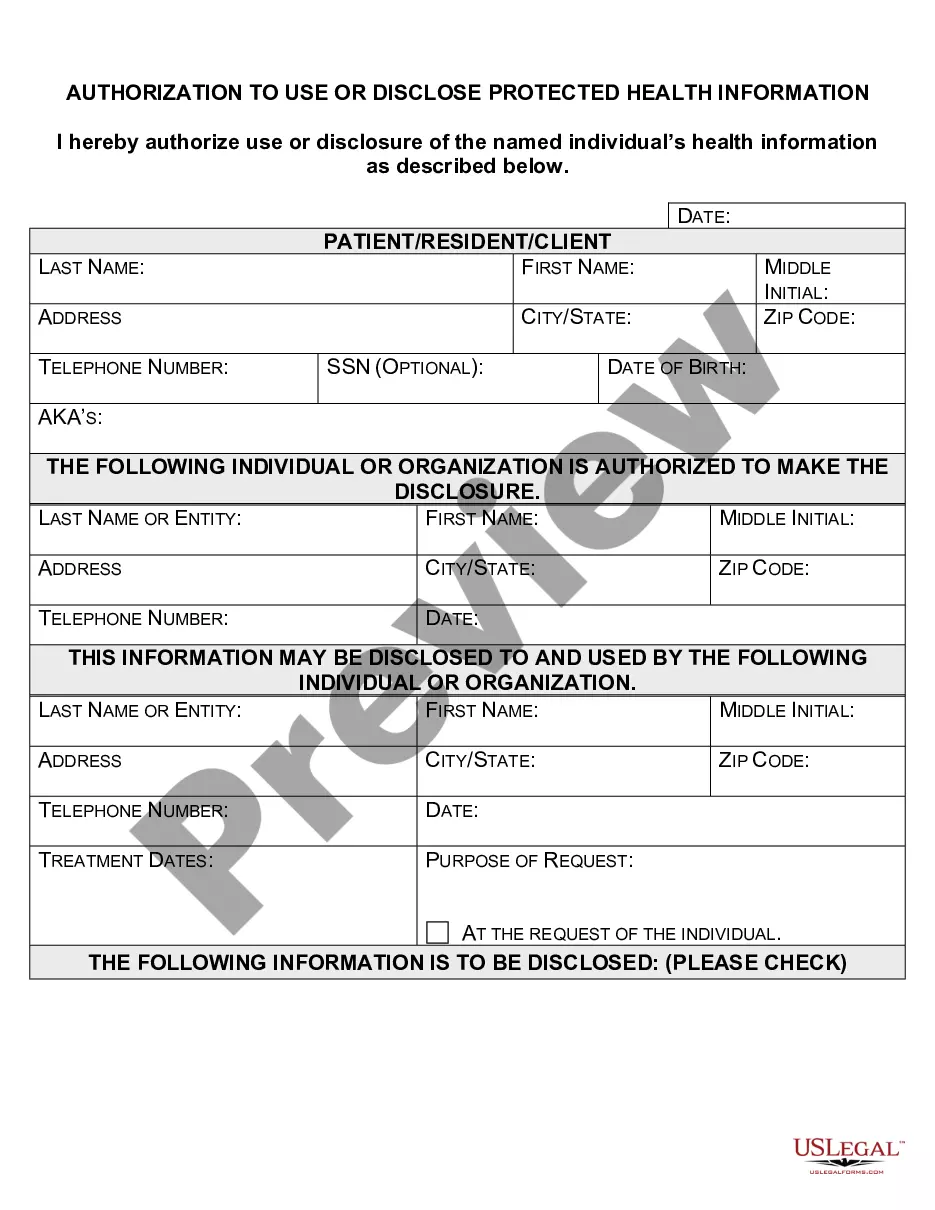
When HIPAA requires authorization to disclose information, the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 must clearly specify the information being shared. It must include details about the purpose of the disclosure, the entities involved, and the duration of the authorization. This clarity protects patient privacy and helps prevent misuse of health information.
The Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 refers to an official consent that allows a healthcare provider to combine patient-specific health information with additional documents. This authorization ensures that sensitive information is shared legally and securely. By utilizing this form, you can better manage the flow of information while maintaining compliance with HIPAA regulations.
To obtain HIPAA approval, start by completing the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 form. This form outlines how you will use and protect health information in compliance with HIPAA regulations. Next, submit the completed form to the appropriate parties to ensure they understand your privacy practices. Utilizing platforms like uslegalforms can simplify this process, ensuring that your forms are accurate and compliant with the necessary legal standards.
A HIPAA waiver of authorization form is a document that allows healthcare providers to share your protected health information without obtaining your explicit permission. This form is important because it enables the flow of information for important purposes such as research or public health. The Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 outlines the specific conditions under which this waiver applies. For more streamlined compliance, consider using the resources available on US Legal Forms, which provide clear templates to facilitate the process.
A patient's authorization for disclosure of PHI (Protected Health Information) is a formal permission allowing healthcare providers to share specific health information with designated individuals or entities. This authorization must comply with regulations, such as the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, ensuring that the patient's rights and preferences are respected. It is crucial for maintaining the integrity and confidentiality of health information.
To properly fill out the authorization for use and disclosure of protected health information, follow the structured format of the form. Clearly state your consent and identify the party receiving the information. Include the specific type of health information being disclosed and ensure that the authorization is dated and signed. Platforms like uslegalforms can provide you with the necessary templates and examples for the Delaware Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508.