Title: Idaho Sample COBRA Enrollment and/or Waiver Letter: Comprehensive Guide Introduction: In this detailed guide, we will provide you with a comprehensive description of Idaho's sample COBRA (Consolidated Omnibus Budget Reconciliation Act) Enrollment and/or Waiver Letter. COBRA is a federal law that allows eligible employees and their dependents to continue receiving health insurance coverage after certain qualifying events, such as job loss or reduced work hours. Overview of Idaho Sample COBRA Enrollment and/or Waiver Letter: Idaho's sample COBRA Enrollment and/or Waiver Letter serves as a template for employers to communicate necessary information to individuals regarding their COBRA rights and options. These letters play a crucial role in ensuring individuals understand their health insurance options and are given the opportunity to enroll or waive COBRA coverage within the specified time frame. Types of Idaho Sample COBRA Enrollment and/or Waiver Letters: 1. Idaho Initial COBRA Enrollment Letter: This letter is issued to eligible individuals who have experienced a qualifying event, notifying them about their COBRA eligibility and providing important details related to enrollment. It outlines the specific rights, deadlines, and requirements to elect COBRA coverage. 2. Idaho COBRA Enrollment Extension Letter: In certain situations, an extended COBRA enrollment period might be offered to eligible individuals due to specific circumstances, such as a delay in receiving initial notification. The COBRA Enrollment Extension Letter informs recipients about the extended deadline and provides instructions regarding the enrollment process. 3. Idaho COBRA Coverage Waiver Letter: This letter is sent to eligible individuals who have the option to waive their COBRA coverage. It explains the implications of waiving coverage, acknowledges their decision to decline COBRA benefits, and indicates that they will not be eligible for COBRA coverage in the future. Key Components of Idaho Sample COBRA Enrollment and/or Waiver Letter: 1. Introduction and Purpose: The letter begins with a clear introduction, explaining that it is a COBRA Enrollment and/or Waiver Letter and its purpose of informing recipients about their rights and options. 2. Qualifying Event Details: The letter provides a concise description of the qualifying event that makes individuals eligible for COBRA coverage, such as job termination, reduction in work hours, or certain life events like divorce or death of a covered employee. 3. COBRA Continuation Period: It informs recipients about the duration of coverage they can receive under COBRA, typically spanning 18 months from the date of the qualifying event. For some qualifying events, such as disability, the coverage period may be extended. 4. Enrollment Information: The letter includes clear instructions on how to enroll in COBRA coverage, specifying the necessary forms, contact information of the employer or plan administrator, and the deadline for submitting the enrollment application. 5. Premium Payment Details: It explains the COBRA premium costs, payment methods, due dates, and consequences of late payments. 6. Coverage Details and Limitations: The letter outlines the benefits, coverage limitations, and conditions that apply specifically to COBRA participants, such as maintaining coverage while outside the plan's service area. Conclusion: Idaho's sample COBRA Enrollment and/or Waiver Letter serves as a vital tool to ensure eligible individuals have a comprehensive understanding of their COBRA coverage rights and options. This detailed description has provided an overview of the different types of Idaho's sample COBRA Enrollment and/or Waiver Letters, highlighting the key components included in these communications. By leveraging this information, employers can effectively communicate COBRA-related details to their employees and dependents, enabling them to make informed decisions regarding their healthcare coverage.
