Georgia General Notice of Preexisting Condition Exclusion
Description
How to fill out General Notice Of Preexisting Condition Exclusion?
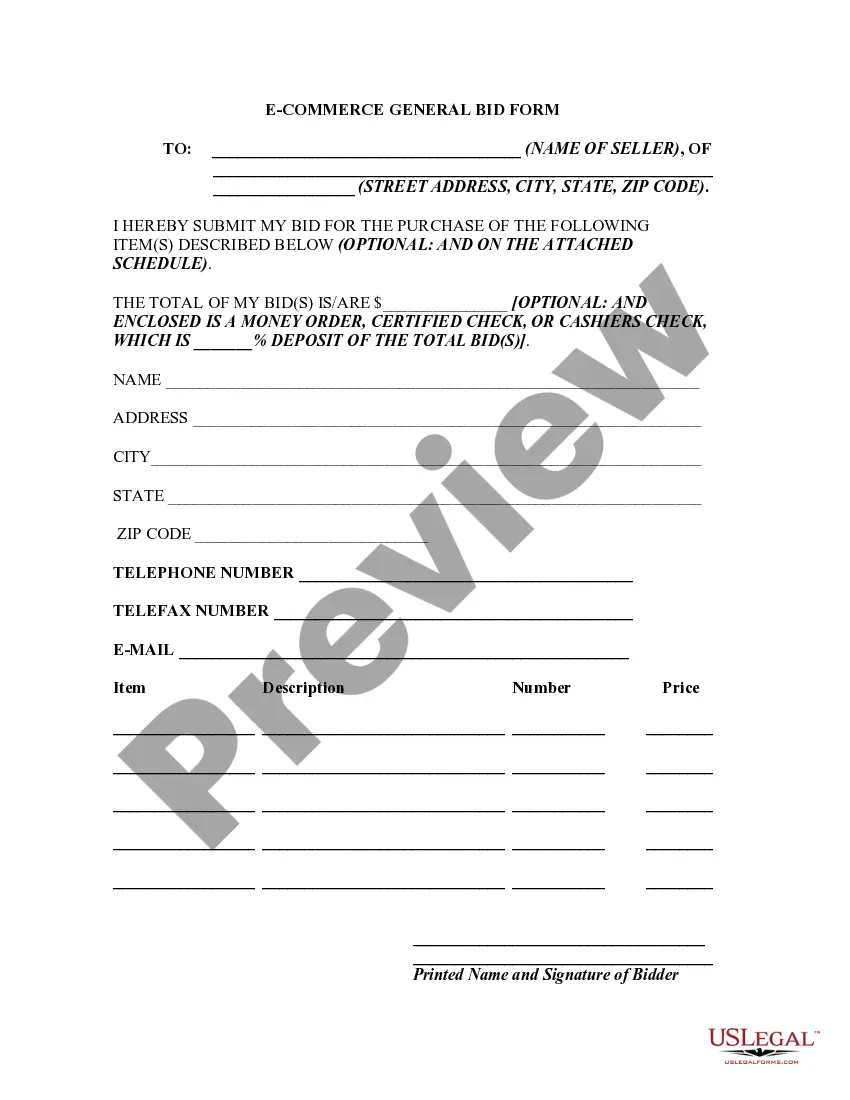
