Georgia Certificate of Group Health Plan Coverage
Description
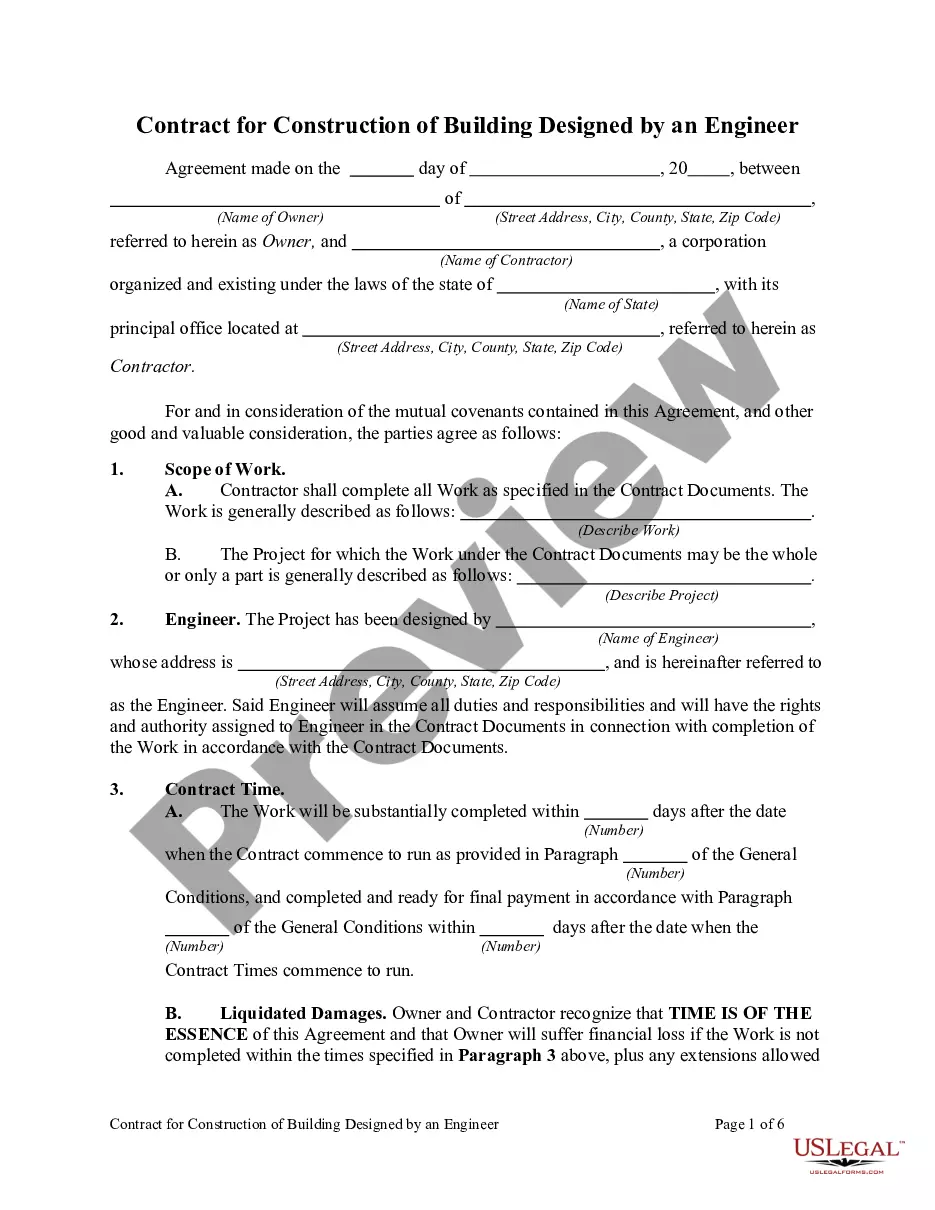
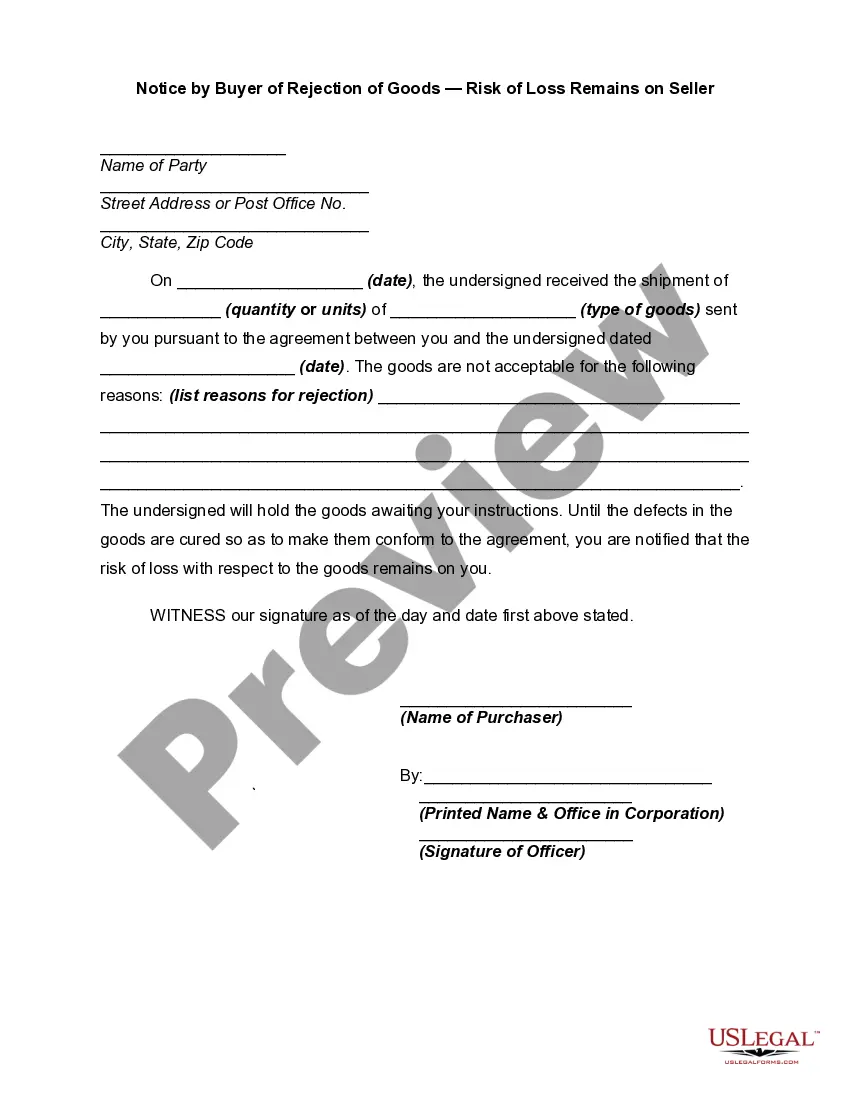
How to fill out Certificate Of Group Health Plan Coverage?
You can devote time on the Internet looking for the legitimate file design that fits the federal and state needs you require. US Legal Forms gives a large number of legitimate varieties that are evaluated by specialists. It is simple to obtain or print the Georgia Certificate of Group Health Plan Coverage from the services.
If you already possess a US Legal Forms account, you can log in and then click the Download option. After that, you can comprehensive, modify, print, or signal the Georgia Certificate of Group Health Plan Coverage. Every legitimate file design you purchase is yours permanently. To have yet another copy associated with a purchased develop, check out the My Forms tab and then click the corresponding option.
If you are using the US Legal Forms website initially, follow the basic directions below:
- Initially, make certain you have chosen the correct file design for the county/metropolis of your choosing. Read the develop description to make sure you have chosen the correct develop. If offered, make use of the Preview option to check from the file design too.
- If you wish to locate yet another model of your develop, make use of the Lookup industry to find the design that meets your needs and needs.
- Upon having found the design you desire, simply click Get now to move forward.
- Select the rates prepare you desire, type your references, and sign up for an account on US Legal Forms.
