Hawaii Individual Notice of Preexisting Condition Exclusion
Description
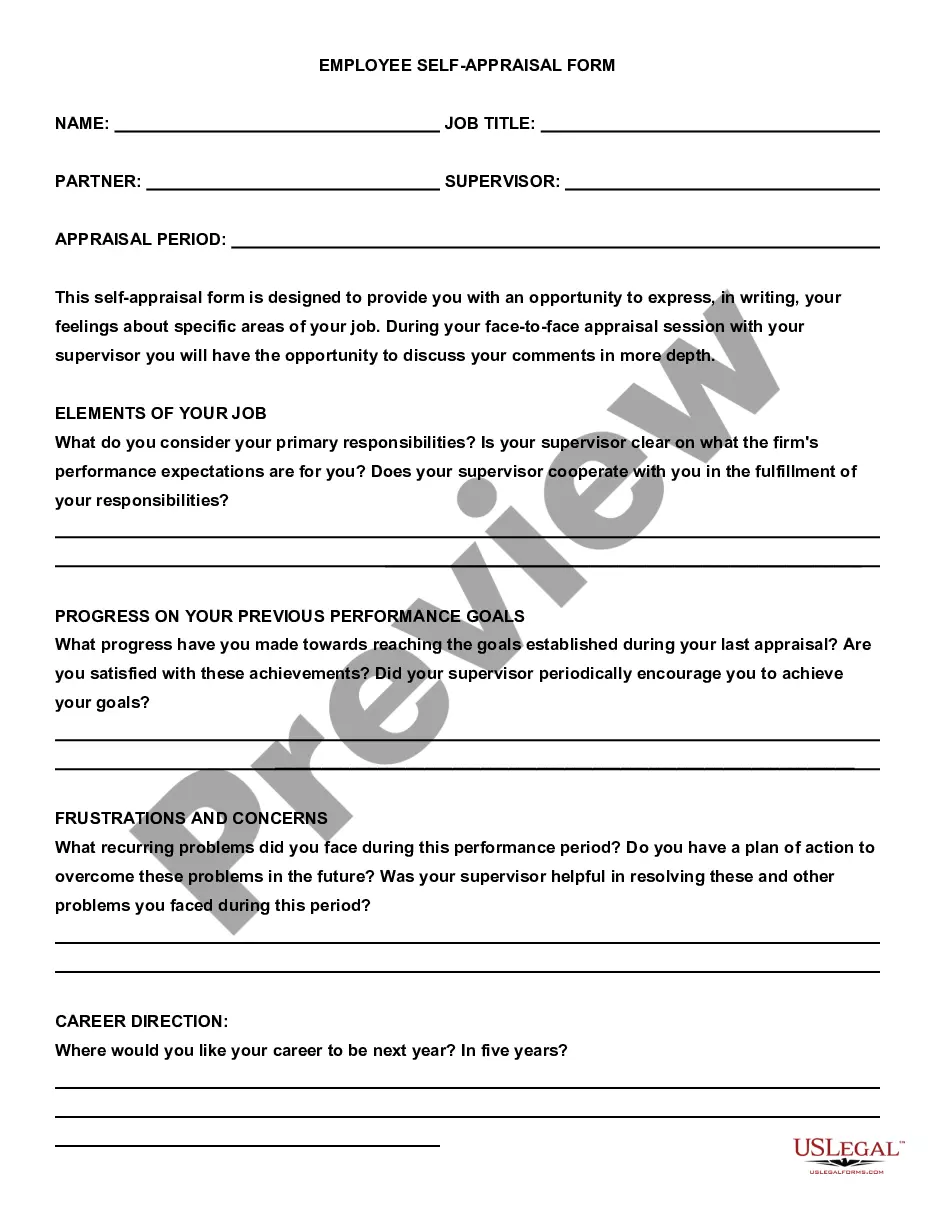
How to fill out Individual Notice Of Preexisting Condition Exclusion?