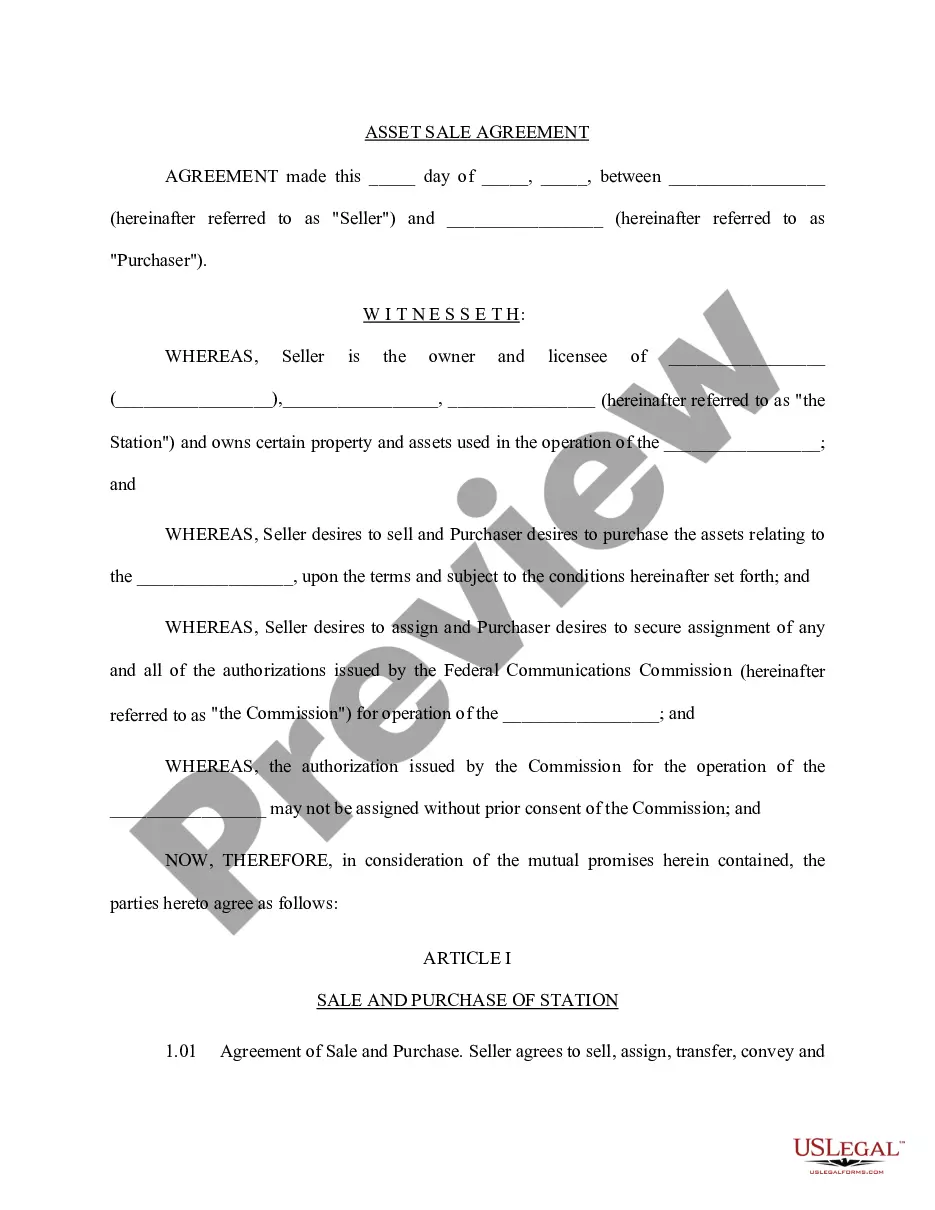
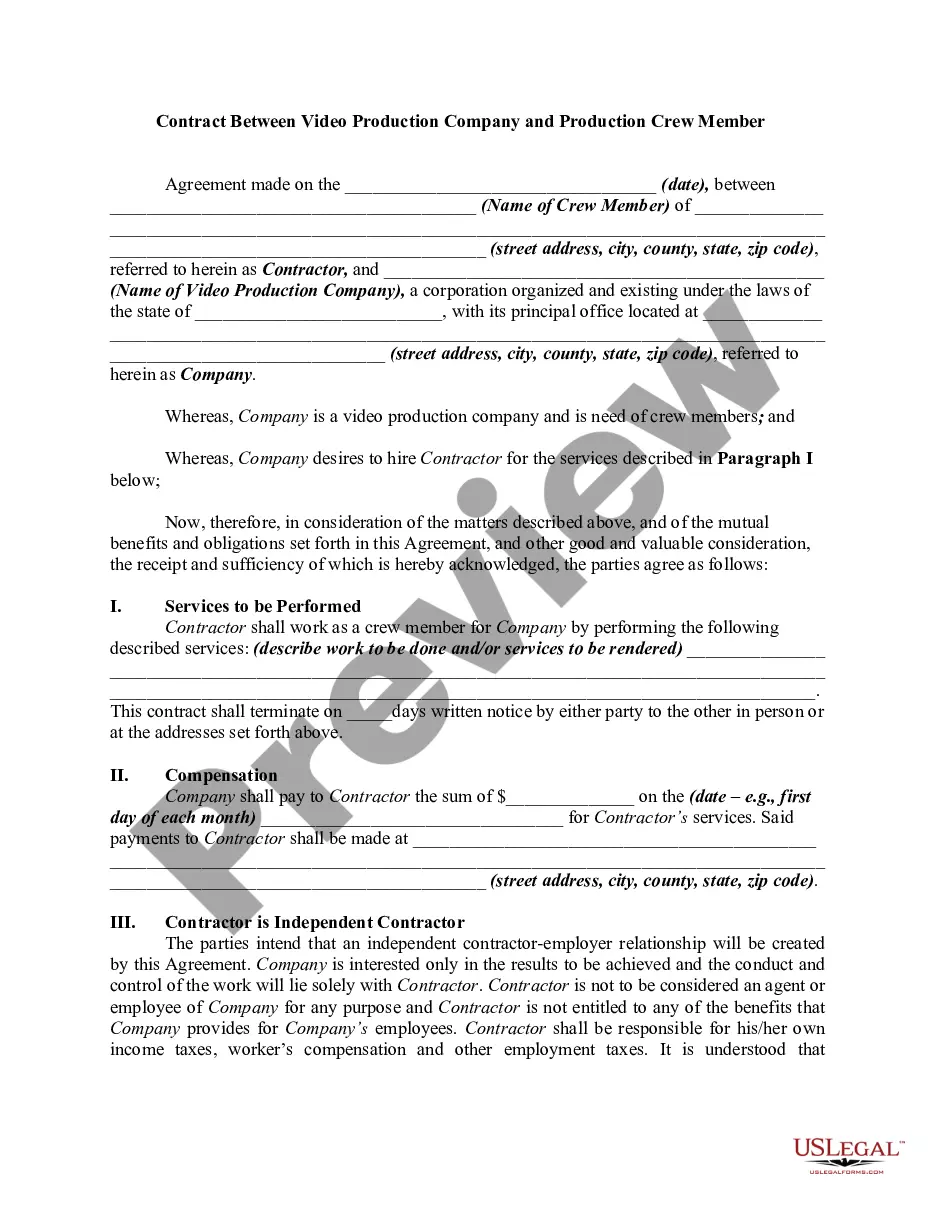
You might spend time online trying to locate the official document template that meets the state and federal requirements you need.