- Total the purchase. You can use your credit card or PayPal account to pay for the legitimate develop.
- Select the structure of your file and obtain it for your device.
- Make modifications for your file if necessary. You can comprehensive, modify and signal and print Georgia Certificate of Group Health Plan Coverage.
Download and print a large number of file templates making use of the US Legal Forms web site, which provides the biggest collection of legitimate varieties. Use professional and express-specific templates to deal with your small business or person demands.
Form popularity
FAQ
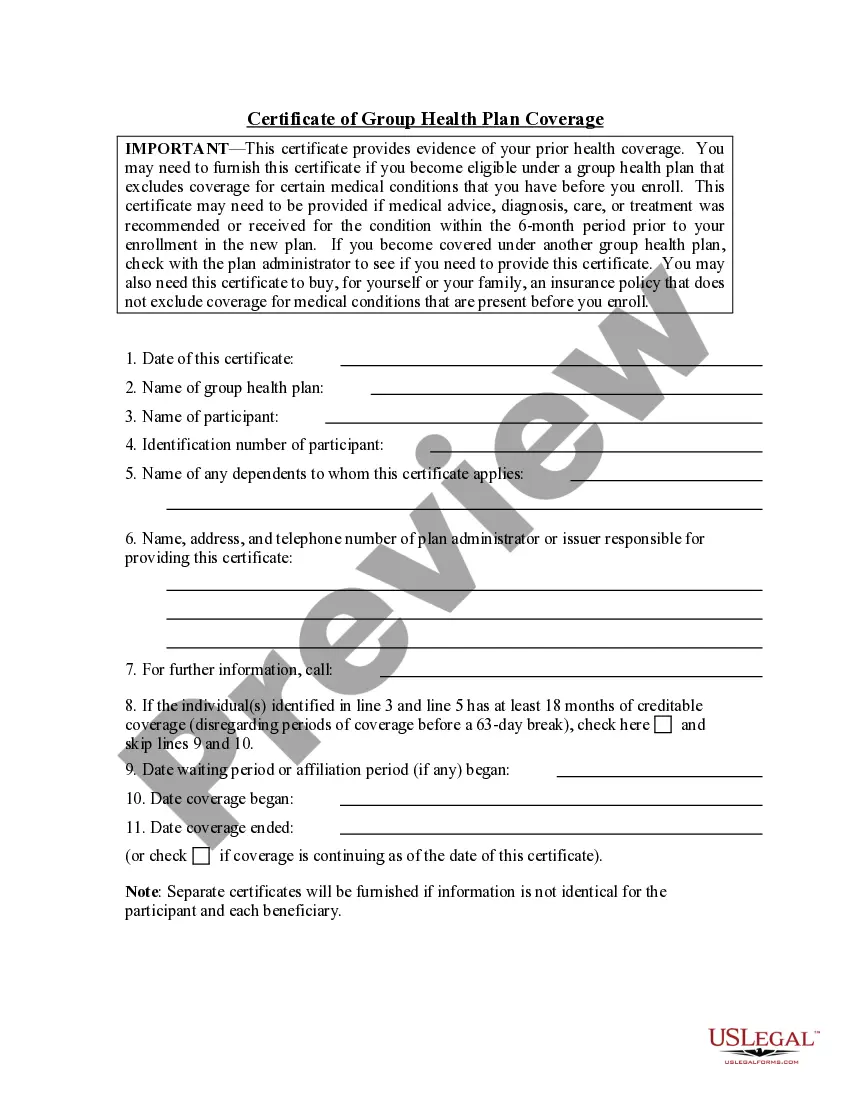
Groups must have at least two employees to be eligible for group insurance coverage. Group health insurance policy rates are usually based on: Group health insurance policy rates are usually based on experience rating in which premiums are based on the claims experience of the entire group.
Employees who elect coverage through the group policy usually receive a certificate of coverage, which is needed to provide to a subsequent insurance company in the event that an individual leaves the company or organization and terminates their coverage.
