Title: Georgia Summary of Rights and Obligations under COBRA: A Comprehensive Guide Introduction: In Georgia, individuals covered by the Consolidated Omnibus Budget Reconciliation Act (COBRA) enjoy certain rights and obligations. This guide provides a detailed description of the Georgia Summary of Rights and Obligations under COBRA, including key information and relevant keywords for different types of coverage. Key Points: 1. Understanding COBRA: COBRA is a federal law that allows eligible employees and their dependents to continue their group health insurance coverage for a limited time after certain qualifying events, such as job loss, reduction in work hours, or other life events that result in a loss of coverage. 2. Eligibility for COBRA: To qualify for COBRA coverage in Georgia, individuals must have been covered under a group health plan provided by their employer before the qualifying event occurred. Employers with 20 or more employees are generally required to offer COBRA coverage. 3. Georgia COBRA Continuation Coverage: Georgia follows the federal COBRA regulations, and the Georgia Department of Insurance provides resources and support to ensure compliance. Employees have the right to elect COBRA coverage if they lose their job-based health insurance, ensuring continuity of comprehensive healthcare. 4. Types of Georgia COBRA Coverage: a) Individual Coverage: This type of coverage applies to employees who experience job loss or reduction in work hours that leads to a loss of employer-provided health insurance. Individuals may elect to continue their coverage for up to 18 months. b) Dependent Coverage: Dependents of employees who qualify for COBRA due to job loss or reduction in work hours may also be eligible for extended coverage. Dependents have the right to continue their coverage for up to 36 months. 5. Rights and Obligations of Qualified Individuals: a) Right to Continue Coverage: Qualified individuals have the right to continue their health insurance coverage under the group plan, albeit at their own expense. They must be provided with the same benefits as those available to similarly situated employees. b) Notification and Election Period: Employers must provide timely notification about COBRA rights and the election process. Qualified individuals have 60 days to decide whether to elect COBRA coverage. c) Premium Payments: Individuals who elect COBRA coverage are responsible for paying premiums, including any administrative fees. Late payments may lead to loss of coverage. d) Coverage Termination: COBRA coverage can be terminated if the qualified individual becomes eligible for another group health plan, Medicare, or fails to make timely premium payments. Conclusion: Understanding the Georgia Summary of Rights and Obligations under COBRA is essential for individuals and employers alike. By providing continued health insurance coverage, COBRA ensures that individuals have access to affordable healthcare during challenging periods. Employers must adhere to the regulations and provide comprehensive information about COBRA rights and the election process. This summary serves as an insightful resource for individuals seeking to navigate COBRA coverage options in Georgia.
