Title: Understanding the Florida Summary of Rights and Obligations under COBRA: A Comprehensive Overview Introduction: The Florida Summary of Rights and Obligations under COBRA (Consolidated Omnibus Budget Reconciliation Act) outlines the regulations and provisions applicable to employees and their dependents when faced with the loss of employer-sponsored healthcare coverage. This comprehensive summary seeks to provide an in-depth understanding of the different aspects and types of COBRA for Florida residents, highlighting key elements and potential obligations. 1. Types of Florida Summary of Rights and Obligations under COBRA: a) State Continuation Coverage: Apart from the federal COBRA provisions, the state of Florida offers its own continuation coverage plan. Employees working for smaller employers or those not covered under federal COBRA may be eligible for state continuation coverage. b) Federal COBRA Coverage: The federal COBRA legislation mandates that employers with 20 or more employees must provide continuation coverage to eligible individuals who experience qualifying events like job loss, reduction in work hours, or certain life events. 2. Eligibility for COBRA Coverage in Florida: To qualify for COBRA coverage in Florida, individuals must meet certain criteria, including: — Being covered by a group health plan on the day before a qualifying event. — Experiencing a qualifying event leading to the loss of coverage. — Not engaging in misconduct that would disqualify them from coverage. 3. Key Components of Florida Summary of Rights and Obligations: a) Notification Requirements: Employers are required to provide employees and their dependents with specific written notices regarding their COBRA rights, including general notice, election notice, and notice of unavailability before the expiry of their health coverage. b) Election Period: The Florida Summary of Rights and Obligations stipulates that eligible individuals have 60 days to elect COBRA coverage from the date they receive the election notice. If not elected within this period, the right to COBRA coverage may be forfeited. c) Duration of Coverage: Under COBRA, eligible beneficiaries can generally maintain their employer-sponsored health coverage for up to 18-36 months, depending on the qualifying event. d) Cost of Coverage: Beneficiaries who elect COBRA coverage are responsible for paying the entire premium, including the portion previously paid by the employer. However, an additional 2% administrative fee may be added. e) Continuation Periods for Dependents: The summary outlines the continuation periods for different types of dependents, such as spouses, dependent children, and those who become disabled within 60 days of COBRA coverage beginning. 4. COBRA and Florida State Continuation Coverage Comparison: The Florida Summary of Rights and Obligations under COBRA also highlights the differences between federal COBRA and state continuation coverage, such as variations in qualifying events, duration, and notification requirements. Conclusion: The Florida Summary of Rights and Obligations under COBRA encompasses both federal COBRA and state continuation coverage, providing critical information to employees and their dependents regarding their rights, obligations, and opportunities to secure continued healthcare coverage. Understanding the various components and types of COBRA ensures individuals can make informed decisions during times of job loss, reduced work hours, or significant life events.
Florida Summary of Rights and Obligations under COBRA
Description
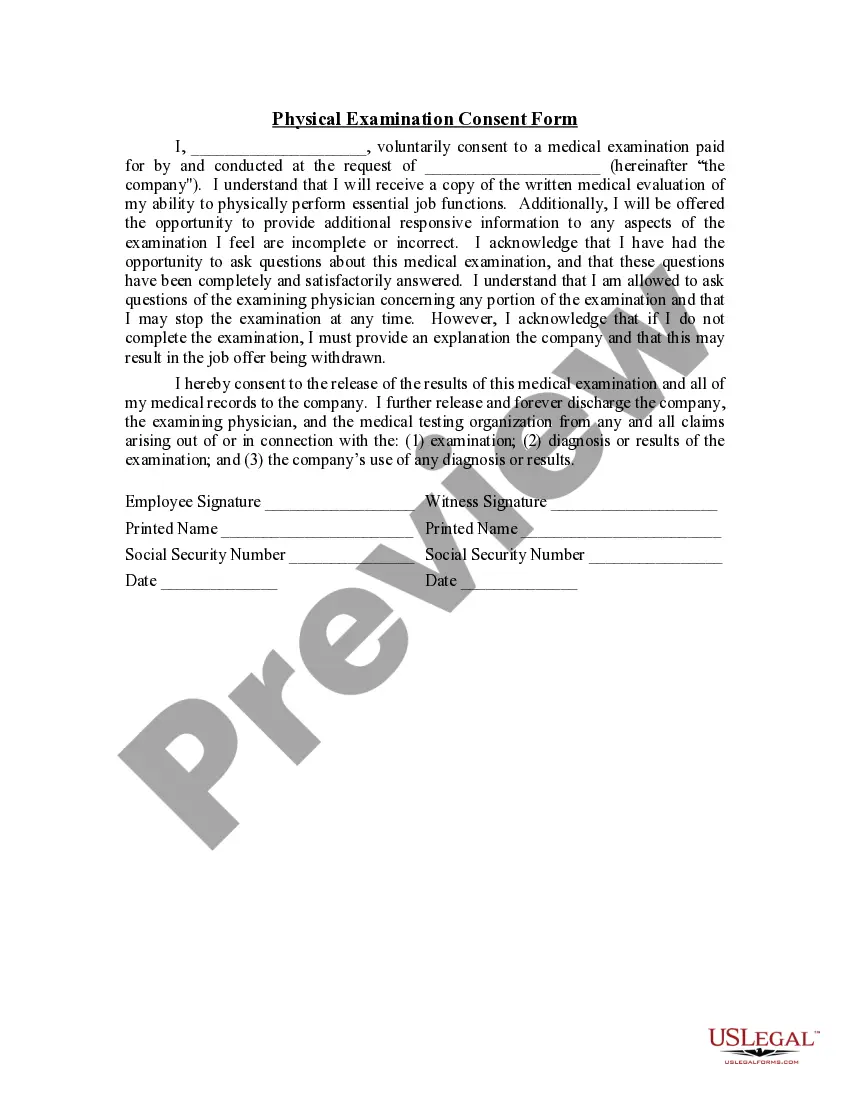
How to fill out Florida Summary Of Rights And Obligations Under COBRA?