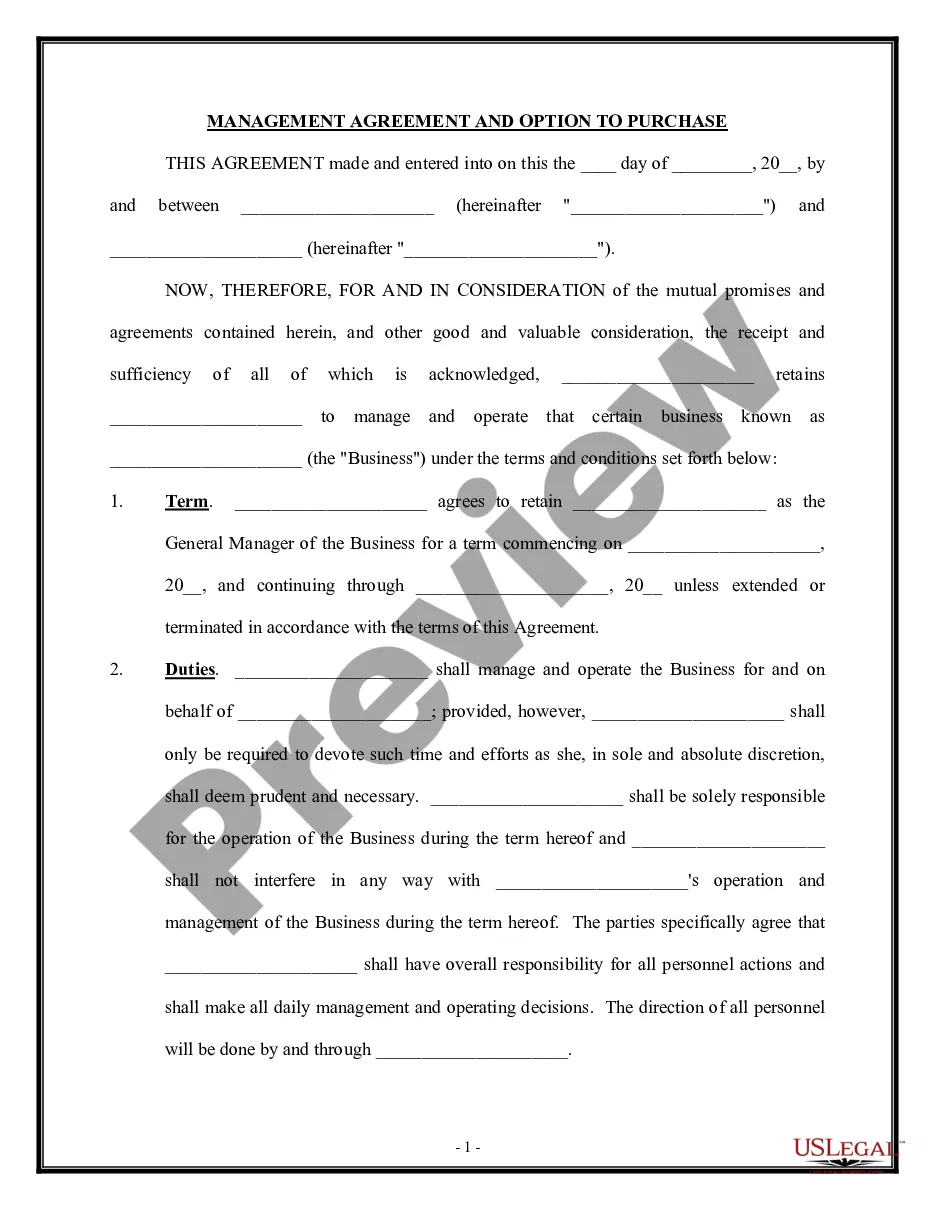
It is possible to invest several hours online searching for the legitimate record design that meets the state and federal specifications you want. US Legal Forms gives a huge number of legitimate forms which are analyzed by pros. You can easily down load or printing the Hawaii Individual Notice of Preexisting Condition Exclusion from the services.
If you already possess a US Legal Forms account, it is possible to log in and click the Download key. Following that, it is possible to full, change, printing, or signal the Hawaii Individual Notice of Preexisting Condition Exclusion. Each and every legitimate record design you acquire is yours for a long time. To have yet another copy associated with a bought form, proceed to the My Forms tab and click the related key.
If you work with the US Legal Forms internet site the very first time, stick to the simple recommendations listed below:
- Initially, make sure that you have chosen the proper record design to the state/metropolis of your liking. Read the form description to ensure you have selected the appropriate form. If readily available, make use of the Preview key to appear with the record design also.