Georgia Summary of Rights and Obligations under COBRA
Description
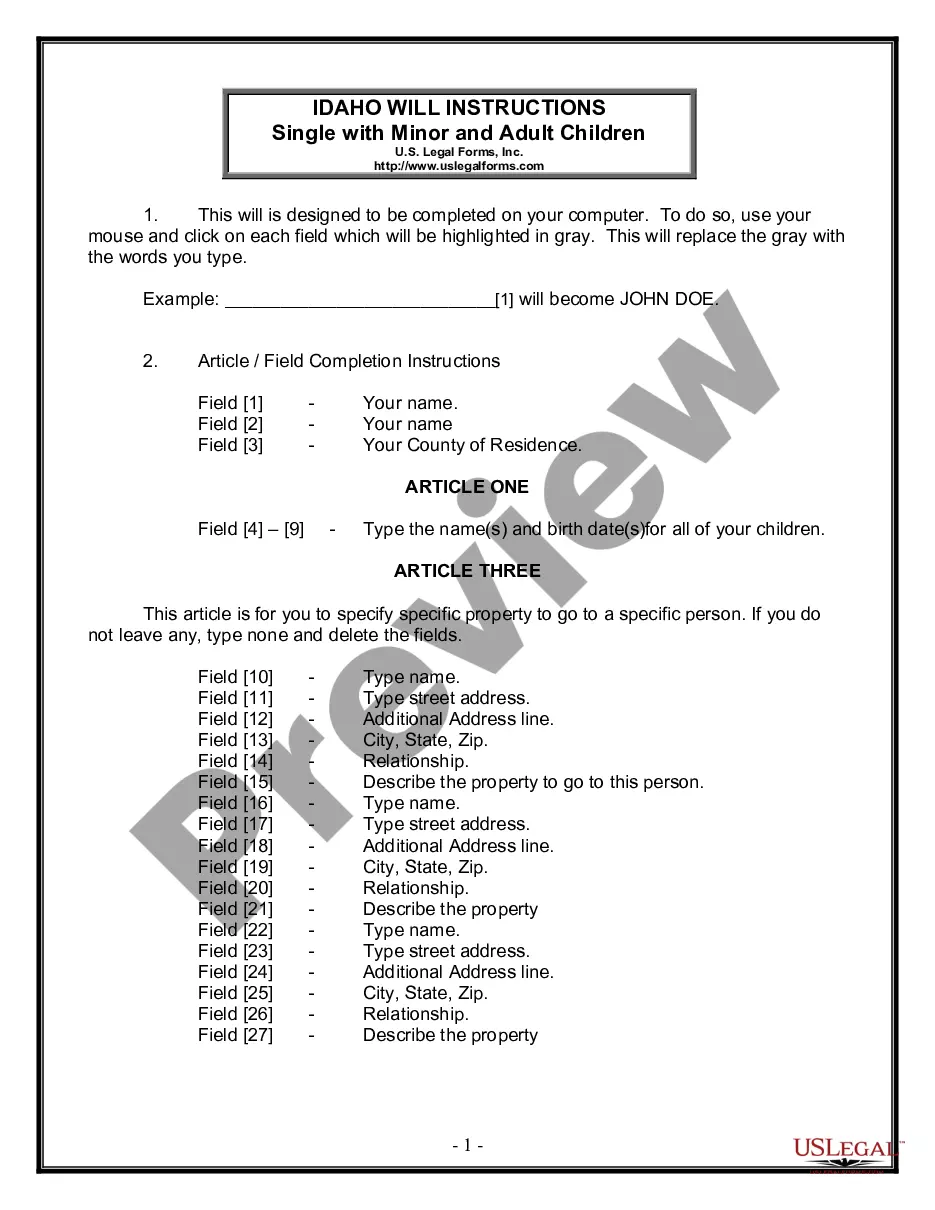
How to fill out Georgia Summary Of Rights And Obligations Under COBRA?
Finding the right legitimate document web template might be a have a problem. Naturally, there are a variety of templates available on the Internet, but how do you get the legitimate develop you will need? Utilize the US Legal Forms website. The service delivers 1000s of templates, including the Georgia Summary of Rights and Obligations under COBRA, that you can use for company and personal requirements. Every one of the kinds are inspected by professionals and fulfill federal and state requirements.
Should you be previously authorized, log in for your account and click on the Acquire switch to find the Georgia Summary of Rights and Obligations under COBRA. Use your account to look through the legitimate kinds you may have acquired formerly. Go to the My Forms tab of your respective account and have yet another copy from the document you will need.
Should you be a fresh customer of US Legal Forms, allow me to share straightforward guidelines that you can stick to:
- First, ensure you have chosen the correct develop to your metropolis/county. You are able to check out the form using the Preview switch and read the form description to make certain it is the best for you.
- In the event the develop fails to fulfill your preferences, take advantage of the Seach discipline to discover the proper develop.
- Once you are certain that the form would work, click the Purchase now switch to find the develop.
- Select the prices strategy you need and type in the essential info. Design your account and buy the order making use of your PayPal account or charge card.
- Pick the document file format and down load the legitimate document web template for your device.
- Total, revise and printing and indication the attained Georgia Summary of Rights and Obligations under COBRA.
US Legal Forms will be the greatest library of legitimate kinds in which you can find a variety of document templates. Utilize the company to down load professionally-created documents that stick to condition requirements.
Form popularity
FAQ
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
When the covered employee's employment is terminated (for reasons other than gross misconduct) or reduction in work hours, qualified beneficiaries must be eligible for 18 months of continuation coverage. Your group health plan can require you to pay for COBRA continuation coverage.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
Georgia and the COBRA Insurance Act. The Federal Consolidated Omnibus Budget Reconciliation Act (COBRA) allows retiring employees, or those who lose coverage due to quitting a job or reduced work hours, to continue group coverage for a limited period of time.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.