The certificate of creditable coverage is intended to establish an individual's prior creditable coverage for purposes of reducing the extent to which a plan or issuer offering health insurance coverage in the group market can apply a preexisting condition exclusion.
A certificate of coverage (CoC) is a contract that lists an individual's health insurance coverage with their payor.
The request should be made on the CON Request for Determination form, which can be obtained at .dch.georgia.gov. The form should also include as much information about the project as possible. There is a filing fee of $250 for a determination request. The Department will respond in writing.
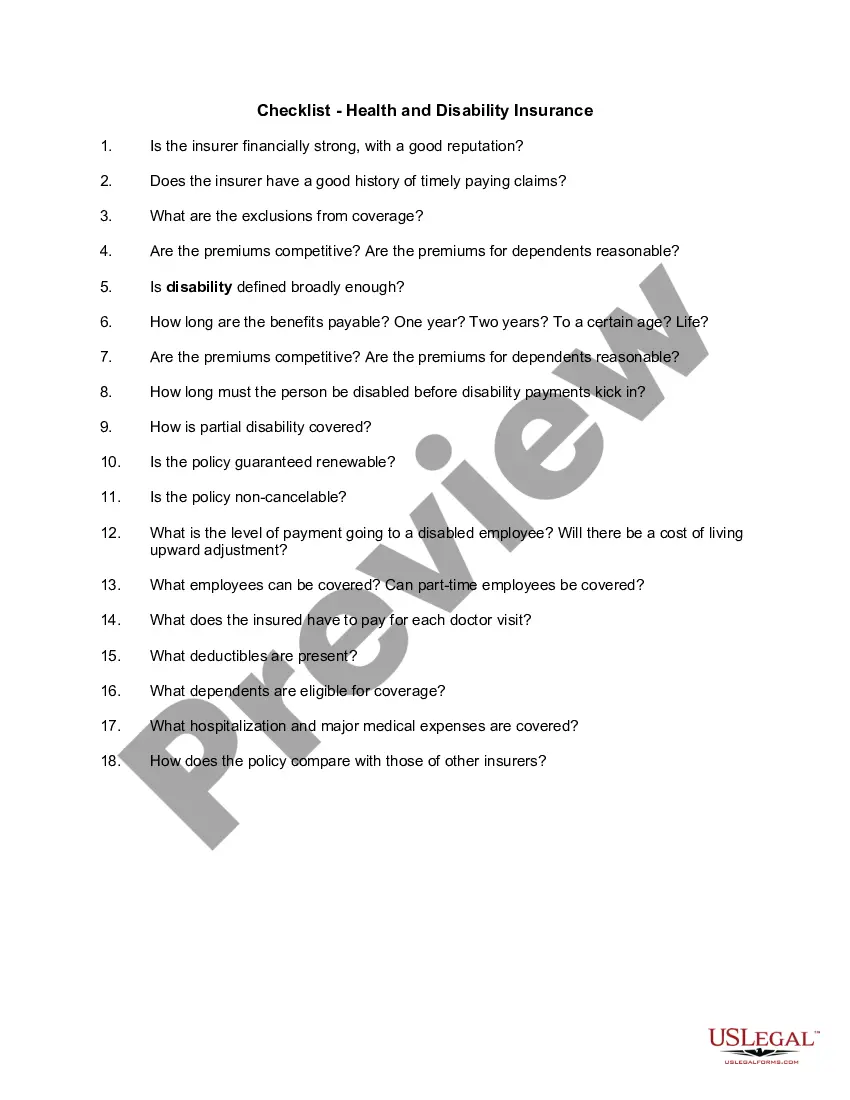
This document explains the health benefits you and your dependents have under the plan. It details the services that will and will not be covered. Services that are not covered are called exclusions.
Which of the following is NOT required in the Outline of Coverage for a health insurance policy? "Projection of the policy's future costs". A table indicating the policy's projected future costs is not required in an Outline of Coverage.
Typically, each insured member of the group receives a certificate of insurance. This certificate states that the insured member of the group is covered under the master contract held by the employer. Also, the provisions of the group insurance are usually stated in the certificate of insurance.