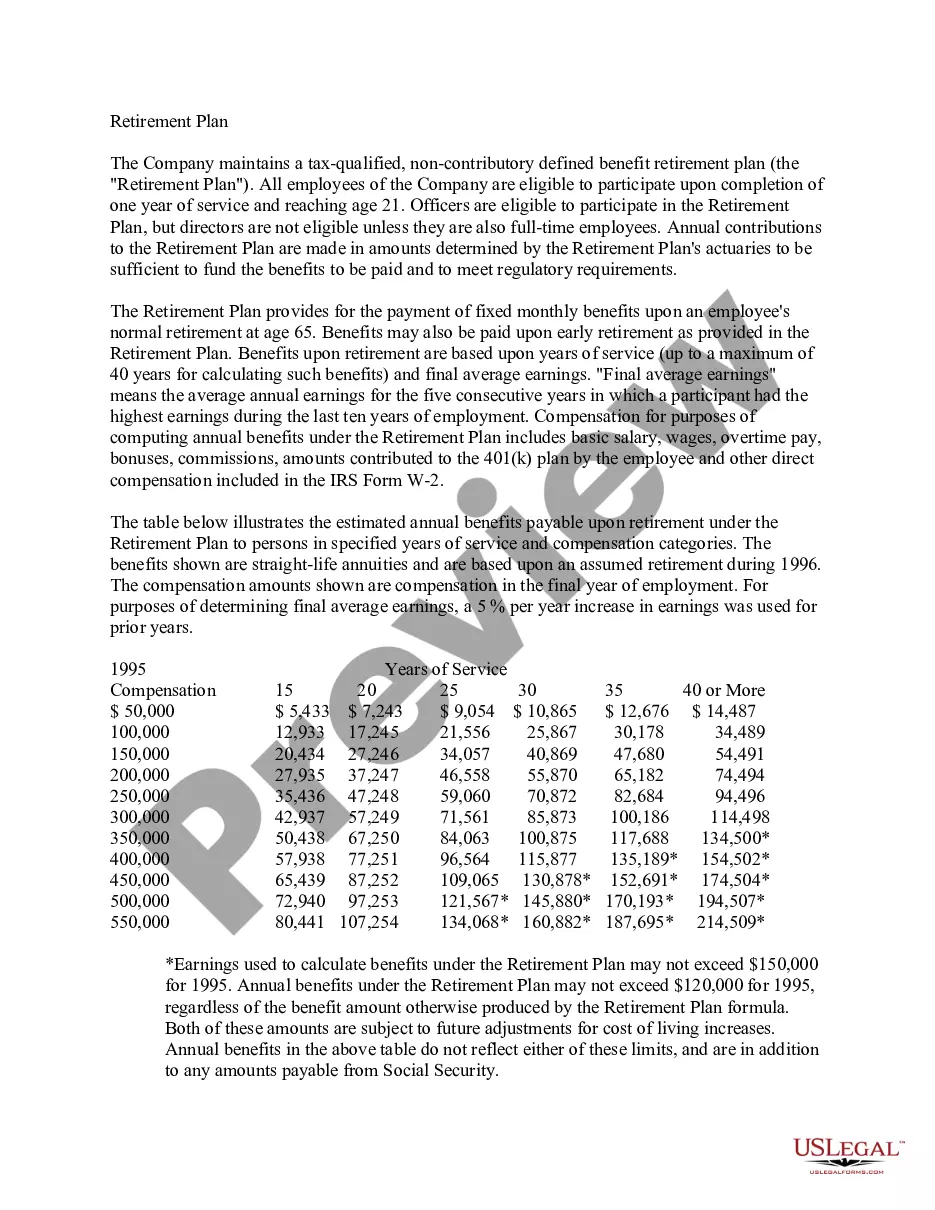
Florida Employer — Plan Administrator Notice to Employee of Unavailability of Continuation is a crucial communication issued by employers in the state of Florida when they are unable to offer continuation coverage to their employees. This notice informs employees about the unavailability of continuation options and educates them on alternative plans or options they may consider. Types of Florida Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: 1. Health Insurance Unavailability Notice: This notice is issued by the plan administrator when the employer's health insurance plan is no longer available due to unforeseen circumstances, such as bankruptcy, loss of contract with the insurance provider, or any other relevant issues. It informs employees about the termination of their health insurance coverage and provides guidance on alternative options or resources available to seek coverage. 2. COBRA Unavailability Notice: This notice is specific to employers who are unable to offer Consolidated Omnibus Budget Reconciliation Act (COBRA) continuation coverage to their employees. COBRA allows employees and their dependents to continue health coverage under the employer's group health plan for a limited time, usually after employment termination. The notice informs employees about the unavailability of COBRA coverage and advises them to explore other avenues to secure health insurance coverage. 3. Retirement Benefits Unavailability Notice: Some employers provide retirement benefits to their employees as part of their compensation package. In certain circumstances, the employer may not be able to continue offering retirement benefits, such as a 401(k) plan, due to financial difficulties, restructuring, or any other valid reasons. This notice outlines the unavailability of retirement benefits and advises employees on alternative ways to save for retirement, such as individual retirement accounts (IRAs) or other employer-sponsored retirement plans. 4. Other Employee Benefit Unavailability Notice: This category encompasses notices that pertain to the unavailability of various other employee benefits, such as dental, vision, disability, or life insurance plans. Employers may issue separate notices for each benefit to ensure employees are aware of the termination of specific benefits and provide suggestions for alternative coverage options or resources. Keywords: Florida, employer, plan administrator, notice, unavailability of continuation, health insurance, COBRA, retirement benefits, employee benefits, termination, coverage, alternative options, resources, bankruptcy, insurance provider, group health plan, Consolidated Omnibus Budget Reconciliation Act, retirement savings, dental insurance, vision insurance, disability insurance, life insurance.
Florida Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
You can devote hours on the web searching for the legitimate document format that suits the federal and state demands you want. US Legal Forms supplies a huge number of legitimate forms which are evaluated by specialists. It is possible to down load or print the Florida Employer - Plan Administrator Notice to Employee of Unavailability of Continuation from my assistance.
