Delaware Notice of Special Enrollment Rules is a set of regulations that govern the special enrollment periods (SEPs) offered by the state of Delaware for individuals seeking health insurance coverage outside the annual open enrollment period. These SEPs allow eligible individuals to enroll in health insurance plans or make changes to their existing coverage due to specific qualifying life events. Delaware offers several types of Notice of Special Enrollment Rules, including but not limited to: 1. Birth or adoption: This type of SEP allows individuals who have recently given birth or adopted a child to enroll themselves and their dependent(s) in health insurance coverage. It ensures the necessary healthcare support for the newborn or adopted child. 2. Loss of previous coverage: Individuals who have experienced a loss of previous health insurance coverage, either due to job loss, expiration of a COBRA plan, or loss of Medicaid/CHIP eligibility, may be eligible for a SEP in Delaware. This rule helps prevent a gap in healthcare coverage for those facing sudden loss or termination of their existing plans. 3. Marriage or domestic partnership: A SEP is available for individuals who get married or enter into a domestic partnership. This allows them to enroll in or make changes to their health insurance coverage to accommodate the new marital or partnership status. 4. Relocation: When individuals move into Delaware or within the state's boundaries, they may qualify for a SEP to obtain health insurance coverage or switch their plans accordingly. This ensures that individuals have access to local healthcare services upon their relocation. 5. Change in household size: Individuals who experience a change in their household size due to divorce, legal separation, death, or the loss or gain of a dependent may be eligible for a SEP. This allows them to adjust their health insurance coverage to reflect the updated household composition accurately. It is essential to abide by the Delaware Notice of Special Enrollment Rules to take advantage of these SEPs. In order to qualify, individuals must provide documentation or proof of the qualifying life event within a specific timeframe, usually 60 days from the occurrence of the event. Compliance with these rules ensures that individuals can access health insurance coverage when they need it the most.
Delaware Notice of Special Enrollment Rules
Description
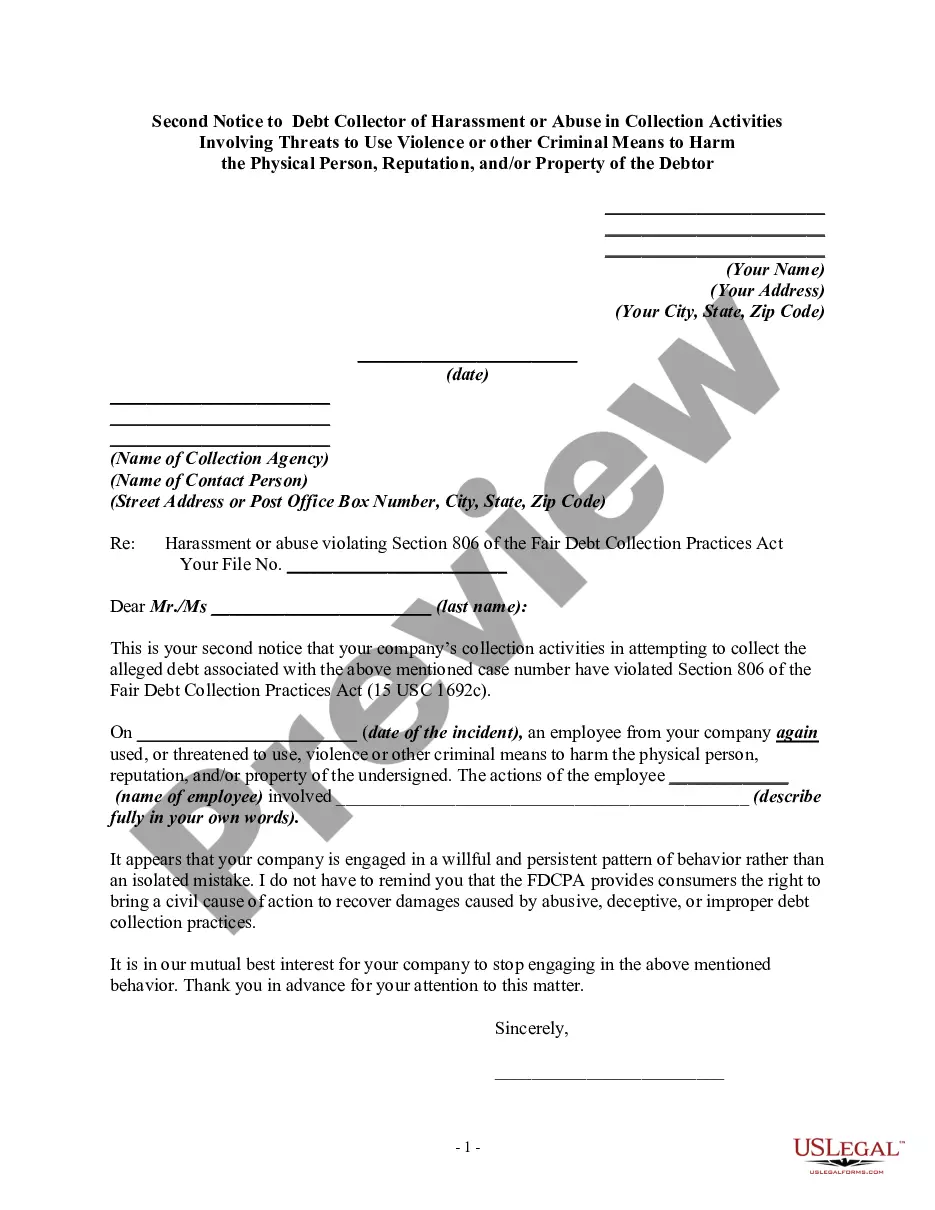
How to fill out Delaware Notice Of Special Enrollment Rules?
US Legal Forms - one of several greatest libraries of lawful forms in America - delivers a wide range of lawful record themes it is possible to obtain or produce. While using site, you can get thousands of forms for organization and personal uses, sorted by groups, says, or key phrases.You can get the latest types of forms such as the Delaware Notice of Special Enrollment Rules within minutes.
If you already have a membership, log in and obtain Delaware Notice of Special Enrollment Rules from your US Legal Forms catalogue. The Down load button will show up on every single form you view. You get access to all earlier downloaded forms within the My Forms tab of the bank account.
If you wish to use US Legal Forms initially, listed below are basic instructions to get you started:
- Ensure you have picked the proper form to your metropolis/county. Click the Review button to analyze the form`s information. Browse the form description to ensure that you have chosen the proper form.
- When the form doesn`t suit your specifications, use the Look for discipline near the top of the monitor to get the the one that does.
- When you are satisfied with the form, confirm your selection by simply clicking the Acquire now button. Then, select the prices plan you favor and offer your qualifications to register to have an bank account.
- Approach the deal. Make use of your Visa or Mastercard or PayPal bank account to perform the deal.
- Choose the file format and obtain the form in your gadget.
- Make alterations. Load, modify and produce and indication the downloaded Delaware Notice of Special Enrollment Rules.
Every single design you added to your bank account lacks an expiry day and is your own permanently. So, if you wish to obtain or produce yet another copy, just check out the My Forms section and then click in the form you require.
Obtain access to the Delaware Notice of Special Enrollment Rules with US Legal Forms, probably the most considerable catalogue of lawful record themes. Use thousands of expert and express-particular themes that meet up with your business or personal requirements and specifications.