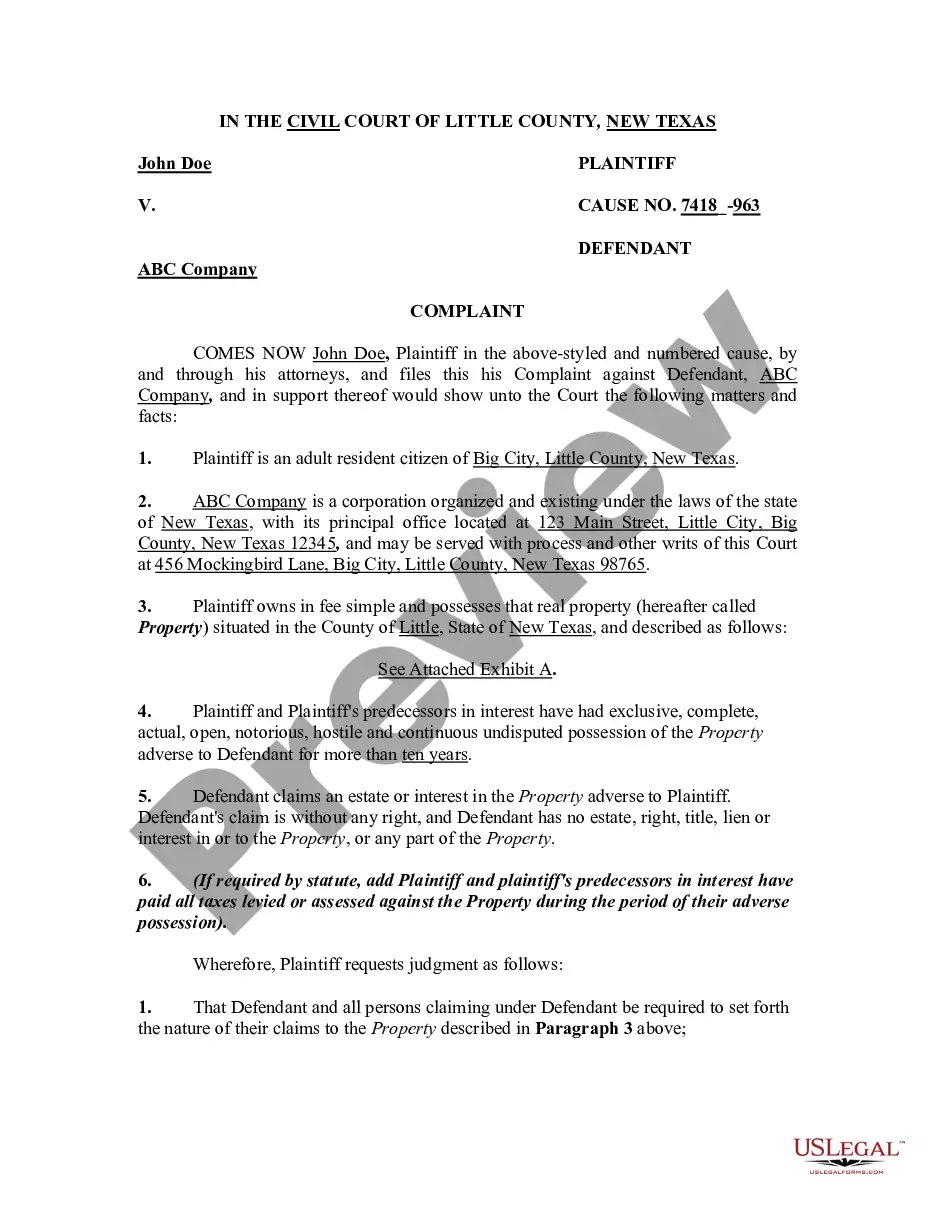
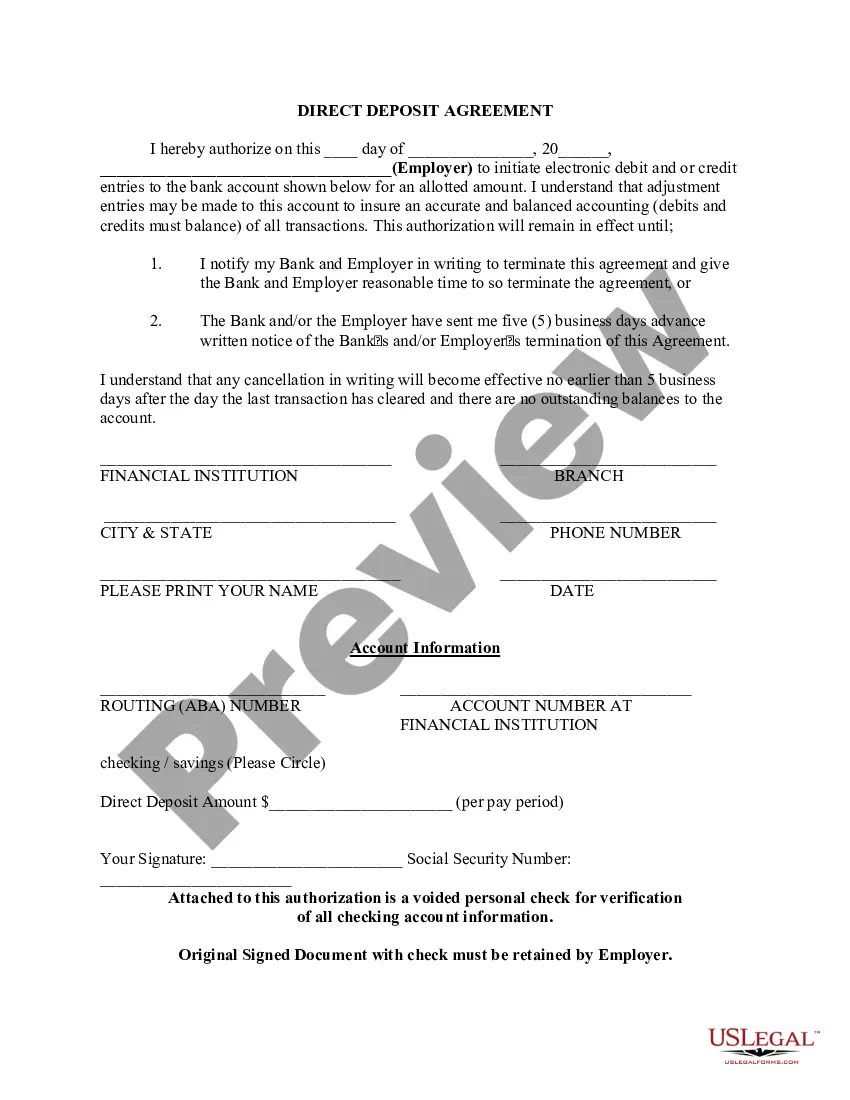
Title: Delaware Introductory COBRA Letter: A Detailed Description of its Purpose and Importance Introduction: The Delaware Introductory COBRA Letter serves as a vital communication tool between employers and employees when it comes to providing information about the Consolidated Omnibus Budget Reconciliation Act (COBRA) and their rights to continued health insurance coverage. This letter aims to educate employees about their options and obligations, ensuring a smooth transition in the event of job loss or certain qualifying life events. This article provides a comprehensive description of the Delaware Introductory COBRA Letter, its significance, and potential variations. 1. Understanding COBRA: COBRA is a federal law that allows individuals and their dependents the option to continue group health insurance coverage for a limited period after certain qualifying events, such as termination of employment, reduction of work hours, divorce, or the death of the covered employee. The Delaware Introductory COBRA Letter informs employees of this valuable benefit and explains their eligibility under Delaware state-specific regulations. 2. Purpose of the Introductory COBRA Letter: The Delaware Introductory COBRA Letter is an essential communication sent by employers to employees who become eligible for COBRA benefits. Key objectives of the letter include: — Educating employees about their COBRA