Illinois Notice of Special Enrollment Rules refers to the specific regulations and guidelines that govern the special enrollment periods (SEPs) available to Illinois residents who wish to enroll in or make changes to their health insurance coverage outside the yearly open enrollment period. These SEPs provide individuals with the opportunity to sign up for or modify their health insurance coverage due to certain qualifying life events. Under the Illinois Notice of Special Enrollment Rules, there are several types of SEPs available to eligible individuals. Some common types of SEPs include: 1. Loss of Qualified Health Plan (HP) Coverage: This SEP is applicable when an individual loses their current health insurance coverage, such as job-based coverage, due to reasons such as termination of employment, divorce, or aging out of a dependent's plan. 2. Permanent Residence in a New Service Area: Individuals who permanently move to a new region within Illinois or enter Illinois from another state may qualify for this SEP. It allows them to enroll in a health insurance plan available in their new service area. 3. Gaining or Becoming Dependent on a Qualified Individual: When a person becomes a dependent, such as through marriage, birth, adoption, or placement for adoption, they may become eligible for this SEP. It allows them to join or switch to a health insurance plan that covers their new dependent status. 4. Loss of Minimum Essential Coverage: This SEP is triggered when an individual experiences a loss of their previous minimum essential coverage, such as losing Medicaid or Children's Health Insurance Program (CHIP) eligibility. 5. Release from Incarceration: Individuals who are released from incarceration and were not previously enrolled in Medicaid or other health coverage may qualify for this SEP. It allows them to enroll in a health plan offered in Illinois. Other possible types of SEPs within the Illinois Notice of Special Enrollment Rules may include SEP for victims of domestic abuse or spousal abandonment, SEP for individuals impacted by a natural disaster, and SEP for Native Americans or Alaska Natives. It is important to familiarize oneself with the specific Illinois Notice of Special Enrollment Rules and respective qualifying life events to determine eligibility for enrollment or changes to health insurance coverage outside the regular enrollment period. These rules aim to provide necessary flexibility to individuals experiencing significant life changes and ensure access to essential healthcare services.
Illinois Notice of Special Enrollment Rules
Description
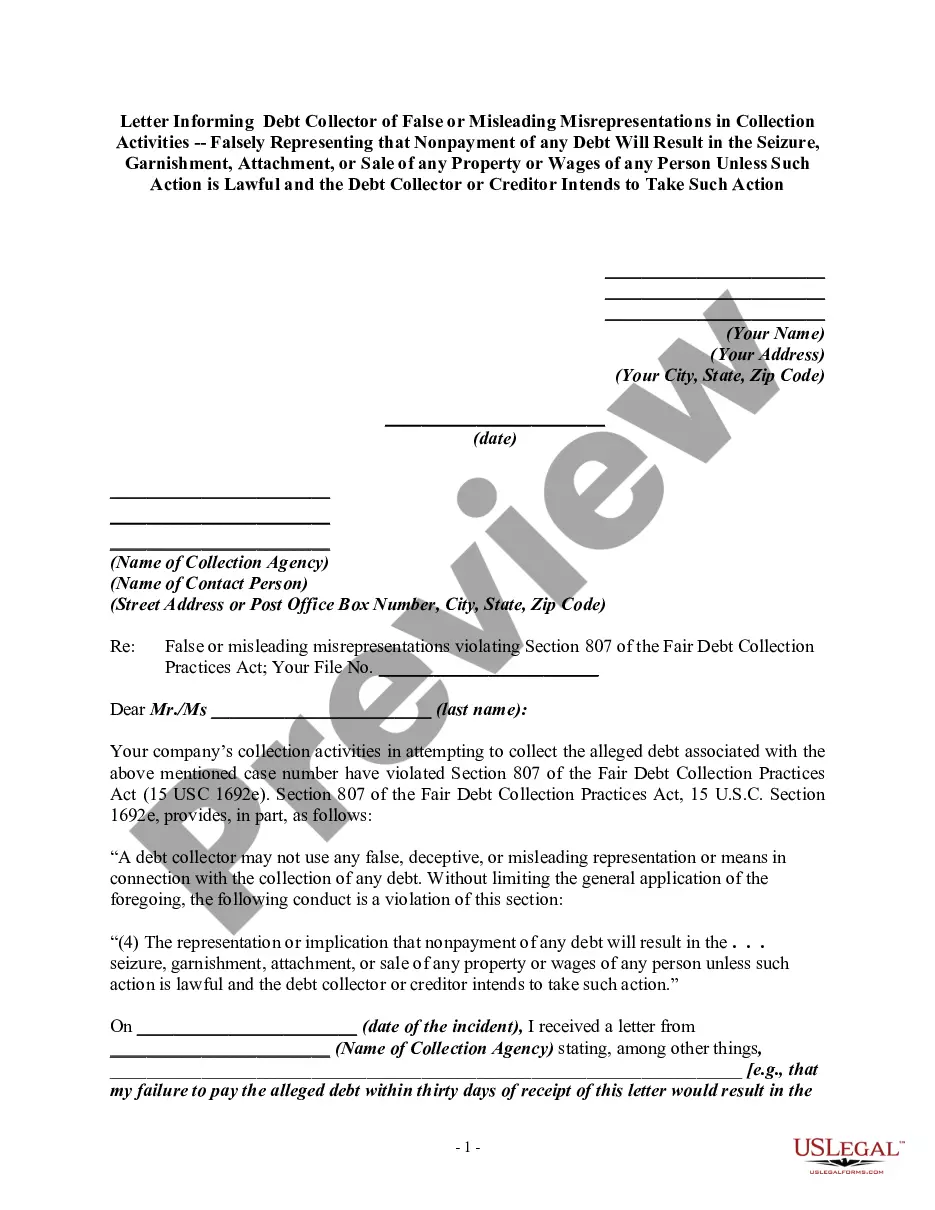
How to fill out Notice Of Special Enrollment Rules?
Are you in the place that you require documents for either organization or personal functions nearly every time? There are a variety of legal file templates available on the Internet, but getting kinds you can trust isn`t straightforward. US Legal Forms provides a huge number of form templates, such as the Illinois Notice of Special Enrollment Rules, which can be written to satisfy state and federal requirements.