- If you want to discover yet another model in the form, make use of the Look for industry to get the design that meets your requirements and specifications.
- Upon having discovered the design you need, just click Purchase now to proceed.
- Pick the costs strategy you need, enter your qualifications, and register for your account on US Legal Forms.
- Full the purchase. You may use your bank card or PayPal account to pay for the legitimate form.
- Pick the file format in the record and down load it for your product.
- Make alterations for your record if necessary. It is possible to full, change and signal and printing Hawaii Individual Notice of Preexisting Condition Exclusion.
Download and printing a huge number of record themes making use of the US Legal Forms site, which provides the biggest selection of legitimate forms. Use expert and status-particular themes to handle your company or person demands.
Form popularity
FAQ
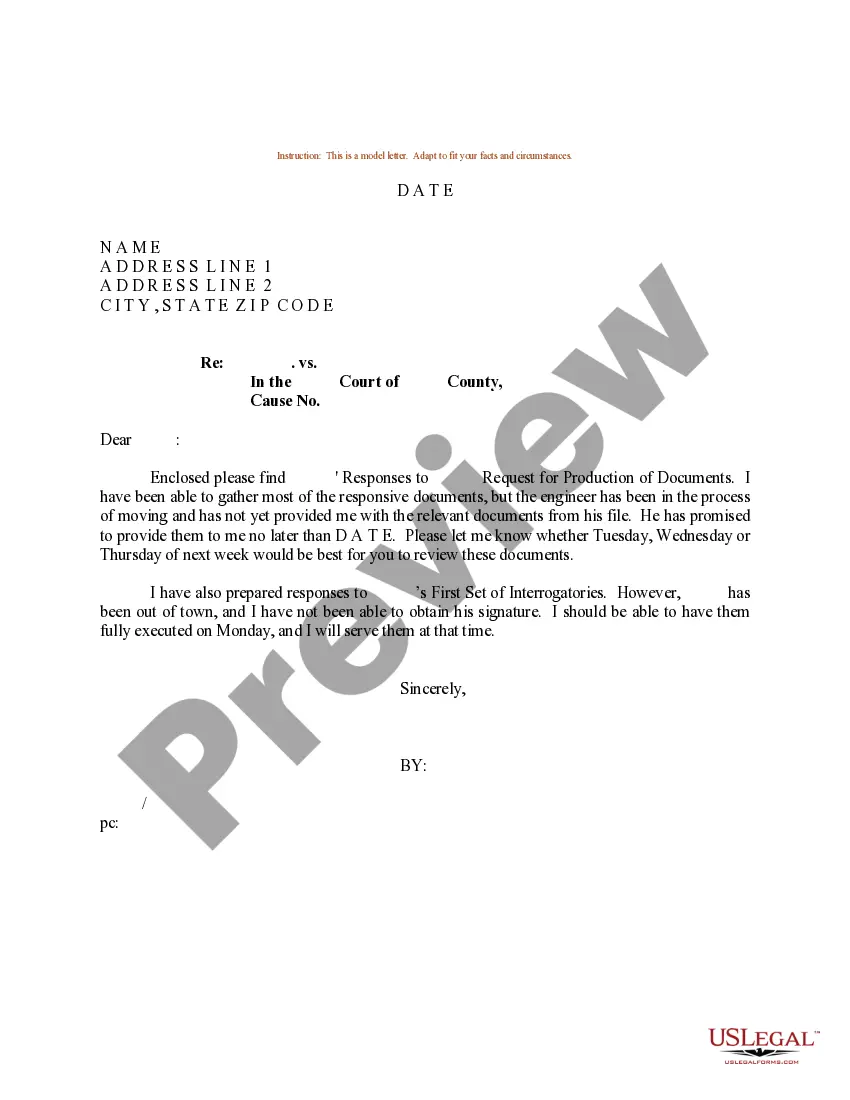
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.
The time period during which an individual policy won't pay for care relating to a pre-existing condition. Under an individual policy, conditions may be excluded permanently (known as an "exclusionary rider").