rights and notifying them of their eligibility status. — Providing detailed information on the cost of coverage, duration, and terms and conditions of continued health insurance. — Clearly explaining the employee's responsibilities, including enrollment deadlines, premium payment guidelines, and reasons for potential termination of coverage. — Offering guidance on how to navigate the COBRA enrollment process and who to contact for assistance. 3. Components of the Delaware Introductory COBRA Letter: To convey the necessary information effectively, the Delaware Introductory COBRA Letter should include the following elements: — Header: Clearly stating the letter as an "Introductory COBRA Letter" for immediate identification. — Introduction: Expressing empathy for the employee's circumstances and acknowledging their eligibility for COBRA benefits. — Explanation of Qualifying Event: Detailing the specific event that triggered their eligibility, such as termination of employment or a reduction in hours. — Coverage Details: Outlining the available health insurance coverage options, including plan names and their corresponding costs. — Premium Payment Instructions: Providing clear instructions on how to remit premium payments, payment due dates, and acceptable payment methods. — Enrollment Deadline: Specifying the deadline by which the employee must enroll to ensure uninterrupted coverage. — Termination Conditions: Clearly outlining circumstances that can lead to the premature termination of COBRA coverage. — Contact Information: Sharing relevant contact details for both the employer and the designated COBRA administrator responsible for assisting employees with enrollment and addressing any concerns. Different Types of Delaware Introductory COBRA Letters: While the essential purpose of the Delaware Introductory COBRA Letter remains the same across different organizations, terminology, formatting, and additional information may vary. Possible variations may include: 1. Basic Introductory COBRA Letter: Providing standard information on coverage options, payment instructions, and relevant deadlines. 2. Expanded Introductory COBRA Letter: Offering more comprehensive details on topics like flexible spending accounts, health savings accounts, and additional benefits. 3. Electronic Introductory COBRA Letter: Delivering the letter digitally through email or electronic employee portals for convenience and environmental friendliness. Conclusion: The Delaware Introductory COBRA Letter plays a crucial role in ensuring employee awareness and understanding of their COBRA rights. By effectively communicating important details, employers support their employees during challenging times of transitioning healthcare coverage, offering peace of mind and guiding them towards a seamless continuation of benefits.
Delaware Introductory COBRA Letter
Description
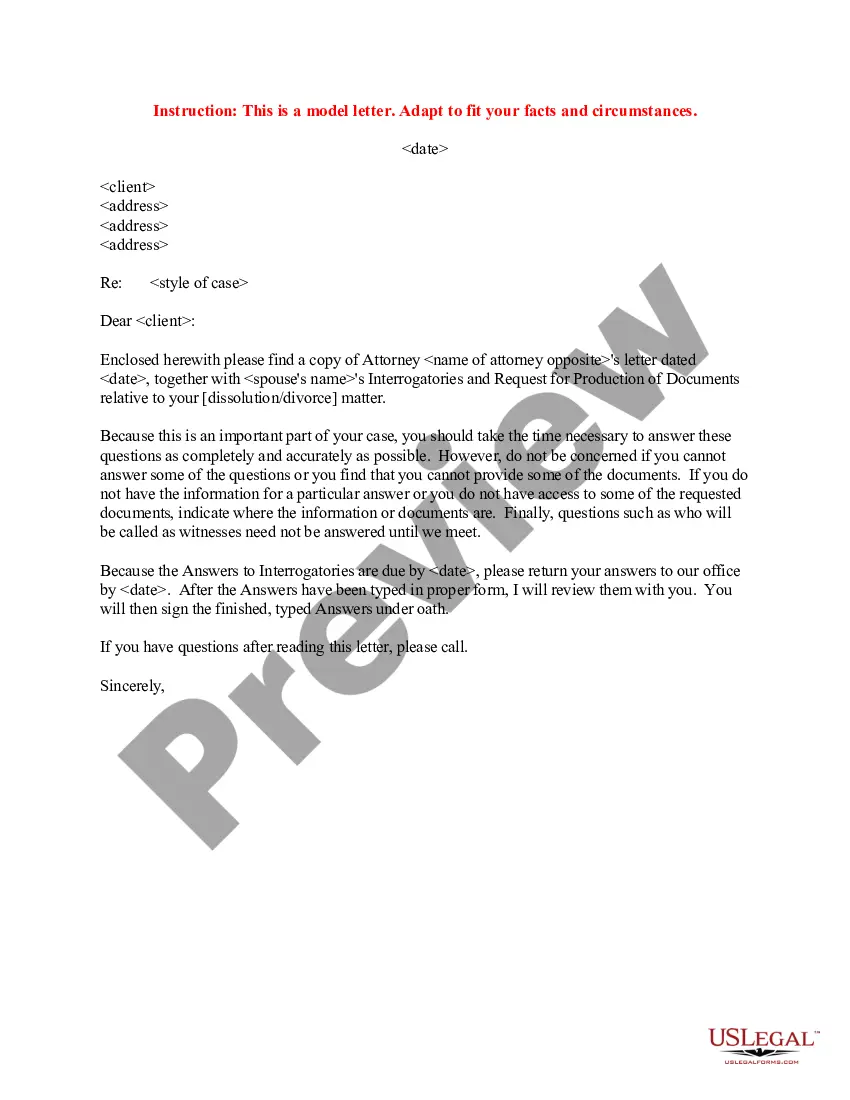
How to fill out Delaware Introductory COBRA Letter?