US Legal Forms offers thousands of legal templates that are reviewed by experts.
You can easily obtain or print the Georgia General Notice of Preexisting Condition Exclusion from the service.
If available, utilize the Review button to look through the document template as well.
- If you already have a US Legal Forms account, you can Log In and then click the Download button.
- Afterward, you can complete, modify, print, or sign the Georgia General Notice of Preexisting Condition Exclusion.
- Every legal document template you receive is yours permanently.
- To acquire another copy of a purchased form, visit the My documents tab and click the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, make sure you have chosen the correct document template for the region/area you select.
- Review the template details to ensure you have selected the right form.
Form popularity
FAQ
The term pre-existing condition exclusion 3 12 indicates a waiting period of three months for a pre-existing condition in a health insurance policy. During these first three months, any medical issues that existed before your coverage begins are not eligible for benefits. After this waiting period, the conditions are generally covered according to the policy limits. It's crucial to refer to the Georgia General Notice of Preexisting Condition Exclusion for further clarity on how this impacts your coverage.
existing condition exclusion for disability insurance means that if you have a health issue prior to obtaining coverage, that condition may not be covered during the policy period. This exclusion aims to limit the risk for insurers when offering policies. The Georgia General Notice of Preexisting Condition Exclusion helps clarify these terms, allowing potential policyholders to understand their rights and obligations. Always check your policy for specific details on exclusions.
In Georgia, pre-existing condition health insurance refers to coverage that takes into account an individual's existing medical conditions when evaluating eligibility for health insurance. Under Georgia General Notice of Preexisting Condition Exclusion, insurers may impose waiting periods before covering these conditions. Understanding this helps you make informed decisions about your health insurance options. It's essential to review your policy details to ensure adequate coverage.
The exclusion period for pre-existing conditions often lasts for a specified time, frequently ranging from six months to a year after your policy starts. The Georgia General Notice of Preexisting Condition Exclusion outlines these details, so reviewing it can clarify any doubts. It’s important to know what your policy states, as understanding these timelines allows you to plan your healthcare accordingly. If you have questions, consider reaching out through platforms like uslegalforms for guidance on your specific situation.
Typically, a pre-existing condition can refer to any health issue that was diagnosed or treated prior to the start of your health insurance coverage. The timeframe may vary depending on your specific insurance provider and their incorporation of the Georgia General Notice of Preexisting Condition Exclusion. In most cases, insurers look back six months to a year, but it's crucial to be aware of your particular policy terms. Taking the time to review your health history with your insurance can make a significant difference in your coverage options.
existing condition exclusion refers to the practice of denying coverage for health issues that were present before the start of an insurance policy. With the Georgia General Notice of Preexisting Condition Exclusion, you can better grasp how your previous conditions might impact your insurance. This knowledge enables you to prepare effectively when choosing a health plan that meets your needs. Always consult your policy to fully understand how these exclusions apply to you.
The pre-existing exclusion clause is a provision in health insurance policies that limits or excludes coverage for conditions that existed before the policy began. Understanding the Georgia General Notice of Preexisting Condition Exclusion helps you navigate these clauses. By knowing how these exclusions work, you can make informed decisions about your healthcare coverage. It’s essential to review your policy details to understand what this means for your health needs.
You can navigate around pre-existing conditions by exploring options like group health insurance or applying during open enrollment periods. Additionally, understanding the provisions of the Georgia General Notice of Preexisting Condition Exclusion can help you find plans that minimize waiting periods. Utilizing resources like USLegalForms can provide valuable insights and tools to guide your search for a suitable health insurance plan.
The 33 3 28 law in Georgia refers to specific timeframes for insurers concerning pre-existing conditions. It states that if you have had prior health insurance, your waiting period for coverage on pre-existing conditions must not exceed 33 days. This provision is designed to protect consumers from extended exclusions and ensures you receive coverage sooner.