Idaho Sample COBRA Enrollment and / or Waiver Letter
Description
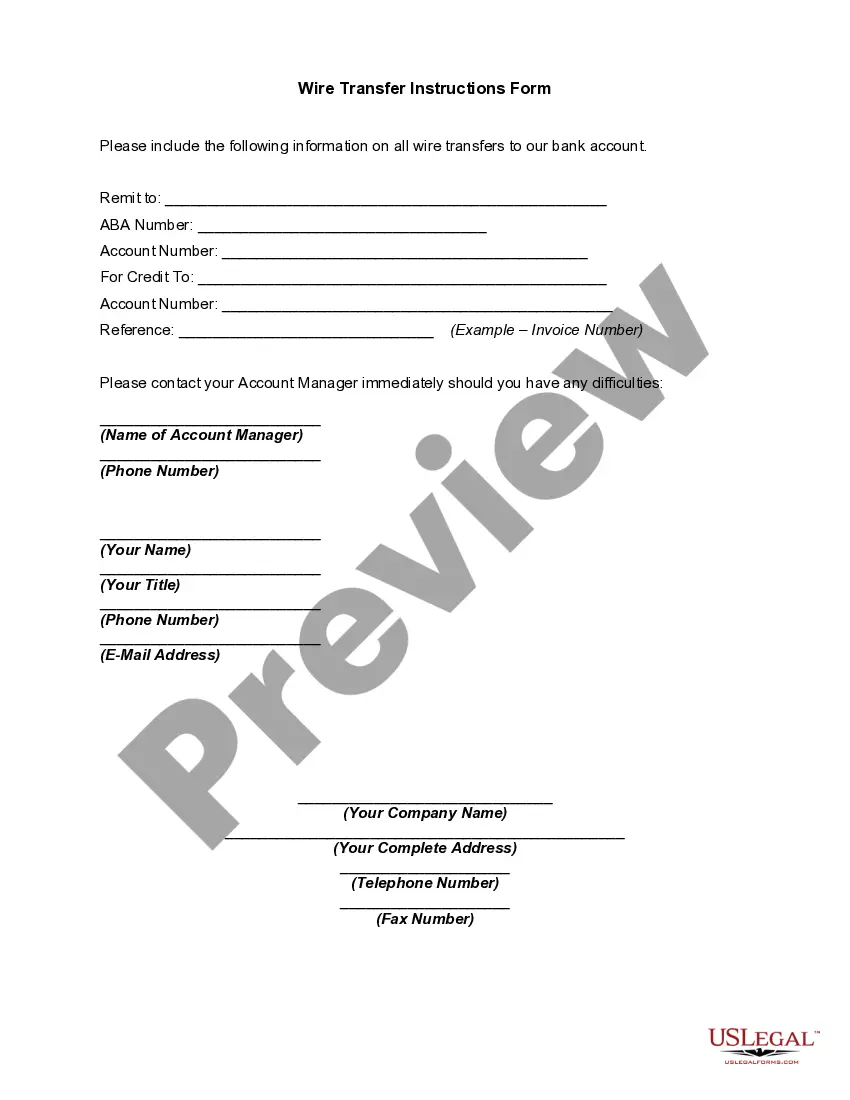
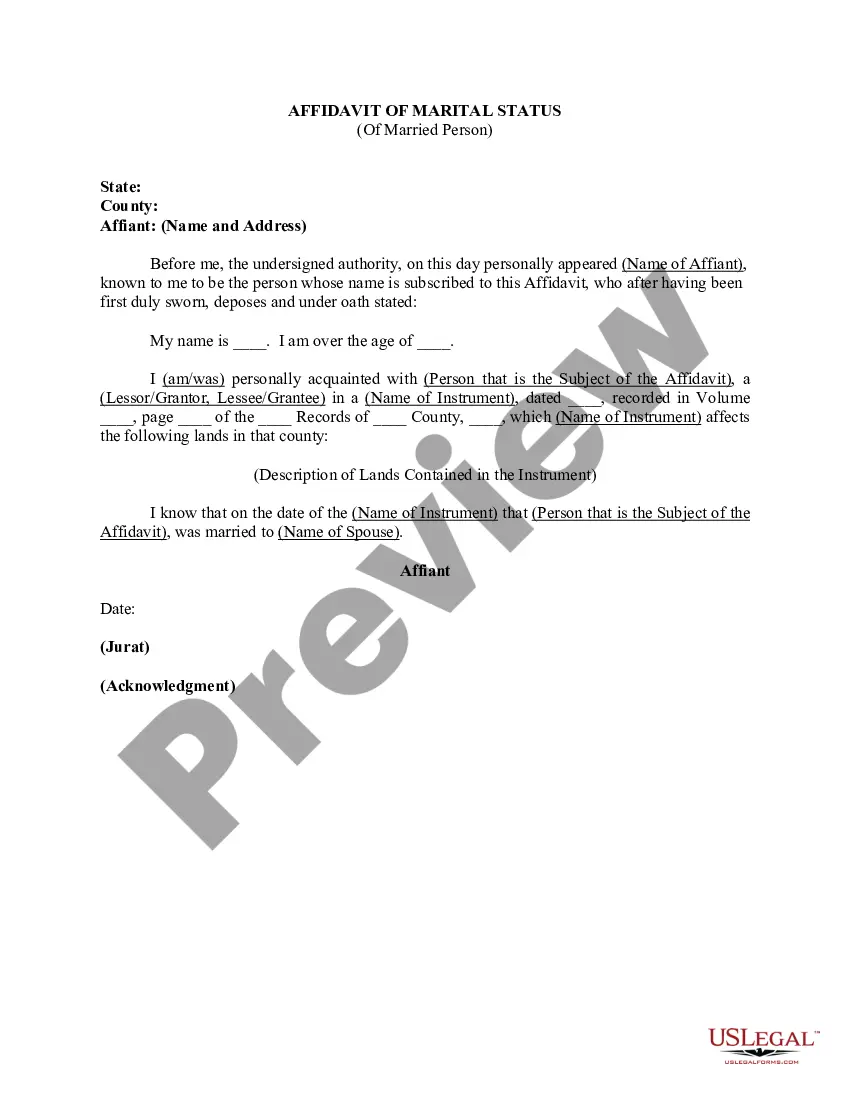
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
If you want to complete, obtain, or print legal record web templates, use US Legal Forms, the biggest variety of legal forms, which can be found online. Take advantage of the site`s easy and hassle-free look for to get the files you require. Various web templates for business and specific purposes are categorized by classes and claims, or keywords. Use US Legal Forms to get the Idaho Sample COBRA Enrollment and / or Waiver Letter in a handful of click throughs.
When you are presently a US Legal Forms consumer, log in to your bank account and click on the Down load switch to get the Idaho Sample COBRA Enrollment and / or Waiver Letter. You may also accessibility forms you in the past downloaded within the My Forms tab of your own bank account.
If you use US Legal Forms the first time, refer to the instructions listed below:
- Step 1. Be sure you have selected the form for your right metropolis/region.
- Step 2. Make use of the Preview option to examine the form`s content material. Never neglect to read the information.
- Step 3. When you are not satisfied with the type, utilize the Research industry on top of the display screen to get other types from the legal type format.
- Step 4. When you have found the form you require, select the Purchase now switch. Pick the rates strategy you prefer and add your accreditations to sign up to have an bank account.
- Step 5. Procedure the financial transaction. You can utilize your charge card or PayPal bank account to accomplish the financial transaction.
- Step 6. Choose the format from the legal type and obtain it on your own gadget.
- Step 7. Comprehensive, revise and print or indicator the Idaho Sample COBRA Enrollment and / or Waiver Letter.
Every single legal record format you acquire is the one you have eternally. You have acces to each and every type you downloaded with your acccount. Select the My Forms segment and decide on a type to print or obtain again.
Compete and obtain, and print the Idaho Sample COBRA Enrollment and / or Waiver Letter with US Legal Forms. There are many specialist and status-distinct forms you can use for the business or specific needs.
Form popularity
FAQ
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA is an acronym for the Consolidated Omnibus Budget Reconciliation Act, which provides eligible employees and their dependents the option of continued health insurance coverage when an employee loses their job or experiences a reduction of work hours.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.