Choosing the best lawful papers template can be quite a battle. Needless to say, there are plenty of templates accessible on the Internet, but how do you discover the lawful develop you will need? Take advantage of the US Legal Forms web site. The support provides a huge number of templates, such as the Delaware Introductory COBRA Letter, that can be used for company and private requirements. Every one of the types are checked by professionals and satisfy federal and state specifications.
Should you be currently listed, log in for your profile and then click the Acquire option to obtain the Delaware Introductory COBRA Letter. Make use of profile to look throughout the lawful types you have purchased previously. Proceed to the My Forms tab of your own profile and get another version of your papers you will need.
Should you be a whole new consumer of US Legal Forms, listed here are easy instructions that you can comply with:
- Initial, make certain you have chosen the correct develop to your city/area. It is possible to look through the shape while using Review option and look at the shape description to guarantee this is basically the best for you.
- In the event the develop does not satisfy your preferences, utilize the Seach area to find the correct develop.
- When you are positive that the shape is acceptable, select the Buy now option to obtain the develop.
- Pick the costs strategy you would like and enter in the essential information and facts. Make your profile and purchase the transaction utilizing your PayPal profile or credit card.
- Opt for the document format and acquire the lawful papers template for your device.
- Comprehensive, modify and print out and signal the obtained Delaware Introductory COBRA Letter.
US Legal Forms is definitely the largest collection of lawful types where you can see various papers templates. Take advantage of the service to acquire expertly-made paperwork that comply with state specifications.
Form popularity
FAQ
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
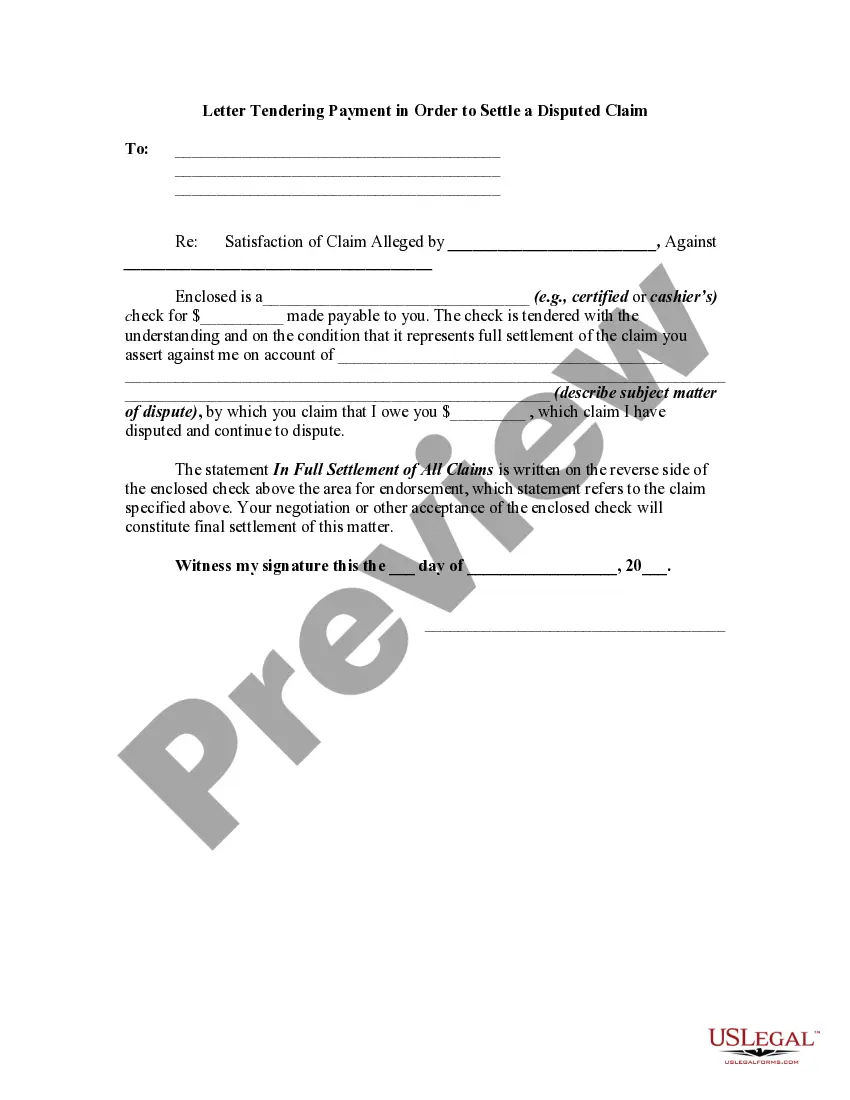
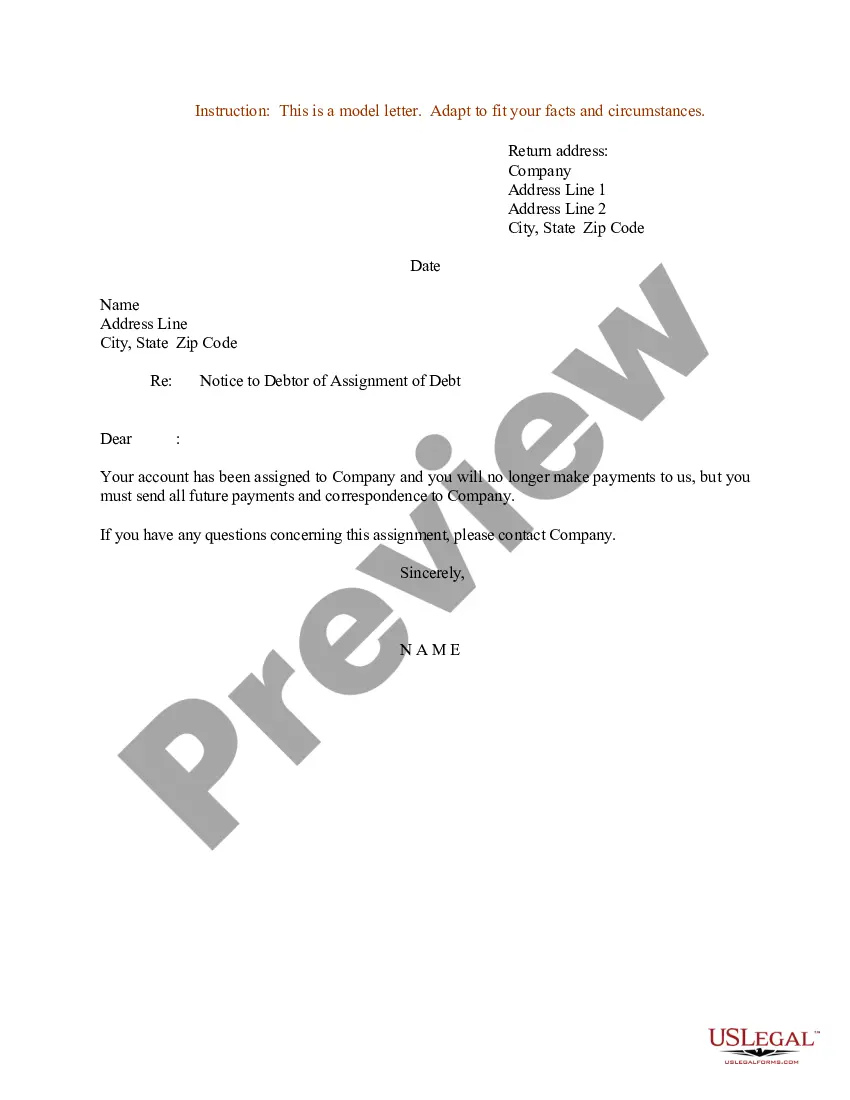
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
How COBRA Works In Delaware. The Federal COBRA Law requires businesses with 20 or more workers to provide the option to elect the same group health coverage to workers and their families if that insurance would end. Exempt from this rule are government employers, churches and tax-exempt organizations.
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.