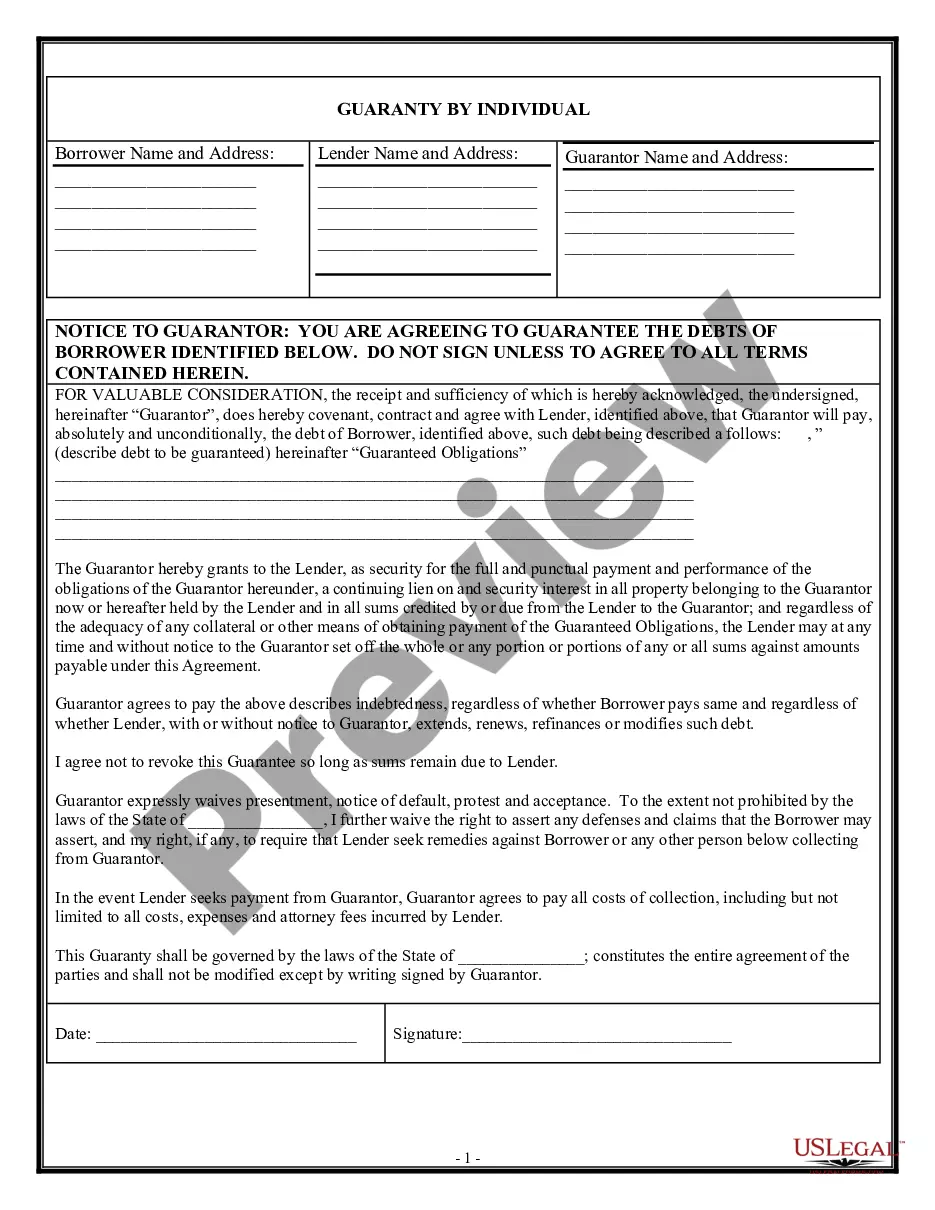
There might be a scenario's where system determines records for more than one condition type in the pricing procedure. In order to avoid this we can set up conditions or a group of conditions to be mutually exclusive. This is called condition exclusion.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
A medical illness or injury that you have before you start a new health care plan may be considered a pre-existing condition. Conditions like diabetes, COPD, cancer, and sleep apnea, may be examples of pre-existing health conditions. They tend to be chronic or long-term.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Examples of pre-existing conditions include cancer, asthma, diabetes, and even pregnancy. Under the Affordable Care Act (Obamacare), health insurance companies cannot refuse to cover you because of any pre-existing conditions nor can they charge you more money for coverage or subject you to a waiting period.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.