Discovering the right lawful papers design could be a struggle. Obviously, there are a variety of themes accessible on the Internet, but how can you discover the lawful form you will need? Take advantage of the US Legal Forms internet site. The service delivers 1000s of themes, such as the Florida Summary of Rights and Obligations under COBRA, that you can use for organization and private needs. All the varieties are checked by specialists and satisfy federal and state requirements.
If you are already registered, log in to the bank account and click the Acquire switch to obtain the Florida Summary of Rights and Obligations under COBRA. Make use of your bank account to look through the lawful varieties you may have ordered formerly. Check out the My Forms tab of your respective bank account and have yet another version from the papers you will need.
If you are a new end user of US Legal Forms, here are straightforward instructions that you can follow:
- First, make certain you have chosen the correct form for your personal metropolis/area. You can check out the shape while using Preview switch and browse the shape information to make certain this is basically the best for you.
- In the event the form does not satisfy your preferences, utilize the Seach area to discover the correct form.
- Once you are sure that the shape is suitable, select the Get now switch to obtain the form.
- Pick the pricing strategy you need and enter in the required information and facts. Create your bank account and buy your order using your PayPal bank account or Visa or Mastercard.
- Opt for the document file format and down load the lawful papers design to the device.
- Full, edit and printing and indicator the obtained Florida Summary of Rights and Obligations under COBRA.
US Legal Forms is the biggest local library of lawful varieties for which you can find a variety of papers themes. Take advantage of the company to down load expertly-created papers that follow condition requirements.
Form popularity
FAQ
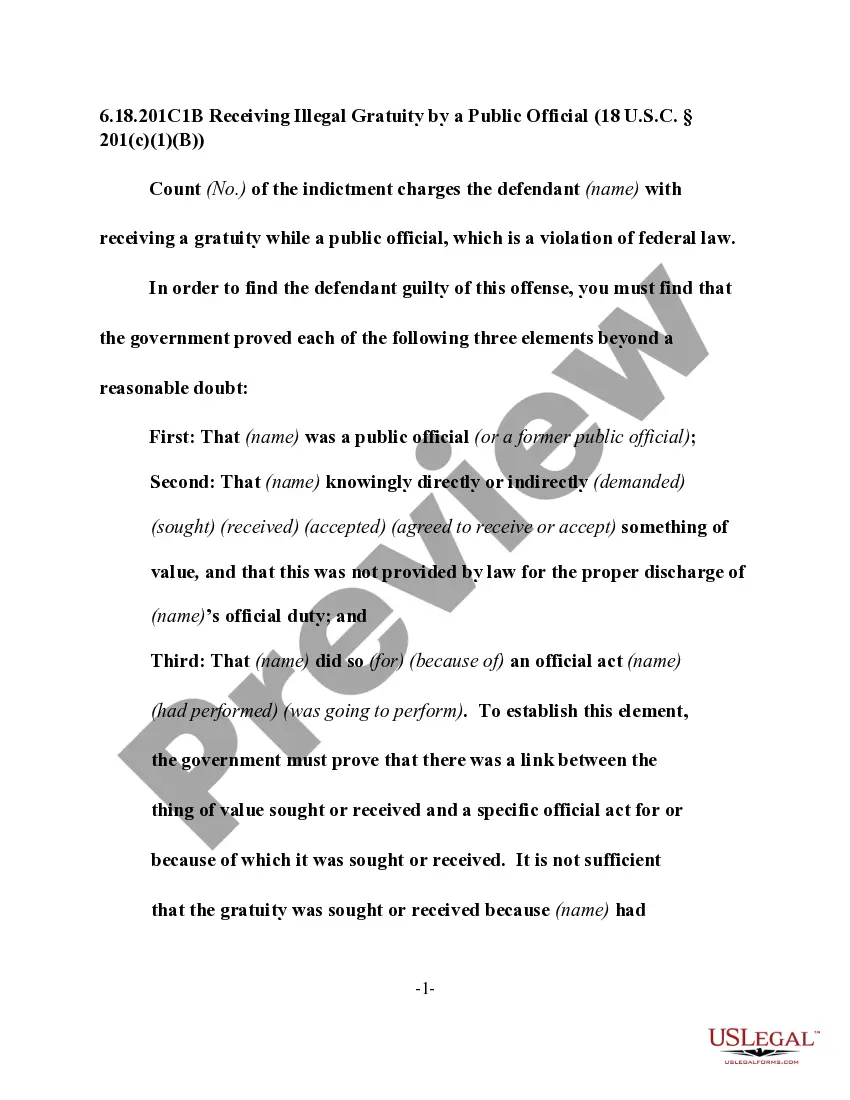
COBRA. The Consolidated Omnibus Budget Reconciliation Act (COBRA) allows employees, retirees, and their families, to continue coverage of health, dental and vision benefits through their employer group plan for limited periods of time under certain circumstances, including: Voluntary or involuntary job loss.
To elect COBRA insurance in Florida, an individual must experience one of the following: Quit their job. Be fired unless it was due to gross misconduct. Have their hours reduced, and they no longer qualify for their employer's health plan because they are no longer considered full time.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Under Florida COBRA insurance, employees can continue their healthcare coverage for a minimum of 18 months, while their spouses and children may receive coverage for up to three years.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.