If you already have a US Legal Forms bank account, you are able to log in and then click the Obtain switch. Afterward, you are able to complete, change, print, or indicator the Florida Employer - Plan Administrator Notice to Employee of Unavailability of Continuation. Every single legitimate document format you purchase is yours eternally. To get an additional backup of any acquired type, check out the My Forms tab and then click the corresponding switch.
If you use the US Legal Forms website for the first time, stick to the basic instructions under:
- First, make certain you have chosen the best document format for your area/town of your liking. Look at the type explanation to ensure you have picked the appropriate type. If offered, make use of the Review switch to look with the document format as well.
- If you want to find an additional edition of your type, make use of the Research field to find the format that suits you and demands.
- When you have found the format you need, just click Purchase now to continue.
- Choose the costs prepare you need, key in your accreditations, and sign up for your account on US Legal Forms.
- Comprehensive the deal. You may use your bank card or PayPal bank account to fund the legitimate type.
- Choose the formatting of your document and down load it in your device.
- Make alterations in your document if needed. You can complete, change and indicator and print Florida Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
Obtain and print a huge number of document templates using the US Legal Forms site, which offers the largest collection of legitimate forms. Use skilled and condition-distinct templates to take on your business or person requirements.
Form popularity
FAQ
The state of Florida also has a mini-COBRA law, called the Florida Health Insurance Coverage Continuation Act, which provides a similar continuation of healthcare coverage for employees who work for small businesses with fewer than 20 employees, and who are not covered by federal requirements.
A covered employee's spouse who would lose coverage due to a divorce may elect continuation coverage under the plan for a maximum of 36 months. A qualified beneficiary must notify the plan administrator of a qualifying event within 60 days after divorce or legal separation.
Florida COBRA insurance isn't much different from other states. If you were a full-time or part-time employee, you should be eligible to receive Florida COBRA healthcare coverage. Keep in mind that your eligibility must also meet other criteria such as plan coverage, qualifying events, and eligible beneficiaries.
What is state continuation? State law allows employees of smaller employers (fewer than 20 employees) to keep the same group health insurance coverage for up to nine months after loss of a job or loss of coverage because of a reduction in work hours. This is called state continuation.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) Passed in 1985, COBRA is a federal law that allows employees of certain companies to continue their health insurance with the same benefits even after they stop working for their employer.
Florida's state continuation or mini-COBRA law provides similar continuation of coverage protection for employees who work for employers with two to 19 employees. Once you elect mini-COBRA coverage, you will pay 100% of the total insurance premium plus a 15% processing fee.