Florida Election Form for Continuation of Benefits - COBRA
Description
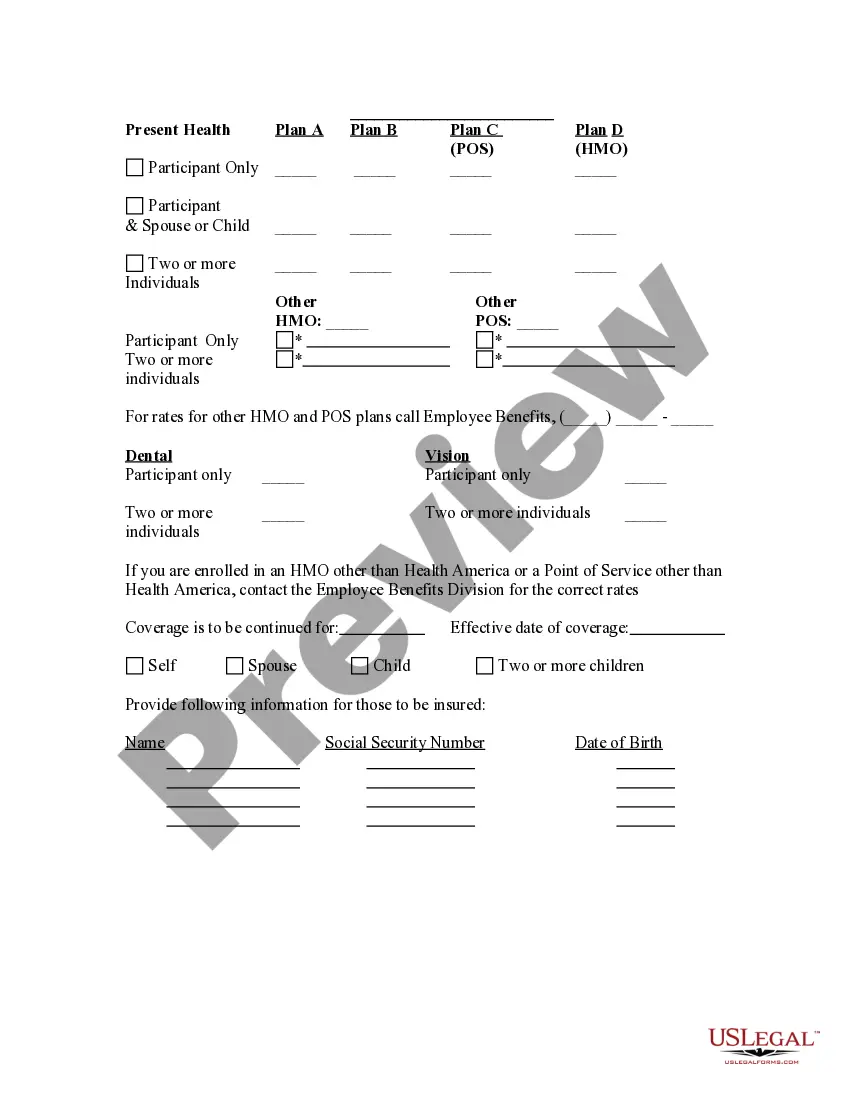
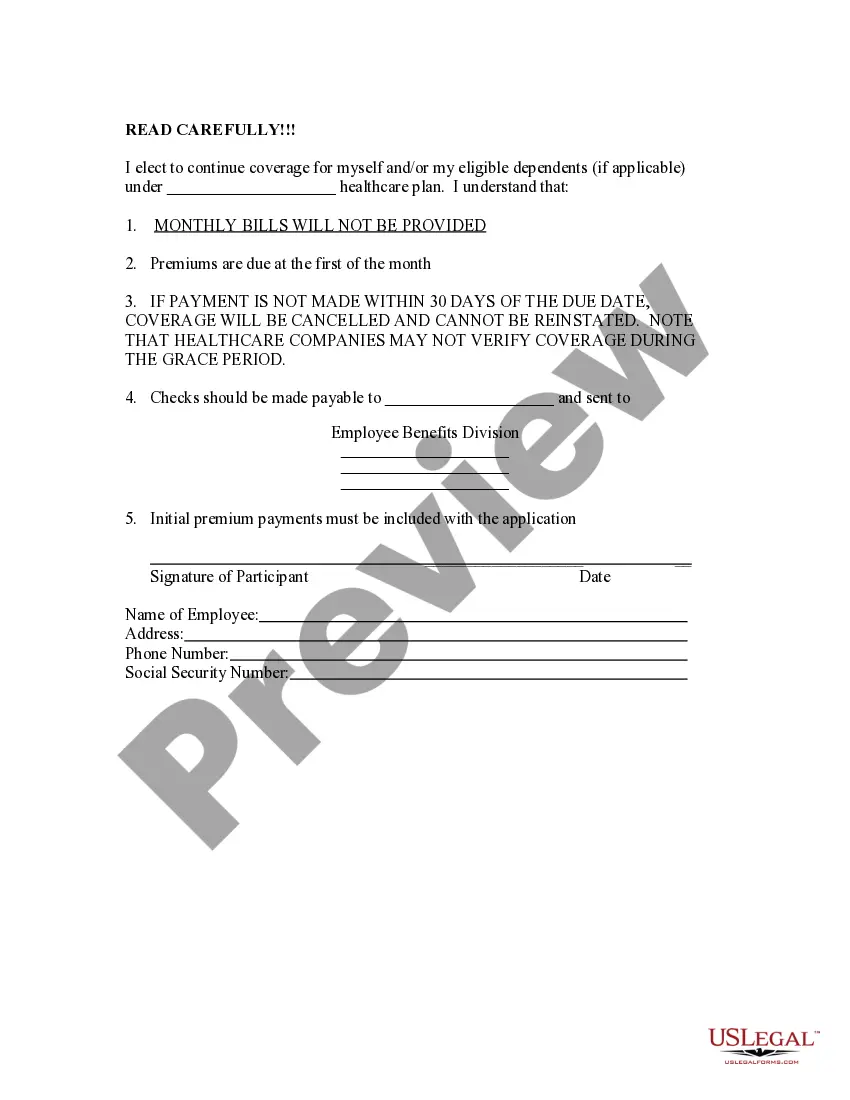
How to fill out Election Form For Continuation Of Benefits - COBRA?
Choosing the best legitimate record design might be a have difficulties. Naturally, there are a variety of templates accessible on the Internet, but how would you discover the legitimate develop you will need? Use the US Legal Forms internet site. The support gives a huge number of templates, for example the Florida Election Form for Continuation of Benefits - COBRA, which can be used for company and private demands. Every one of the types are examined by pros and meet state and federal requirements.
When you are currently registered, log in to your accounts and then click the Acquire option to obtain the Florida Election Form for Continuation of Benefits - COBRA. Make use of accounts to appear with the legitimate types you have acquired in the past. Check out the My Forms tab of your accounts and have another version from the record you will need.
When you are a whole new consumer of US Legal Forms, allow me to share easy recommendations so that you can follow:
- First, be sure you have selected the correct develop to your metropolis/region. You are able to look over the form using the Preview option and look at the form explanation to guarantee this is basically the right one for you.
- In case the develop will not meet your preferences, use the Seach discipline to obtain the right develop.
- Once you are sure that the form would work, go through the Get now option to obtain the develop.
- Opt for the rates plan you desire and enter the necessary information. Create your accounts and purchase your order with your PayPal accounts or Visa or Mastercard.
- Choose the data file formatting and acquire the legitimate record design to your product.
- Full, edit and produce and indication the acquired Florida Election Form for Continuation of Benefits - COBRA.
US Legal Forms is the greatest library of legitimate types in which you can see various record templates. Use the company to acquire professionally-made paperwork that follow state requirements.
Form popularity
FAQ
Under Florida COBRA insurance, employees can continue their healthcare coverage for a minimum of 18 months, while their spouses and children may receive coverage for up to three years.