If you are previously familiar with US Legal Forms site and have a merchant account, basically log in. Afterward, you may acquire the Illinois Notice of Special Enrollment Rules design.
Should you not provide an bank account and would like to begin using US Legal Forms, abide by these steps:
- Get the form you require and make sure it is for the appropriate town/state.
- Utilize the Review switch to examine the form.
- Look at the description to actually have selected the correct form.
- When the form isn`t what you`re looking for, take advantage of the Research discipline to find the form that fits your needs and requirements.
- Whenever you find the appropriate form, click Get now.
- Opt for the rates prepare you would like, complete the desired information and facts to create your money, and pay money for your order with your PayPal or bank card.
- Choose a convenient file formatting and acquire your backup.
Discover all of the file templates you possess bought in the My Forms food selection. You can obtain a additional backup of Illinois Notice of Special Enrollment Rules at any time, if necessary. Just select the needed form to acquire or print out the file design.
Use US Legal Forms, one of the most extensive assortment of legal kinds, in order to save some time and prevent mistakes. The support provides professionally produced legal file templates that can be used for a selection of functions. Produce a merchant account on US Legal Forms and commence making your daily life a little easier.
Form popularity
FAQ
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
Special enrollment periods are typically 60-days long and will allow you to purchase major medical insurance.
More Definitions of Eligible Event Eligible Event means, subject to the elections made in the Election of Coverage, the occurrence of one or more of the following: Accidental Death, death, Accidental Disability, and Total Disability.
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
Normally, coverage is only available for purchase during the annual open enrollment period, but a special enrollment period allows people to sign up for coverage outside of that annual window, as long as they have a qualifying event.
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
2022 Special Enrollment Period You have two set times each year to buy a BCBSIL health plan. One is the Open Enrollment Period (OEP), when everyone can buy a health plan. Generally, OEP is from November 1 through December 15 of the same year. This year's OEP was from November 1, 2021 January 15, 2022.
Period of enrollment means the period that the title IV institution has established for which institutional charges are generally assessed (i.e., length of the student's course, program, or academic year.)
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.