Kentucky Managed-Care Utilization Review (MCR) is a state-funded program that is designed to ensure the delivery of quality health care services while managing costs for both providers and consumers. The program is managed by the Kentucky Department of Medicaid Services (DMS). MCR is used to evaluate the appropriateness, effectiveness, and efficiency of services provided by Medicaid providers. It also helps to ensure that Medicaid members are receiving the most appropriate health care services for their needs. The two main types of Kentucky MCR are Pre-Service Utilization Review (POUR) and Post-Service Utilization Review (POUR). POUR is used to evaluate proposed services prior to their being performed, to ensure that the services are medically necessary and appropriate for the Medicaid member’s condition and diagnosis. Post-Service Utilization Review is used to evaluate services after they have been performed, to ensure that the services were appropriate, effective, and medically necessary.
Kentucky Managed-Care Utilization Review
Description
How to fill out Kentucky Managed-Care Utilization Review?
US Legal Forms is the most easy and cost-effective way to find appropriate formal templates. It’s the most extensive online library of business and individual legal documentation drafted and checked by attorneys. Here, you can find printable and fillable blanks that comply with federal and local laws - just like your Kentucky Managed-Care Utilization Review.
Getting your template requires just a couple of simple steps. Users that already have an account with a valid subscription only need to log in to the website and download the form on their device. Later, they can find it in their profile in the My Forms tab.
And here’s how you can get a properly drafted Kentucky Managed-Care Utilization Review if you are using US Legal Forms for the first time:
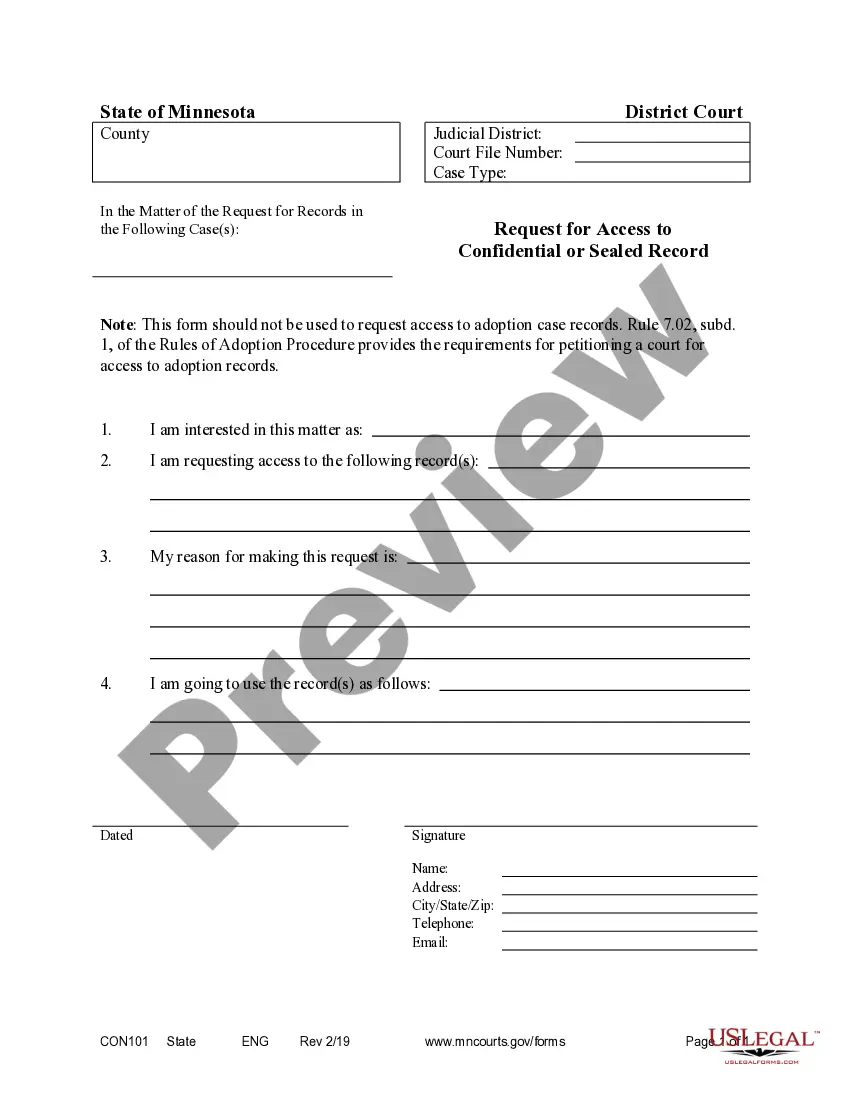
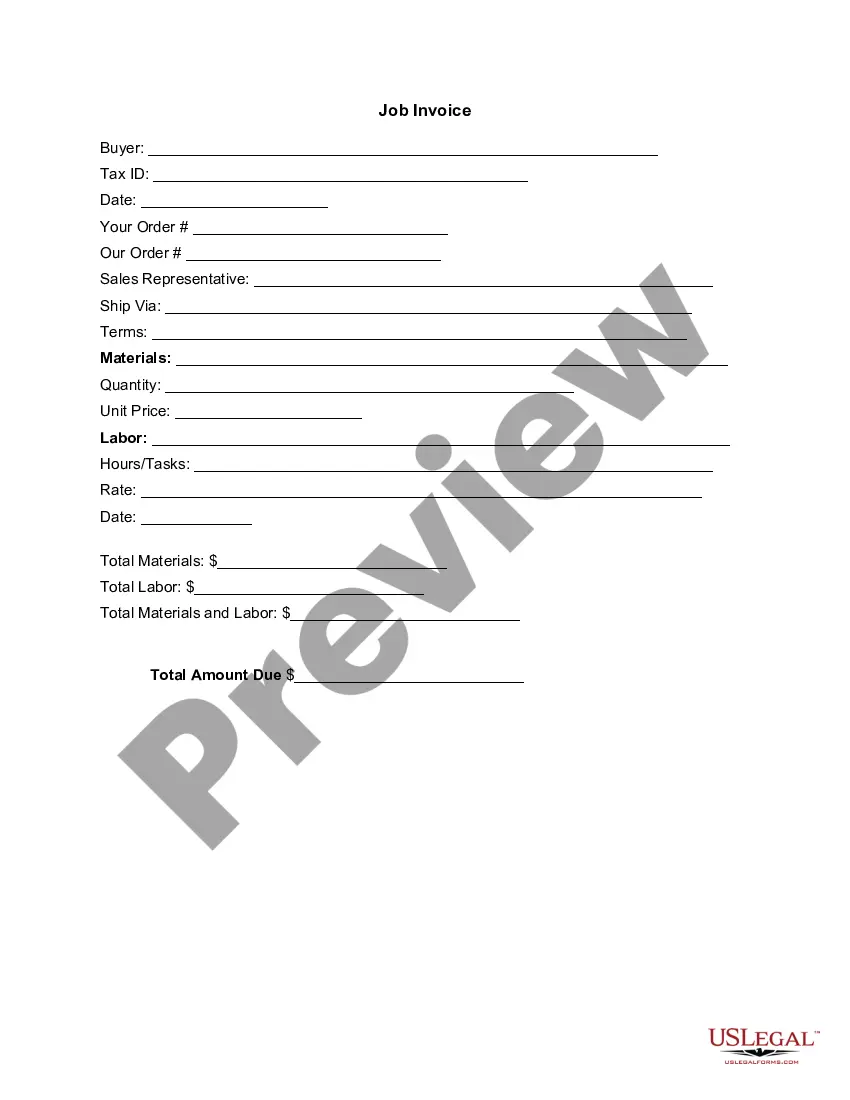
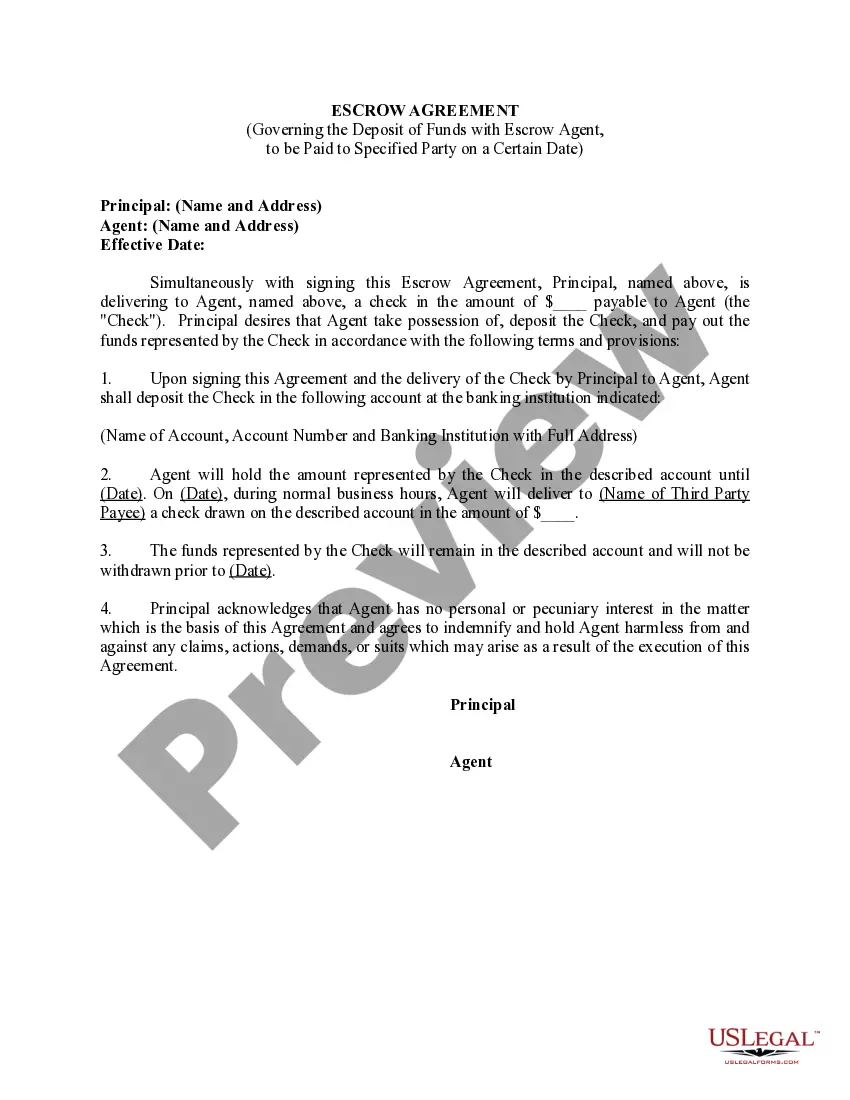
- Read the form description or preview the document to ensure you’ve found the one meeting your demands, or find another one using the search tab above.
- Click Buy now when you’re certain about its compatibility with all the requirements, and choose the subscription plan you like most.
- Register for an account with our service, sign in, and purchase your subscription using PayPal or you credit card.
- Select the preferred file format for your Kentucky Managed-Care Utilization Review and download it on your device with the appropriate button.
Once you save a template, you can reaccess it whenever you want - simply find it in your profile, re-download it for printing and manual completion or import it to an online editor to fill it out and sign more proficiently.
Benefit from US Legal Forms, your reliable assistant in obtaining the required official paperwork. Give it a try!
Form popularity
FAQ
Utilization review coordinators and mds coordinators both include similar skills like "patients," "patient care," and "discharge planning" on their resumes. While some skills are similar in these professions, other skills aren't so similar.
Other examples of utilization reviews might include determining whether or not a patient should be transferred to a specialty trauma ICU at a regional center or getting insurance approval for an extended hospital stay that goes beyond the typical guidelines.
There are three types of utilization reviews: Prospective review: determines whether services or scheduled procedures are medically necessary before admission. Concurrent review: evaluates medical necessity decisions during hospitalization. Retrospective review: examines coverage after treatment.
There are three activities within the utilization review process: prospective, concurrent and retrospective.
What Is Utilization Management in Healthcare? Utilization management (UM) is a process that evaluates the efficiency, appropriateness, and medical necessity of the treatments, services, procedures, and facilities provided to patients on a case-by-case basis.
The goal of utilization review is to make sure patients get the care they need, that it's administered via proven methods, provided by an appropriate healthcare provider, and delivered in an appropriate setting.
Types of Utilization Management Preadmission Certification. Admission Certification. Continued Stay/Concurrent Review. Retrospective Review. Second Surgical Options. Discharge Planning Review. Pharmacy Therapy Management. Review for Referral to Case Management.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.