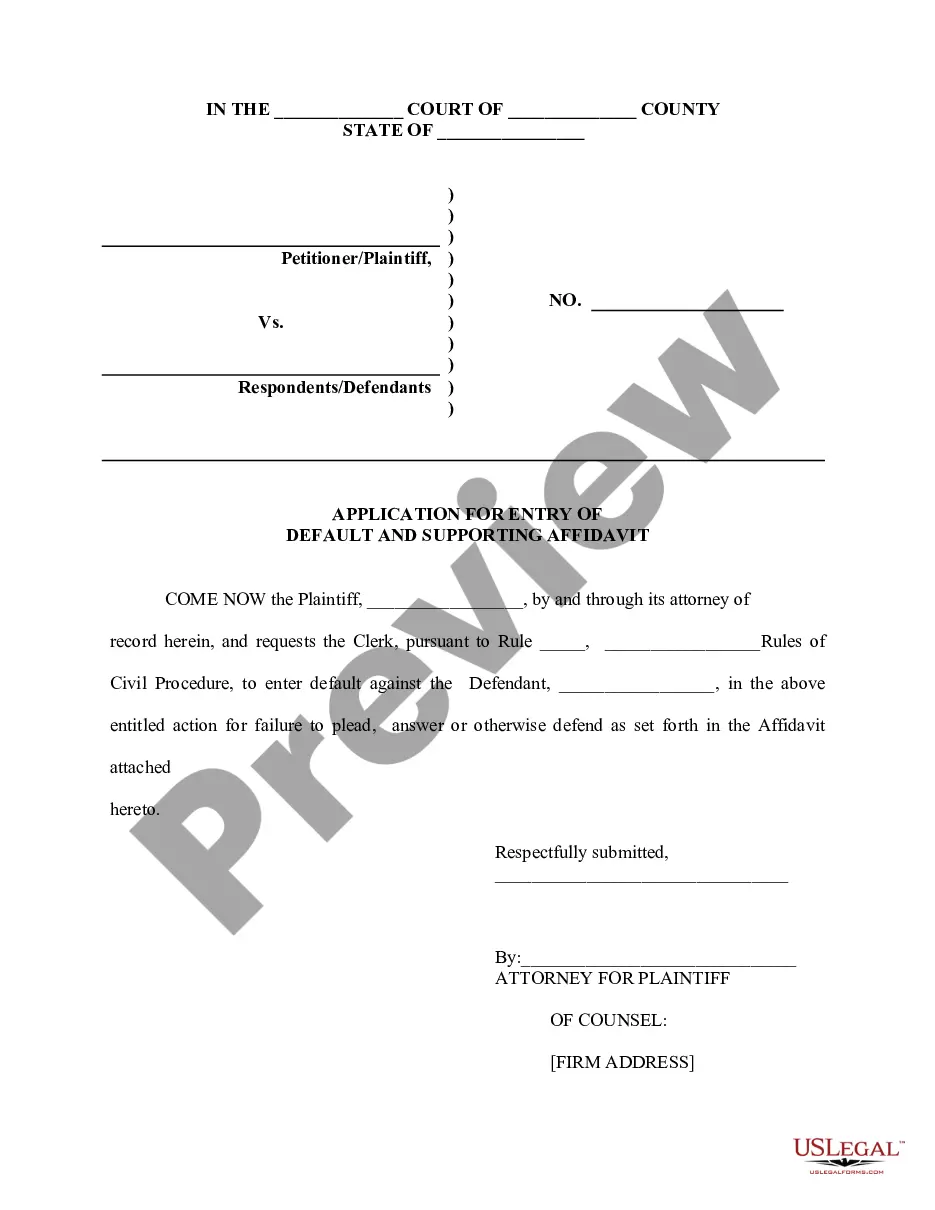
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
A covered employee's spouse who would lose coverage due to a divorce may elect continuation coverage under the plan for a maximum of 36 months. A qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or legal separation.
The temporary Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) health insurance premium subsidy Congress granted to eligible individuals through the American Rescue Plan Act of 2021 (the ARP) will expire at the end of September 2021.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
Second Qualifying Event - If you are receiving an 18-month maximum period of continuation coverage, you may become entitled to an 18-month extension (giving a total maximum period of 36 months of continuation coverage) if you experience a second qualifying event that is the death of a covered employee, the divorce or
Florida's state continuation or mini-COBRA law provides similar continuation of coverage protection for employees who work for employers with two to 19 employees. Once you elect mini-COBRA coverage, you will pay 100% of the total insurance premium plus a 15% processing fee.